Abstract
Objective:
This study aims to estimate the current and future burden of cardiovascular diseases (CVD) in Turkey.
Methods:
A burden-of-disease model was developed that included inputs on population growth, prevalence, and incidence of ischemic disease (IHD) and cerebrovascular disease (CeVD), prevalence of modifiable risk factors, mortality rates, and relationship between risk factors and IHD/CeVD. Direct costs to the public health-care system and indirect costs from lost production due to premature mortality, hospitalizations, disability, and absenteeism were considered.
Results:
We estimated that in 2016, 3.4 million Turkish adults were living with CVD, including 2.5 million affected by IHD, and 0.9 million by CeVD. This prevalence is projected to increase to 5.4 million by 2035. The economic burden of CVD was estimated at US$10.2 billion in 2016, projected to increase twofold to US$19.4 billion by 2035.
Conclusion:
Our study confirms that the current burden of CVD is significant, and that it is projected to increase at a steep rate over the next two decades. This growing burden of disease will likely create significant pressure on the public health-care system in the form of direct health-care costs, as well as on society in the form of lost productivity.
Keywords: cardiovascular diseases, heart diseases, risk factors, cost of illness, health expenditures, public health
Introduction
According to the World Health Organization (WHO), cardiovascular diseases (CVD) are the leading cause of death globally, and were responsible for over 17 million deaths (about 31% of all deaths) in 2012. By 2030, CVD are projected to account for approximately 23.6 million deaths annually worldwide, surpassing by a huge margin the global burden of infectious diseases, nutritional disorders, and maternal conditions combined (1).
In 2010, ischemic heart disease (IHD) and cerebrovascular disease (CeVD) were reported as the first and second leading causes of premature deaths in Turkey. Each was responsible for estimated 1.8 million and 1.2 million years of life lost (YLL) (2). Still, mortality rates from IHD and CeVD have been consistently declining since 1994 and 2004, respectively (3). In addition, CVD are among the leading causes of lost disability-adjusted life years (DALYs), with IHD accounting for 2160 lost DALYs per year, and CeVD for 976 DALYs (4).
Like other countries in the region and across the world, Turkey’s population of approximately 80 million is aging, caused in part by steadily decreasing mortality and fertility (5, 6). In addition, positive changes in availability of primary health care, economic growth, and immunization rates have contributed to an epidemiological shift from communicable diseases and nutritional deficiencies toward noncommunicable diseases such as CVD (7, 8).
The rising prevalence of modifiable risk factors is also intimately linked to the growing burden of chronic diseases, including CVD. For example, several studies have reported high rates of overweight and obesity, low physical activity, hypertension, dyslipidemia, and type 2 diabetes in the Turkish population (9-11). Inversely, epidemiological research has shown that CVD events are preventable through the modification, elimination, or avoidance of one or several of these risk factors. For example, declining rates of CVD in some high-income countries have been attributed to population-wide prevention initiatives, and access to effective medical and pharmacological interventions (12).
Planning and implementing effective public policies to achieve these improvements relies on access to reliable and up-to-date information on the prevalence and economic burden of CVD in Turkey. To meet this need, this study (Part 1) estimates the prevalence, mortality, and economic burden of CVD, and forecasts the results out to 2035. A linked study (Part 2) estimates the health and economic impact of addressing modifiable risk factors for CVD.
Methods
The Conference Board of Canada developed an additive burden of illness model that projects the prevalence and economic burden of CVD in Turkey out to 2035. The approach is similar to the model developed by Checkoway et al. (13) in “Research Methods in Occupational Epidemiology” as detailed later. The additive model assumes that when an individual has two or more risk factors, their increased risk (beyond the base risk) of developing IHD or stroke is the sum of the increased risks of each of the risk factors present.
Our model relies on population forecasts combined with the prevalence/incidence of CVD and modifiable risk factors, and estimated relative risks, to project the prevalence of CVD over time. Data presented in the next sections were used to create a forecast of the direct costs of treating CVD, while an indirect cost model was developed to project foregone earnings and reduced productivity due to illness.
Population model
The demographic forecast of the Turkish population is crucial to the analysis as it drives a significant portion of changes in disease prevalence over time. Population estimates and projections were obtained from the World Bank DataBank, and are based on total population and age distributions of the United Nations Population Division’s World Population Prospects (14). Population growth in Turkey appears to be relatively linear (arithmetic increase) between 2016 and 2035.
Prevalence of cardiovascular disease and risk factors
In our study, CVD is broadly defined as IHD and CeVD, and model inputs were collected for both the conditions. According to various sources, 5.8% of Turkish males and 5% of females have a history of heart disease, while 1.7% of males and 2.2% of females have a history of stroke (15, 16).
Epidemiologic research has shown that CVD are partially preventable through the modification, elimination, or avoidance of modifiable risk factors, including hyperlipidemia, arterial hypertension, type 2 diabetes mellitus, tobacco smoking, overweight and obesity, physical inactivity, and low fruit and vegetable consumption. Our model leverages prevalence rate estimates from a variety of sources, including the Chronic Diseases and Risk Factors Survey from the Ministry of Health, Ankara (see Appendix Table 1).
Table 1.
Average direct cost per case
| Hospitalization cost (US$) | Maintenance cost (US$) | Total cost (US$) | |
|---|---|---|---|
| Ischemic heart disease | $2,675 | $735 | $3,411 |
| Cerebrovascular disease | $1,678 | $352 | $2,030 |
US$: United States Dollar
Relative risk of cardiovascular disease
Estimates for the relative risk of each condition with and without a risk factor, or for different levels of exposure/intensity of a risk factor, were obtained from a review of the literature (see details in Appendix Table 2). This literature review included systematic reviews examining the relationship between various modifiable and lifestyle risk factors and chronic conditions. Where a systematic review was not available to quantify the risk factor-condition relationship, other individual studies (of mostly observational design) were included.
Mortality rates
Data on number of deaths for IHD (ICD-10 codes: I20–I25) and CeVD (ICD-10 codes: I60–I69) came from WHO’s Mortality Database (17). The case fatality rate is calculated as the number of deaths in 2013 (the most recent year for which data was available) divided by the prevalence in 2013 for each condition (see details in Appendix Table 3). In our model, the case fatality rate is assumed to remain constant over the forecast period for each age-sex group.
Estimating the base risk
In our study, the base risk is defined as the prevalence rate of a condition in the absence of any risk factor. It is important because the relative risk of each risk factor is added to the base risk in the model to forecast prevalence rates of IHD and CeVD from 2016 to 2035. The additive model used in this report is as described by Checkoway et al. (13) in “Research Methods in Occupational Epidemiology.” It implies that in the prevalence of several concurring risk factors, the relative risk is assumed to be where n is the total number of concurrent risk factors.
The additive model assumes that when an individual has two or more risk factors, his or her increased risk (beyond the base risk) of developing a chronic condition is the sum of the increased risks of each of the risk factors he or she has. For example, if smoking raises the chance of developing cancer by 10 percentage points, and lack of physical activity by 5 percentage points, then the additive model assumes that a person who both smokes and is physically inactive will have a 15 percentage-point increased risk of developing cancer. Because base risks are not documented in the literature, we estimated them using data on the prevalence of risk factors combined with relative risk estimates from the literature (see Appendix Table 4).
Forecasting the prevalence of cardiovascular disease
A forecast of the prevalence of CVD by age and sex was generated by using our base risk estimates, combined with our relative risk estimates and our population forecasts. The number of acute incident (hospitalized) cases of IHD and CeVD in Turkey was estimated by applying a Centers for Disease Control and Prevention (CDC) statistic on the proportion of individuals with IHD and CeVD who are hospitalized per year due to their condition (18, 19), to the prevalence of each condition in Turkey. This proportion of incident (hospitalized) cases is 13.4% for individuals diagnosed with IHD and 15.9% for CeVD. In our model, the prevalence rate of CVD and modifiable risk factors as well as the relative risk estimates were assumed to remain constant over the forecast period of 2015–2035.
From prevalence to economic burden estimates
A projection of the economic burden of CVD was developed by leveraging our prevalence forecasts, combined with disease cost data and CVD mortality rates.
Direct costs
Direct costs refer to costs directly related to the detection, treatment, and rehabilitation of a disease. The average cost per hospitalized case of IHD was calculated from a sample dataset of 2728 admitted cases (ICD I20–I25) to the University of Health Sciences Türkiye Yüksek İhtisas Hospital reimbursed between January and March 2016 by the Social Security Institution [Sosyal Güvenlik Kurumu (SGK)] (20). The average cost per hospitalized case of CeVD was obtained from the literature (21). An adjustment was subsequently applied to account for disease maintenance costs, estimated as a share of hospitalization costs presented in work by Hermus et al. (22). More specifically, the management costs represent the annual cost of controlling (or managing) the condition, excluding hospitalization costs. This includes visits to a family doctor, and medications needed to treat the disease that are separate from an actual visit to the hospital due to an acute event, which were estimated at 27.5% of the cost of hospitalizations for IHD and 21% for CeVD (22). In our study, prevalent non-hospitalized cases of IHD and CeVD were modeled to incur maintenance costs only (US$735 and US$352, respectively), while acute incident hospitalized cases included both the hospitalization and maintenance costs (totaling US$3411 for IHD and $2030 for CeVD) (Table 1).
The adjusted costs per case was then converted from Turkish Lira (TRY) to United States dollar (US$) using the Organisation for Economic Co-Operation and Development (OECD) purchasing power parity (PPP) adjusted exchange rate for 2014 of 1.163. The PPP is often used in international economic analyzes as an alternative to market rates, which are highly volatile and vary over time (23). The OECD also states that PPPs are much more stable, and represent exchange rates that are relative to the ratio of prices (in national currencies) for the same basket of goods or services in different countries (24). Based on expert opinion, inflation rates were not applied to the cost per case over the forecast period because the cost of health care services has remained stable in the last decade in Turkey, and is not expected to increase in the near future. The resulting economic burden of CVD in Turkey is expected to follow a linear increase as it is calculated as a function of prevalence (which increases linearly with population) multiplied by the average cost per case.
Indirect costs
Indirect costs in economic analyses are typically calculated as the value of foregone income lost due to disease. These costs can arise for several reasons, and in our model, they include costs from premature mortality, early retirement, and hospitalizations. To calculate the foregone earnings from CVD over patients’ lifetime, the human capital approach was used, we and leveraged existing data and estimates from the literature (25-28). The value of time lost from work is measured by foregone earnings calculated as average earnings, adjusted by the participation rate and unemployment rate, over the relevant period within the working life of an individual from ages 15 to 65 years inclusive (see Appendix Table 5 for more details).
Results
Prevalence and incidence of cardiovascular disease
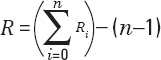
We estimated that in 2016, 3.4 million Turks were living with CVD, including 2.5 million individuals affected by IHD and 0.9 million by CeVD. Out of this prevalence, the number of acute incident (hospitalized) cases in 2016 was estimated at 324.242 for IHD and 141.359 for CeVD. The prevalence of CVD is projected to increase to 4.2 million adults by 2025, and to 5.4 million by 2035, which represents a 26.0% and 58.1% growth in prevalence respectively compared to 2016 (Fig. 1). This increase is anticipated to be driven by both IHD and CeVD, although the later condition will grow at a greater pace than the former (67.1% vs. 54.7% between 2016 and 2035). Within this broader prevalence, the number of incident cases is expected to increase at a similar rate, reaching 516,473 new cases of IHD and 244.043 new cases of CeVD by 2035.
Figure 1.
Prevalence of cardiovascular disease by year, 2016-2035
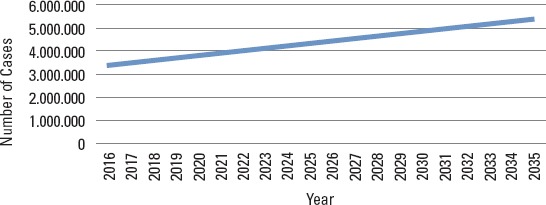
In 2016, more than half of the overall prevalence of CVD was found to occur between the ages of 55-74 years (55.5%), followed by 35-54 years (31.1%). A smaller proportion of cases were expected for the older age group of 75 years and above (10.1%), and even fewer for the 25-34 age group (3.3%). By 2035, the growing prevalence of CVD will be proportionately accompanied by more cases of heart disease and stroke occurring in older age groups. For example, 14.2% of CVD cases are projected to occur in adults aged 75 years and above by 2035, which represents a 40.3% increase compared to 2016. Inversely, adults aged 35-54 years old will represent a diminishing proportion of affected individuals (Fig. 2).
Figure 2.
Distribution of cardiovascular disease prevalence by age group and year
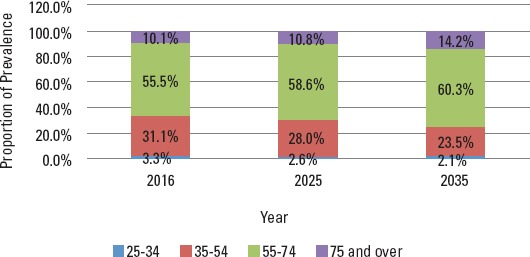
Cardiovascular disease mortality
We estimated that 100,430 deaths were due to CVD in 2016, with 60,963 deaths attributable to IHD and 39,468 to CeVD. By 2035, the number of deaths is expected to nearly double to 194,702, with CeVD deaths increasing at a slightly steeper rate compared to that of IHD, with 78,131 and 116,572 deaths, respectively. In 2016, the majority of deaths were expected to occur in the older age group of 75 years and above, followed closely by adults aged 55-74 years old (56.0% and 35.6%, respectively). It is also expected that the 75 and older age group will experience a steeper increase in the number of CVD deaths over time (Fig. 3).
Figure 3.
Cardiovascular disease mortality by age group and year, 2016-2035
The economic burden of cardiovascular disease
In 2016, the economic burden of CVD in Turkey, including direct health-care costs and indirect costs from lost productivity, was estimated at US$10.2 billion. Most of this burden (US$5.9 billion) was associated with IHD, while CeVD costs were estimated at US$4.2 billion. Direct health-care costs, estimated at US$3.4 billion in 2016, were responsible for one-third of the overall economic burden of CVD, while indirect costs made up the other two-thirds at US$6.8 billion. The burden of CVD in Turkey is projected to increase by 40% by 2025, reaching US$14.2 billion. By 2035, direct and indirect costs are expected to total US$19.4 billion, nearly doubling since 2016. Furthermore, direct costs are forecast to grow at a slower rate than indirect costs, reaching US$5.4 billion and US$13.9 billion respectively by the end of the forecast period (Fig. 4).
Figure 4.
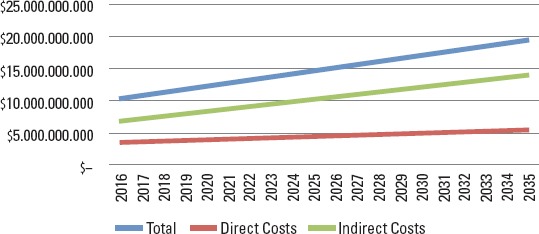
Economic burden of cardiovascular disease, 2016-2035
Discussion
Using a burden-of-disease model, we estimated the current and future burden of CVD in Turkey. The economic burden is approached from two perspectives: the first is the impact on the public health-care system (direct costs), and the second is the impact on society from lost productivity (indirect costs). We projected that the prevalence of CVD would grow from 3.4 million in 2016 to 5.3 million cases by 2035, while the economic burden would almost double from US$10.2 billion to US$19.4 billion. This increase is largely driven by demographic changes and more specifically by the anticipated aging of the Turkish population over the next 20 years, which is expected to shift the proportion of CVD cases even more toward older age groups.
Our results complement the existing literature on the burden of disease in Turkey, which shows that CVD are one of the most important causes of premature mortality and disability in the country (2, 4, 29). According to the WHO data, IHD and CeVD are among the main causes of DALYs, contributing to 2160 and 976 lost DALYs, respectively (4). In 2003, it was estimated IHD cost the European economy 49 billion a year, which corresponded to around 2.6% of total health-care expenditure (30). Although our study did not compare the burden of CVD with other conditions, it reaffirms that CVD is of concern in Turkey, and will increase at a steep rate over the next 20 years.
The growing burden of CVD projected in our study is also indirectly aligned with the observation that Turkey is experiencing a major epidemiological transition where the main causes of mortality are shifting away from infectious diseases and nutritional deficiencies toward noncommunicable diseases (31). Along with improvements in the health-care system, other factors are influencing this shift. For example, urbanization is leading to important lifestyle changes related to diet and sedentary behavior. Rising immunization rates, improved sanitation, and economic growth are also contributing to the shift toward chronic and noncommunicable diseases (31).
Turkey’s epidemiological transition is also contributing to important demographic changes, characterized by an increasingly greater distribution of the population represented in older age groups. Indeed, population projections from the World Bank DataBank show the country’s population will age significantly within the next two decades (14). The share of adults aged 65 years and above is expected to almost double from 7.5% in 2015 to 13.9% in 2035. Likewise, the share of adults aged between 50 and 64 years will increase from 13.5% in 2015 to 18.3% in 2035.
We believe this demographic shift toward an older age pyramid is largely responsible for the projected increase in CVD burden over time reported in our study. As the population continues to increase and age over the next two decades, so will the prevalence, deaths, and costs associated with CVD. This growing burden of disease will likely create significant pressure on the public health-care system in the form of direct health-care costs, as well as on society in the form of lost productivity.
Indeed, the composition and financing structure of health-care systems largely impact the burden chronic diseases place on governments, private insurers, and individuals. The Turkish national health-care system is comprised of a mix of public and private institutions. Universal coverage is provided under the Universal Health Insurance (Genel Sağlık Sigortası) system, which insures individuals registered with the Social Security Institution (Sosyal Güvenlik Kurumu). The state of the health-care system in Turkey has improved in recent years due to changes implemented as part of the Health Transformation Program (HTP), which tackled legislative, governance, efficiency, and quality improvements (32).
In light of the projected growing burden of CVD in the next 20 years, the Turkish government has interest in increasing public health efforts to address the most important modifiable risk factors, including hypertension, dyslipidemia, tobacco smoking, type 2 diabetes, obesity, and overweight. This is especially important in the context of Turkey’s economic development, which could lead to inflation of the cost of health-care services, and further contribute to the growing economic burden of CVD incurred by government. By adding to the knowledge base on the current and future burden of CVD in Turkey, we hope our study will contribute to the movement toward greater public health efforts and increased access to effective treatments to address modifiable risk factors.
Study limitations
Our study makes use of the best available information to forecast the prevalence and economic burden of CVD in Turkey. While every effort was made to maximize the accuracy of these forecasts, certain limitations in the data sources and modeling assumptions are worth noting. New estimates of the average cost per case of IHD and CeVD hospitalizations recently became available. These new cost figures are slightly higher than the ones used in our model; therefore, we may be underestimating the true economic burden of CVD in Turkey. Furthermore, assumptions on the share of hospitalized and non-hospitalized cases were used to derive CVD incidence from the overall prevalence of the condition.
In terms of our modeling approach, we used an additive model that assumed an increased risk of CVD for every risk factor present in the population. This could lead to an overestimation of the true overall risk in the event that specific risk factors moderate one another when present in combination. An alternative to the additive model is the multiplicative model, which is mostly used in studies where risk factors are believed to act as effect modifiers for the relationship between another risk factor and the risk of the condition. Multiplicative models are believed to be more relevant in disease etiology studies, while additive models are most often used (and are also easier to interpret) when quantifying the impact of public health measures to reduce disease frequency (33).
In our study, the prevalence of risk factors is assumed to remain constant over the forecast period, although the longitudinal Turkey Adult Risk Factor Study (TEKHARF) could have been used to derive historical data on risk factor progression in Turkey (34). For example, some risk factors such as obesity and diabetes may see an increase in the future, which would impact the projected prevalence of CVD over the forecast period. Inversely, some risk factors such as tobacco smoking may see a decrease in future years, which could lessen the burden of CVD in Turkey. Lastly, our indirect cost model was limited to costs due to premature mortality, early retirement, and hospitalizations, and did not consider other costs such as payments made by the Social Security Institution to relatives of severely disabled patients after a Rankin 4 stroke episode.
Conclusion
CVD, and more specifically, IHD and CeVD are two important causes of morbidity, premature mortality, and disability in Turkey. Our study confirms that the current burden of CVD is significant, and that it is projected to increase at a steep rate over the next two decades due in large part to aging of the population. This growing burden of disease will likely create significant pressure on the public health-care system in the form of direct health-care costs, as well as on society in the form of lost productivity. Efforts to address the key modifiable risk factors for CVD and to increase access to effective treatment are therefore essential to ensure the sustainability of the Turkish health-care system over time.
Footnotes
Financial support: This work was supported by research funding from Amgen, Inc, Thousand Oaks, CA.
Declaration of interests: Mohdhar Habib, Guillermo Villa and Gülnihal Ertuğrul are employees of Amgen and hold Amgen stock. Simten Malhan has worked as consultant for Amgen. Yücel Balbay has worked as consultant for Amgen, Sanofi and Bayer. Mehmet Ergun Öksüz, Isabelle Gagnon-Arpin, Greg Sutherland and Alexandru Dobrescu have no conflict of interest to declare.
Peer-review: Externally peer-reviewed.
Authorship contributions: Concept – I.G.A., M.H.; Design – Y.B., S.M., M.E.Ö., G.V.; Supervision – I.G.A., M.H.; Materials – None; Data collection &/or processing – Y.B., S.M., M.E.Ö., G.E.; Analysis &/or interpretation – G.S., A.D.; Literature search – I.G.A., G.S., A.D.; Writing – I.G.A., G.S., A.D., G.V., G.E., M.H.; Critical review – Y.B., I.G.A., S.M., M.E.Ö., G.S., A.D., G.V., G.E., M.H.
References
- 1.World Health Organization. Cardiovascular Diseases. 2015. [Accessed February 22, 2016]. http://www.who.int/cardiovascular_diseases/en/
- 2.Institute for Health Metrics and Evaluation. Turkey: GBD Profile; 2010. [Google Scholar]
- 3.Dinç G, Sözmen K, Gerçeklioğlu G, Arık H, Critchley J, Unal B. Decreasing trends in cardiovascular mortality in Turkey between 1988 and 2008. BMC Public Health. 2013;13:896. doi: 10.1186/1471-2458-13-896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Estimated DALYs ('000) by cause, sex and WHO Member State. [Accessed August 30, 2017]. http://www.who.int/healthinfo/global_burden_disease/estimates/en/index2.html .
- 5.The World Bank. [Accessed August 30, 2017];Death rate, crude (per 1,000 people) http://data.worldbank.org/indicator/SP.DYN.CDRT.IN?locations=TR . [Google Scholar]
- 6.D'Addato AV, Vignoli V, Yavuz S. Towards smaller family size in Egypt, Morocco and Turkey:overall change over time or socio-economic compositional effect? Rostock. 2007 [Google Scholar]
- 7.Carter S, Taylor D, Kanavos P, Grimaccia F, Tordrup D, Tatar M. Transforming Health in Turkey:21st Century Opportunities. UCL School of Pharmacy. 2012:1–23. [Google Scholar]
- 8.Sozmen K, Unal B. Socioeconomic Inequalities in Non-Communicable Diseases and Self Assessed Health in Turkey. Iran J Public Health. 2014;43:736–48. [PMC free article] [PubMed] [Google Scholar]
- 9.Ünal B, Ergör G, DinçHorasan G, Kalaça S, Sözmen K. Chronic Diseases and Risk Factors Survey in Turkey. Ankara: Anıl Matbaa Ltd. Şti; 2013. pp. 69–89. [Google Scholar]
- 10.Arıcı M, Birdane A, Güler K, Yıldız BO, Altun B, Ertürk S, et al. Turkish Hypertension Consensus Report. Turk Kardiyol Dern Ars. 2015;43:402–9. doi: 10.5543/tkda.2015.16243. [DOI] [PubMed] [Google Scholar]
- 11.Satman I. TURDEP-II Sonuçları. 2011 [Google Scholar]
- 12.Institute of Medicine. Promoting Cardiovascular Health in the Developing World:A Critical Challenge to Achieve Global Health. Washington, DC: The National Academies Press; 2010. [PubMed] [Google Scholar]
- 13.Checkoway H, Pearce N, Kriebel D. Research Methods in Occupational Epidemiology. New York: Oxford University Press; 2004. [Google Scholar]
- 14.The World Bank. Health Nutrition and Population Statistics:Population estimates and projections. [Accessed July 15, 2016]. http://databank.worldbank.org/data/reports.aspx?source=Health%20Nutrition%20and%20Population%20Statistics:%20Population%20estimates%20and%20projections .
- 15.Onat A, Senocak MS, Surdum-Avci G, Ornek E. Prevalence of coronary heart disease in Turkish adults. Int J Cardiol. 1993;39:23–31. doi: 10.1016/0167-5273(93)90293-p. [DOI] [PubMed] [Google Scholar]
- 16.Ozturk Y, Demir C, Gursoy K, Koselerli R. Analysis of Stroke Statistics In Turkey. ISPOR 18th Annual European Congress Research Abstracts Research Abstracts. 2015;18:A402. [Google Scholar]
- 17.World Health Organization. [Accessed July 15, 2016];WHO Mortality Database. 2015 http://www.who.int/healthinfo/mortality_data/en/ [Google Scholar]
- 18.Centers for Disease Control and Prevention. Heart Disease. 2016. [Accessed July 8, 2016]. http://www.cdc.gov/nchs/fastats/heart-disease.htm .
- 19.Centers for Disease Control and Prevention. [Accessed July 8, 2016];Cerebrovascular Disease and Stroke. 2016 http://www.cdc.gov/nchs/fastats/stroke.htm . [Google Scholar]
- 20.Data from the billing system of the University of Health Scienes Türkiye Yüksek Ihtisas Hospital. 2016 [Google Scholar]
- 21.Asil T, Celik Y, Sut N, Celik AD, Balci K, Yilmaz A, et al. Cost of acute ischemic and hemorrhagic stroke in Turkey. Clin Neurol Neurosurg. 2011;113:111–4. doi: 10.1016/j.clineuro.2010.09.014. [DOI] [PubMed] [Google Scholar]
- 22.Hermus G, Stonebridge C, Dinh T, Didic S, Theriault L. Reducing the Health Care and Societal Costs of Disease:The Role of Pharmaceuticals. The Conference Board of Canada. 2013;105 [Google Scholar]
- 23.Gosden TB, Torgerson DJ. Economics notes:Converting international cost effectiveness data to UK prices. BMJ. 2002;325:275–6. doi: 10.1136/bmj.325.7358.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.OECD. PPPs and Exchange Rate. 2016. [Accessed September 18, 2016]. http://stats.oecd.org/Index.aspx?DataSetCode=SNA_TABLE4 .
- 25.Euromonitor International. Euromonitor Country Profile. [Accessed August 4, 2016]. http://www.euromonitor.com/
- 26.The World Bank. World Development Indicators. 2016. [Accessed September 12, 2016]. http://data.worldbank.org/products/wdi .
- 27.Sözmen K, Pekel Ö, Yılmaz TS, Şahan C, Ceylan A, Güler E, et al. Determinants of inpatient costs of angina pectoris, myocardial infarction, and heart failure in a university hospital setting in Turkey. Anatol J Cardiol. 2015;15:325–33. doi: 10.5152/akd.2014.5320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Harbers MM, Achterberg PW National Institute for Public Health and the Environment. Europeans of retirement age:chronic diseases and economic activity. RIVM, December 2012 [Google Scholar]
- 29.The Ministry of Health of Turkey. Turkey Burden of Disease Study. Ankara, Turkey: The Ministry of Health of Turkey, editor; 2004. [Google Scholar]
- 30.Tasçı C, Özçelik N. An Overview on Coronary Heart Disease (A Comparative Evaluation of Turkey and Europe) and Cost-effectiveness of Diagnostic Strategies. Mol Imaging Radionucl Ther. 2011;20:75–93. doi: 10.4274/MIRT.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Marinho FM, Soliz P, Gawryszewski V, Gerger A. Epidemiological transition in the Americas:changes and inequalities. The Lancet. 2013;381:S89. [Google Scholar]
- 32.World Health Organization. Country Cooperation Strategy At A Glance-Turkey. 2013 [Google Scholar]
- 33.Penn State Eberly College of Science. 12.5 - An Extension of Effect Modification - Additive vs Multiplicative Effect Modification. 2017. [Accessed September 12, 2017]. https://onlinecourses.science.psu.edu/stat507/node/86 .
- 34.Institute for Health Metrics and Evaluation. Turkey Adult Risk Factor Study 2008. 2017. [Accessed April 19, 2018]. http://ghdx.healthdata.org/record/turkey-adult-risk-factor-study-2008 .


