Abstract
Over the past decades, management of rheumatic diseases improved both due to development of new drugs and to new imaging techniques. Objective: The aim of this study was to evaluate the type and frequency of different structures involvement in the hand of patients with rheumatoid arthritis, psoriatic arthritis and gout compared to patients with osteoarthritis of the hand Methods: We designed an observational, transverse study, which included 110 consecutive patients evaluated in the Rheumatology Department, Emergency County Hospital Craiova, during one year 2014-2015, from which 50 were diagnosed with rheumatoid arthritis, 20 with psoriatic arthritis, 20 with gout and 20 with osteoarthritis. All patients uderwent clinical, biological and US examination. Results: The global prevalence showed any US abnormalities at the hand level in 47 (94%) RA patients with respect to 17 (85%) patients in PsA group, 15 (75%) patients with gout and 12 (60%) patients in OA group (p=0.01) (Table 1). In all groups, except PsA patients, the tendon involvement (Figure 3a,b) was present in less than 30% of the patients, the high global prevalence being explained by the joint involvement (Figure 3c,d). In most of the patients with tendon involvement, we found joint involvement too. Conclusions: In conclusion, although further studies are needed, with more patients and more homogenous population, the study reveals some US involvement pattern depending on the patient’s disease.
Keywords: ultrasonography, rheumatoid arthritis, psoriatic arthritis, gout, synovitis
Introduction
Over the past decades, the management of rheumatic diseases improved significantly, due to the development of new drugs and to new imaging techniques. There were defined new strategies for diagnosting and monitoring patients, with targeted treatment and tight control, which make necessary an accurate evaluation of the patients. In rheumatoid arthritis, both new diagnostic and remission criteria suggest that ultrasonography (US) might be used for additional information and that it might add value to clinical examination [1,2]. Often, in all inflammatory arthritis patients in clinical remission, US is able to depict joint subclinical inflammation. For this, we should be able to select the structures to evaluate, considering the different pattern involvement in rheumatic diseases.
The aim of this study was to evaluate the type and frequency of different structures involvement in the hand of patients with rheumatoid arthritis, psoriatic arthritis and gout compared to patients with osteoarthritis of the hand.
Patients and methods
We designed an observational, transverse study, which included 110 consecutive patients evaluated in the Rheumatology Department, Emergency County Hospital Craiova, during one year 2014-2015, from which 50 were diagnosed with rheumatoid arthritis, 20 with psoriatic arthritis, 20 with gout and 20 with osteoarthritis, according to current classification or diagnostic criteria [3,4,5,6,7]. All patients uderwent clinical, biological and US examination, after informed consent was obtained. The study was conducted according to the Declaration of Helsinki and local regulations. Approval for the study was obtained from the local ethics committee.
Clinical examination was performed by an experienced rheumatologist, and laboratory data including erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), rheumatoid factor (RF) and anticitrullinated protein antibodies (ACPA) were obtained.
US examination was performed from the first to fifth metacarpophalangeal (MCP) and proximal interphalangeal (PIP) joints, but included radiocubitocarpal (RCC) joint and flexor (flexor digitorum, flexor pollicis longus, flexor carpi ulnaris and flexor carpi radialis) and extensor (abductor pollicis longus, extensor pollicis brevis, extensor carpi radialis longus, extensor carpi radialis brevis, extensor pollicis longus, extensor digitorum and index, extensor of the fifth finger, extensor carpi ulnaris) tendons too. The US examination was performed using a MyLab 25 machine (Esaote SpA, Genoa, Italy) with a 10-18 MHz frequency linear probe according to the EULAR guidelines [8,9], and the following abnormalities were recorded in all groups: synovitis, tenosynovitis. All US examinations were performed by an experienced sonographer, blinded to clinical and laboratory data and we noted greyscale (GS) findings that indicated joint or tendon inflammation, assessed in terms of presence/absence according to the OMERACT definitions [10]. The semiquantitative evaluation of the joints described scoring systems for joint inflammation [11]: score 0=absence of US findings indicative of joint inflammation; score 0=absence of synovitis, score 1=mild hypoechoic synovial thickening, up to margins of the bones; score 2=moderate hypoechoic synovial thickening, over one side of the joint; score 3=marked hypoechoic synovial thickening, over both borders of the joint.
Statistical analysis
Statistical analyses were performed with the software program Excel, Microsoft Office. All data were expressed as the mean±standard deviations (SD) unless specified otherwise. Simple correlations were estimated by Pearson’s correlation coefficient. The Mann Whitney test was used to calculate statistically significant difference between joints, in terms of GS findings. We considered p<0.05 as statistically significant.
Results
A total of 220 hands were assesed, 100 in RA patients, 40 in each APs, gout and OA. The mean±SD for age was 50.91±13.55 years in RA, 49.8±10.73 years in APs, 59.5±8.37 years in gout and 69.5±8.08 years in OA (Fig.1).
Figure 1.
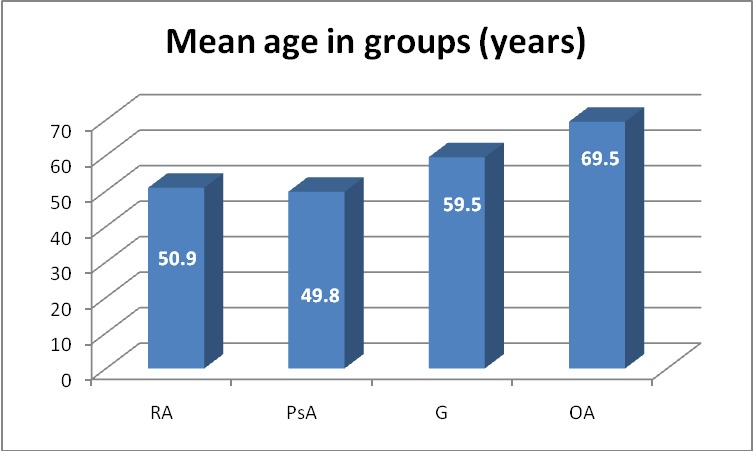
Mean age in groups
The distribution in terms of sex is shown in Fig.2, with a high predominance of the females.
Figure 2.
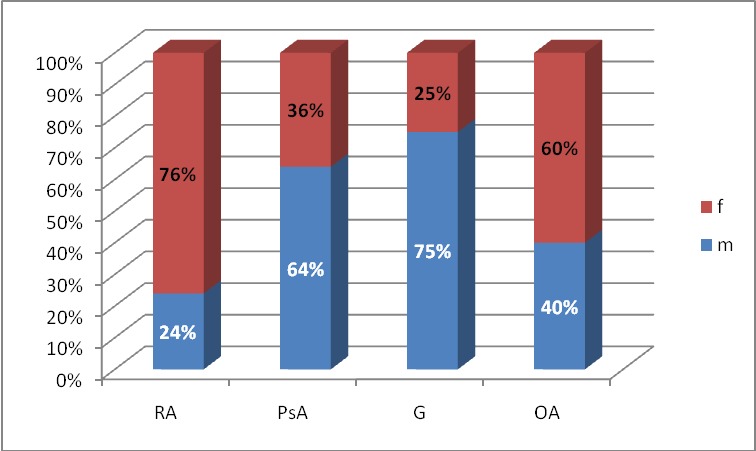
Distribution in terms of sex in all groups (RA-rheumatoid arthritis, PsA- psoriatic arthritis, G-gout, OA-osteoarthritis)
The global prevalence showed any US abnormalities at the hand level in 47 (94%) RA patients with respect to 17 (85%) patients in PsA group, 15 (75%) patients with gout and 12 (60%) patients in OA group (p=0.01) (Table 1). In all groups, except PsA patients, the tendon involvement (Fig.3a, b) was present in less than 30% of the patients, the high global prevalence being explained by the joint involvement (Fig.3c, d). In most of the patients with tendon involvement, we found joint involvement too.
Table 1.
Percentage of US abdormalities in all groups
| Any US abnorm | At least one joint abnorm | At least one tendon abnorm | |
| RA | 94% | 90% | 24% |
| PsA | 85% | 80% | 50% |
| Gout | 75% | 75% | 5% |
| OA | 60% | 55% | 20% |
Figure 3.
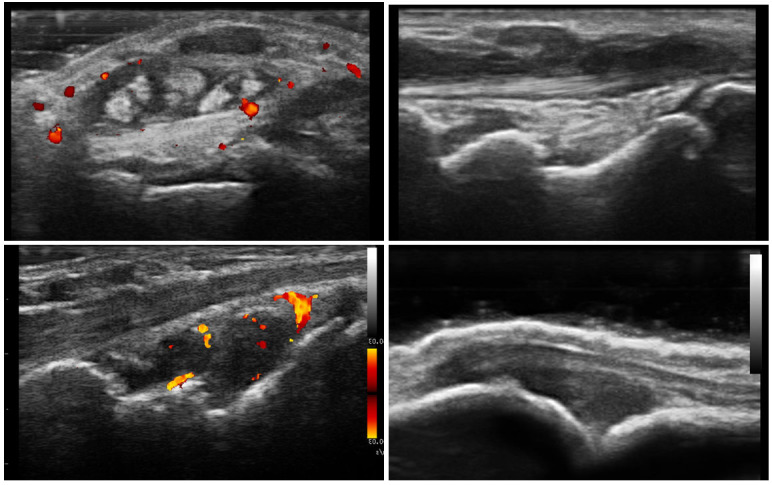
Tenosynovitis of the forth compartment of extensor tendons, transverse (a) and longitudinal (b) view; Synovitis grade III of the wrist in longitudinal view(c), Synovitis grade III of the MCP joint in longitudinal view(d)
The high prevalence of tendon involvement in OA patients, comparable to RA patients, can be explained by mechanic injury due to repetitive movements, like in De Quervain tenosynovitis.
The most frequent US abnormality in RA patients was RCC synovitis (38/50) (76%), followed by MCP synovitis (23/50) (46%) and extensor tendons involvement (9/50) (18%). (Figure 3). In the psoriatic arthritis population, the most frequent abnormality was RCC synovitis (15/20) (75%), followed by extensor tendons involvement (9/20) (45%) and MCP synovitis (6/20) (30%) (Figure 3). The analysis of gouty patients population showed RCC synovitis (12/20) (60%) as the most frequent abnormality, followed by MCP synovitis (4/20) (20%) and extensor tendons involvement (1/20) (5%). The OA group presented with the same prevalence in RCC and MCP joints (6/20) (30%) (Fig.4).
Figure 4.
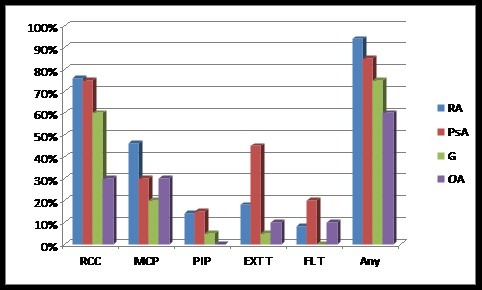
US abnormalities on different sites by groups (RCC-Wrist, MCP-metacarpophalangeal joint, PIP-proximal interphalangeal joint, EXT T-extensor tendons, FL T-flexor tendons, Any-any US abnormality).
As a greyscale (GS), in RA we found statistic significant higher scores, compared to PsA (p<0.05) and OA (p<0.05) and higher than in gouty patients, without being statistic significant (p=0.36) (Fig.5). The variance of GS scores was found to be higher in the MCP joints for RA (1.85) and gouty (3.41) patients and for RA (1.54) patients in PIP joints (Fig.5).
Figure 5.
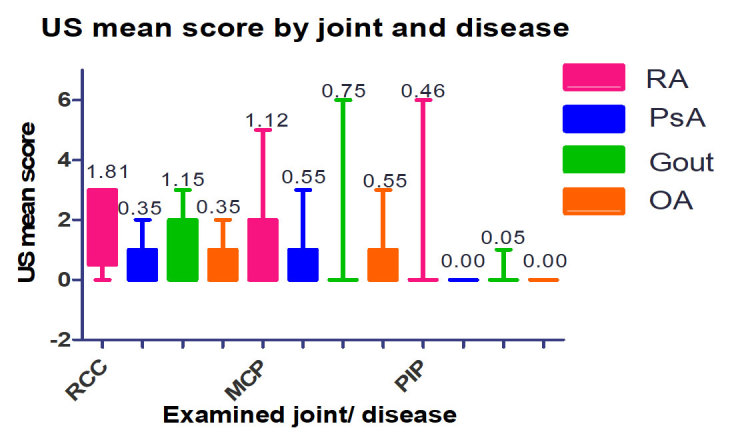
US mean score and variance by joint and disease
Discussion and conclusions
In the daily practice, scanning only the painful joints is not valid strategy, but scanning all the joints is not feasible [12], so knowing which structures are more often involved depending on the patient’s disease might have an important role in the optimal management of the patient.
Often, in all inflammatory arthritis patients in clinical remission or in the early phases, US is able to depict joint subclinical inflammation [13]. For this, we should be able to select the structures to evaluate, considering the different pattern involvement in rheumatic diseases.
The results of the study show that in RA patients we find more joint involvement of the wrists and MCP joints, but in the same time PsA patients have more tendons involvement, which is consistent with the findings in literature. We have to scan the hands of the gouty patients too, because we might find often high degree synovitis. In OA patients we might find sometimes tenosynovitis, but it is due to mechanical overuse.
One problem of the study might be the inclusion of the GS score 1, which is debatable for the purpose of discriminating arthritis patients from the non-arthritic ones. This would explain some of the joint involvement found in OA or even gouty patients. Another problem could be the groups wich are unhomogenous as a relation to disease activity and treatment.
In conclusion, although further studies are needed, with more patients and more homogenous population, the study reveals some US involvement pattern depending on the patient’s disease.
Acknowledgement
This paper was published under the frame of European Social Found, Human Resources Development Programme 2007-2013, POSDRU/159/1.5/S/136893
References
- 1.Aletaha D, Neogi T, Silman AJ, et al. 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann Rheum Dis. 2010;69:1580–1588. doi: 10.1136/ard.2010.138461. [DOI] [PubMed] [Google Scholar]
- 2.Wakefield RJ, Freeston JE, Hensor EM, Bryer D, Quinn MA, Emery P. Delay in imaging versus clinical response: a rationale for prolonged treatment with anti-tumor necrosis factor medication in early rheumatoid arthritis. Arthritis Rheum. 2007;57:1564–1567. doi: 10.1002/art.23097. [DOI] [PubMed] [Google Scholar]
- 3.Aletaha D, Neogi T, Silman AJ, et al. 2010 Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum. 2010;62:2569–2581. doi: 10.1002/art.27584. [DOI] [PubMed] [Google Scholar]
- 4.Wallace SL, Robinson H, Masi AT, et al. Preliminary criteria for the classification of the acute arthritis of primary gout. Arthritis Rheum. 1977;20:895–900. doi: 10.1002/art.1780200320. [DOI] [PubMed] [Google Scholar]
- 5.Janssens HJ, Fransen J, van de Lisdonk EH. A diagnostic rule for acute gouty arthritis in primary care without joint fluid analysis. Arch Intern Med. 2010;170:1120–1126. doi: 10.1001/archinternmed.2010.196. [DOI] [PubMed] [Google Scholar]
- 6.Pelaez-Ballestas I, Hernandez Cuevas C, Burgos-Vargas R, et al. Diagnosis of chronic gout: evaluating the American College of Rheumatology proposal, European League Against Rheumatism recommendations, and clinical judgment. J Rheumatol. 2010;37:1743–1748. doi: 10.3899/jrheum.091385. [DOI] [PubMed] [Google Scholar]
- 7.Taylor W, Gladman D, Helliwell P, Marchesoni A, Mease P, Mielants H. Classification criteria for psoriatic arthritis: development of new criteria from a large international study. Arthritis and Rheumatism. 2006;54(8):2665–2673. doi: 10.1002/art.21972. [DOI] [PubMed] [Google Scholar]
- 8.Backhaus M, Burmester GR, Gerber T, Grassi W, Machold KP, Swen WA, Wakefield RJ, Manger B. Working Group for Musculoskeletal Ultrasound in the EULAR Standing Committee on International Clinical Studies including Therapeutic Trials. Guidelines for musculoskeletal ultrasound in rheumatology. Ann Rheum Dis. 2001;60:641–649. doi: 10.1136/ard.60.7.641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Torp-Pedersen ST, Terslev L. Settings and artefacts relevant in colour/power Doppler ultrasound in rheumatology. Ann Rheum Dis. 2008;67:143–149. doi: 10.1136/ard.2007.078451. [DOI] [PubMed] [Google Scholar]
- 10.Wakefield RJ, Balint PV, Szkudlarek M, Filippucci E, Backhaus M, D'Agostino MA, Sanchez EN, Iagnocco A, Schmidt WA, Bruyn GA, Kane D, O'Connor PJ, Manger B, Joshua F, Koski J, Grassi W, Lassere MN, Swen N, Kainberger F, Klauser A, Ostergaard M, Brown AK, Machold KP, Conaghan PG; OMERACT 7 Special Interest Group. Musculoskeletal ultrasound including definitions for ultrasonographic pathology. J Rheumatol. 2005;32:2485–2487. [PubMed] [Google Scholar]
- 11.Naredo E, Bonilla G, Gamero F, Uson J, Carmona L, Laffon A. Assessment of inflammatory activity in rheumatoid arthritis: a comparative study of clinical evaluation with grey scale and power Doppler ultrasonography. Ann Rheum Dis. 2005;64(3):375–381. doi: 10.1136/ard.2004.023929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cate T, et al. Role of ultrasonography in diagnosing early rheumatoid arthritis and remission of rheumatoid arthritis-a systematic review of the literature. Arthritis Research & Therapy. 2013;15:R4–R4. doi: 10.1186/ar4132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bandinelli F, Denaro V, Prignano F, Collaku L, Ciancio G, Matucci-Cerinic M. Ultrasonographic wrist and hand abnormalities in early psoriatic arthritis patients: correlation with clinical, dermatological, serological and genetic indices. Clin Exp Rheumatol. 2015;33:330–335. [PubMed] [Google Scholar]


