Abstract
Background:
Sputum microscopy is still used for diagnosis of drug-sensitive pulmonary tuberculosis (TB). Revised National Tuberculosis Control Program (TB programs) aims to rapidly diagnose and treat all cases of TB. The aim of this study is to find the proportion of loss to follow up during diagnosis of pulmonary TB after the patient reached hospital (was handed over sputum cups for sputum collection) from DOTS center after referral from respective outpatient department (OPD) at a tertiary care hospital.
Methodology:
Record-based data from designated microscopic center at a tertiary care hospital were collected regarding the number of patients who had been given sputum cup container for sputum collection for diagnosis of pulmonary TB referred from different OPDs from January to December 2015.
Results:
A total of 1518 presumptive patient for pulmonary TB had visited DOTS center after referral from different OPDs in the hospital for sputum examination during the above period. The loss to follow-up during diagnosis among presumptive pulmonary TB patient was 461 (30.04%), which was higher among those below 15 years of age. At this rate of loss to follow up of presumptive TB patient to submit sputum for diagnosis, it was estimated to be about 46 smear-positive pulmonary TB cases per year which will be missed out for diagnosis during the above period (considering sputum positivity rate is 10% in the hospital). The mean gap between sputum referral to submission of two sputum samples was 2.73 days (95% confidence interval 2.52–2.84) among those of submitted sputum for diagnosis.
Conclusion:
Approximately one-third of presumptive patient for pulmonary TB had loss to follow-up for diagnosis of TB even after consulting a doctor at a tertiary care hospital. There is a need to address this gap in diagnosis of pulmonary TB in this region.
Keywords: Loss to follow-up, microscopy, presumptive pulmonary tuberculosis, pulmonary, tuberculosis
Introduction
Revised National Tuberculosis Control Program (RNTCP) covered the whole country since 2006, but the burden of tuberculosis (TB) is still very high in India with 2.8 million new cases detected in 2017 as per World Health Organization (WHO) TB report 2017, which is about a quarter of the world's TB cases at the rate of 211 cases per 1 lakh population.[1,2] Direct sputum microscopy by Ziehl–Neelsen acid-fast staining/fluorescence microscopy is the primary case detection tool in RNTCP for presumptive patient with drug-sensitive TB. More than 14,000 designated microscopic center (DMC) have been established under RNTCP for the diagnosis of pulmonary TB across the country.[1] Sputum smear microscopy performed by trained health workers is a reliable method for diagnosis of pulmonary TB.[3] Recently, newer diagnostic methods have been included such as Cartridge Based Nucleic Acid Amplification Test (CBNAAT) and culture and drug susceptibility testing through laboratory network under RNTCP.[1] Early case identification of individuals with sputum smear-positive TB and initiation of standard treatment are important for controlling TB.[3]
A study at primary care setting in rural Haryana estimated on average 9 days gap between diagnosis and initiation of treatment for TB.[4] In addition, a study from Uganda estimated a median of 8 weeks delay from onset of symptoms to initiation of treatment for pulmonary TB.[5] In addition, the patient has to attend multiple visits to health center/hospital before diagnosis is made for pulmonary TB in a study conducted from Peru and also from India.[6,7] Even after the patient reached the hospital and diagnosed with TB, still few of them default in starting the treatment which is called as initial default which ranges from 11.6% to 38%.[8,9,10,11,12,13] Default during diagnosis was 18.6% out of all initial default as reported from Uttarakhand.[10] One study from Pakistan reported defaults during diagnosis after submission of at least one sputum which was 12.9%.[14] There was lack of study reporting on presumptive pulmonary TB cases not reporting two sputum samples to DMC laboratory of the referral hospital. The aim of this study is to find out the proportion of presumptive pulmonary TB cases who were loss to follow up pathways after consulting the physician for submission of two sputum specimens for diagnosis of pulmonary tuberculosis.
Methodology
A record-based study was conducted at the DMC from January to December 2015 among presumptive case of pulmonary TB in a tertiary care hospital. DMC maintained one separate register for distribution of sputum cups mentioning name, age, gender, address and date of cups distribution, and date of sputum submission. All the patients who were presumptive case of pulmonary TB were referred to the DMC/DOTS center of the hospital for sputum microscopy after consulting doctors from the outpatient department (OPD). The patients were then given two sputum cup for the collection of two sputum samples (spot and morning) along with recording of patient demographic profile in a separate register. Records from the register were entered and analyzed in SPSS (IBM SPSS 22.0, Armonk, New York, USA). Descriptive analysis and Chi-square test for categorical variables were analyzes. Patient flow chart is given in Figure 1.
Figure 1.
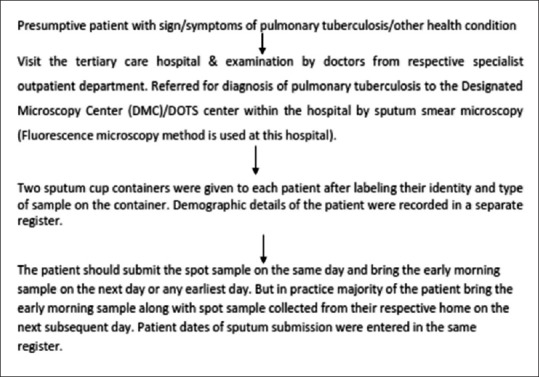
Flow chart of patient flow in diagnosis pathway of pulmonary tuberculosis
Definition of different terms used
Initial default is defined as patient with laboratory result of smear +ve pulmonary TB but not stated treatment within 7 days of diagnosis.[15] Loss to follow up during diagnosis during diagnosis in this study was defined as a presumptive patient for diagnosis pulmonary TB not submitting any sputum samples within 30 days from the date of referral for sputum examination.
Presumptive pulmonary TB is defined as a person with any of the signs and symptoms suggestive of TB including cough >2 weeks, significant weight loss, hemoptysis, and any abnormality in chest radiograph.[15]
Results
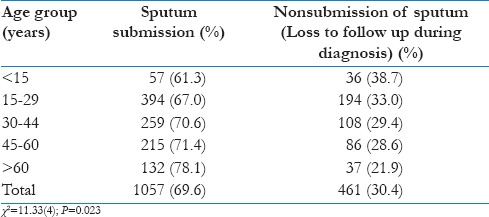
A total of 1518 presumptive patient for pulmonary TB were referred to the DMC/DOTS center for sputum examination from different OPDs in the hospital as per recorded in the register issuing sputum cup container. The majority of the patients were male (58%). The mean age of the study subject was 37.3 and 34.53 years for males and females, respectively. Of 1518, a total of 461 patients (30.4%) did not return sputum samples for testing. It was similar for both males (30%) and females (31%). Loss to follow up rate was higher among the younger (<15 years) population at 38.7% in comparison to older age group which was significantly different among the group as given in Table 1. At this rate of loss to follow up for diagnosis, it is estimated that about 46 smear-positive pulmonary TB cases may be missed for diagnosis during the above period (taking sputum positivity rate as 10% out of all suspects examined for sputum). The mean duration of sputum submission was 2.73 days for both males and females from the date of getting sputum cups (95% confidence interval 2.51–2.85 days).
Table 1.
Loss to follow up of sputum submission by age group (n=1518)
Discussion
This study found that approximately one-third of presumptive patients for pulmonary TB have not submitted two sputum samples for diagnosis which is a major problem in tackling TB where the emphasis for early detection and treatment is to be ensured. This problem may not be known in many places as there is no maintenance of a separate register for issuing of sputum cup container as reported in few of the centers in our state. Corrective measures were taken in consultation with the staff of DMC and District Tuberculosis Officer of the district to prevent further loss to sputum follow-up. Studies from other centers have shown lower report of initial default during diagnosis which is 18.6% from Uttarakhand,[10] and from Pakistan[14] it was only 12.9% where at least one sputum sample is submitted which is much lower in comparison to this study. This may depend on the study setting as this study was done at a tertiary care hospital and the patient usually attends from far areas and a good proportion of the patients (20-30%) are from outside the states. This high rate of loss to follow up during diagnosis may be due to convenient wherein the health worker at the DOTS center may asked the patient to bring early-morning sputum along with spot samples the next day after explaining them the procedure of how to cough the sputum. This may also be that the same-day sputum collections as per RNTCP guidelines[15] have not been briefed in detail to the DOTS/DMC staff and to be followed accordingly.
WHO has changed its policy, to two sputum specimens instead of three and same-day collection[16] and also recommend same-day diagnosis with two spot sputum samples since 2011, but same-day diagnosis was less sensitive (2.8%) than the conventional approach. Same-day diagnosis with two spot samples 1 h apart is shown to be possible in a study done in Rajahmundry.[17] Also a study by Murphy ME et al. showed that spot sample are similar with early morning sputum sample for diagnosis of Pulmonary TB.[18] There is delay in health-seeking behaviors for various diseases and which is also true for pulmonary TB. TB patients at times have to make multiple visits to health facilities before they were diagnosed and get treated.[19] Diagnosis and treatment of TB followed the Onion Model[20] with drop-offs at different levels from onset of symptoms to cure of the disease. Approximately 40% of the new cases may not have received healthcare and they are missed by the system.[21] WHO also encourages strategies for finding the missing cases especially in areas with high HIV infection.[22] With India aiming to eliminate TB by 2025,[23] as per the National Strategic Plan for TB elimination 2017, the RNTCP program has to take important steps so that there is no delay in diagnosis of pulmonary TB at all levels along with better sputum transport system in difficult-to-reach areas.
The limitation in this study is that we have no information on loss to follow up patients as they might have visited other hospital/nearest health centers and also not able to know the reasons for not coming back for sputum sample testing. As envisaged in RNTCP (TB program) of India, emphasis should be given for same-day spot collection of sputum's sample for the diagnosis of pulmonary TB as the patient may not able to come the next day for submission of sputum samples due to various reasons, which will minimize loss to follow up during diagnosis. A similar study may be conducted in all the DOTS/DMC centers in the district for assessment of this loss to follow-up during diagnosis of presumptive pulmonary TB so that corrective measures can be taken.
Conclusion
Approximately one-third of the patients suspected for pulmonary TB had missed for diagnosis even after consulting a doctor at a tertiary care hospital. There is a need to address this gap in diagnosis of pulmonary TB in this region, by proper documentation so that we know to track the patient efficiently by planning a full-fledge study involving few districts in the state.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
The authors thanks the State Task Force, Meghalaya, and Dr. Amad Dkhar and staff at DOTS/DMC center and Dr. M. Mawrie, District Tuberculosis Officer, for their support and cooperation.
References
- 1.Central TB Division. India TB Report 2018- Annual Status Report. Ministry of Health and Family Welfare, Government of India. 2018. [Last accessed on 2018 Aug 27]. Available from: https://tbcindia.gov.in/showfile.php?lid=3314 .
- 2.Dye C, Bassili A, Bierrenbach AL, Broekmans JF, Chadha VK, Glaziou P, et al. Measuring tuberculosis burden, trends, and the impact of control programmes. Lancet Infect Dis. 2008;8:233–43. doi: 10.1016/S1473-3099(07)70291-8. [DOI] [PubMed] [Google Scholar]
- 3.WHO. WHO | TB Diagnostics and Laboratory Strengthening – WHO Policy. World Health Organization; 2012. [Last accessed on 2018 Jun 16]. Available from: http://www.who.int/tb/laboratory/policy_diagnosis_pulmonary_tb/en/ [Google Scholar]
- 4.Kant S, Singh AK, Parmeshwaran GG, Haldar P, Malhotra S, Kaur R, et al. Delay in initiation of treatment after diagnosis of pulmonary tuberculosis in primary health care setting: Eight year cohort analysis from district Faridabad, Haryana, North India. Rural Remote Health. 2017;17:4158. doi: 10.22605/RRH4158. [DOI] [PubMed] [Google Scholar]
- 5.Sendagire I, Schim Van der Loeff M, Mubiru M, Konde-Lule J, Cobelens F. Long delays and missed opportunities in diagnosing smear-positive pulmonary tuberculosis in Kampala, Uganda: A cross-sectional study. PLoS One. 2010;5:e14459. doi: 10.1371/journal.pone.0014459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bailey SL, Roper MH, Huayta M, Trejos N, López Alarcón V, Moore DA, et al. Missed opportunities for tuberculosis diagnosis. Int J Tuberc Lung Dis. 2011;15:205–10, i. [PMC free article] [PubMed] [Google Scholar]
- 7.Chakraborty AK, Krishnamurthy MS, Shashidhara AN, Juvekar S. Missed opportunities for diagnosis of pulmonary tuberculosis: A study among rural patients seeking relief on their own under the tuberculosis programme in India. [Last accessed on 2018 Jun 16];Indian J Tuberc. 2001 48:181–92. Available from: http://www.medind.nic.in/ibr/t01/i4/ibrt01i4p181.pdf . [Google Scholar]
- 8.Pillai D, Purty AJ, Prabakaran S, Singh Z, Soundappan G, Anandan V. Initial default among tuberculosis patients diagnosed in selected medical colleges of Puducherry: Issues and possible interventions. [Last accessed on 2018 Jun 16];Int J Med Sci Public Health. 2015 4:957–60. Available from: https://www.ejmanager.com/mnstemps/67/67-1422624496.pdf . [Google Scholar]
- 9.Ministry of Health and Family Welfare. TB India Report 2018. Ministry of Health and Family Welfare. 2018. [Last accseed on 2018 Jun 16]. Available from: https://www.tbcindia.gov.in/showfile.php?lid=3314 .
- 10.Mehra D, Kaushik RM, Kaushik R, Rawat J, Kakkar R. Initial default among sputum-positive pulmonary TB patients at a referral hospital in Uttarakhand, India. Trans R Soc Trop Med Hyg. 2013;107:558–65. doi: 10.1093/trstmh/trt065. [DOI] [PubMed] [Google Scholar]
- 11.Thomas BE, Subbaraman R, Sellappan S, Suresh C, Lavanya J, Lincy S, et al. Pretreatment loss to follow-up of tuberculosis patients in Chennai, India: A cohort study with implications for health systems strengthening. BMC Infect Dis. 2018;18:142. doi: 10.1186/s12879-018-3039-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Afutu FK, Zachariah R, Hinderaker SG, Ntoah-Boadi H, Obeng EA, Bonsu FA, et al. High initial default in patients with smear-positive pulmonary tuberculosis at a regional hospital in Accra, Ghana. Trans R Soc Trop Med Hyg. 2012;106:511–13. doi: 10.1016/j.trstmh.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 13.Sai Babu B, Satyanarayana AV, Venkateshwaralu G, Ramakrishna U, Vikram P, Sahu S, et al. Initial default among diagnosed sputum smear-positive pulmonary tuberculosis patients in Andhra Pradesh, India. Int J Tuberc Lung Dis. 2008;12:1055–58. [PubMed] [Google Scholar]
- 14.Khan MS, Khan S, Godfrey-Faussett P. Default during TB diagnosis: Quantifying the problem. Trop Med Int Health. 2009;14:1437–41. doi: 10.1111/j.1365-3156.2009.02406.x. [DOI] [PubMed] [Google Scholar]
- 15.Central Tb Division. Technical Operative Guidelines (TOG) – Case Finding & Diagnosis Strategy. Ch. 3. Ministry of Health and Family Welfare, Government of India. 2016. [Last accessed on 2018 Jun 17]. Available from: https://www.tbcindia.gov.in/showfile.php?lid=3216 .
- 16.Geneva: World Health Organization; 2011. World Health Organization. Same-day Diagnosis of Tuberculosis by Microscopy: Policy Statement; p. 11. [PubMed] [Google Scholar]
- 17.Chandra TJ, Raj RS, Sharma YV. Same day sputum smear microscopy approach with modified ZN staining for the diagnosis of pulmonary tuberculosis in a microscopy centre at Rajahmundry. Indian J Med Microbiol. 2014;32:153–56. doi: 10.4103/0255-0857.129801. [DOI] [PubMed] [Google Scholar]
- 18.Murphy ME, Philips PPJ, Mendel CM, Bongard E, Bateson ALC, Hunt R, et al. Spot sputum samples are at least as good as early morning samples for identifying Mycobacterium tuberculosis. BMC Med. 2017;15:192. doi: 10.1186/s12916-017-0947-9. doi: 10.1186/s12916-017-0947-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ndubuisi NO, Chibuike OA, Esther UA, Christopher OU. Delay in diagnosis of pulmonary tuberculosis among presumptive tuberculosis cases in parts of Anambra State, Nigeria. [Last accessed on 2018 Jun 16];J Infect Dis Pathol. 2016 1:120. [Google Scholar]
- 20.Chin DP, Hanson CL. Finding the missing tuberculosis patients. J Infect Dis. 2017;216:S675–8. doi: 10.1093/infdis/jix368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Partners Launch Global Effort to Find Missing Cases of TB. [Last accessed on 2018 Jun 16]. Available from: https://www.theglobalfund.org/en/news/2017.10-09-partners-launch-global-effort-to-findmissing.cases-of-tb/
- 22.Grzemska M. Child and Adolescent TB Working Group Meeting Kigali, Rwanda Finding the Missing TB Cases Optimizing Strategies to Enhance Case Detection in High HIV Burden Settings. 2017. [Last accessed on 2018 Jun 16]. Available from: http://www.who.int/tb/areas-of-work/children/missing_childhoodtb_cases.pdf .
- 23.Central Tb Division. National Strategic Plan for Tuberculosis Elimination 2017–2025. Ministry of Health and Family Welfare, Government of India. 2016. [Last accessed on 2018 Aug 17]. Available from: https://www.tbcindia.gov.in/WriteReadData/NSP%20Draft%2020.02.2017%201.pdf .


