Abstract
Background
The notion that neutral alignment is mandatory to assure long-term durability after TKA has been based mostly on short-film studies. However, this is challenged by recent long-film studies.
Questions/purposes
We conducted this long-film study to know (1) whether the risk of aseptic revision for nontraumatic reasons was greater among knees with greater than 3° varus or valgus (defined as “outliers”) than those that were aligned within 3° of neutral on long-standing mechanical axis (hip to knee) radiographs; and (2) what the failure mechanisms were and whether the malalignment was femoral or tibial in origin, or both, among those in the outlier group.
Methods
Between November 1998 and January 2009 we performed 1299 cemented, posterior cruciate ligament-substituting TKAs in 867 patients for primary osteoarthritis. We had inadequate long-standing radiographs to analyze postoperative alignment for 124 of those knees, and an additional 24 were excluded for prespecified reasons. Consequently, 1151 knees were enrolled in our study. Of these, 982 (85%) in 661 patients (620 women and 41 men) who had followup greater than 24 months were analyzed. The knees were divided according to whether the postoperative mechanical axis was neutral (0° ± 3°), varus (> 3°), or valgus (< -3°) alignment on long-standing radiographs. The survivorships free from aseptic revision for nontraumatic reasons were compared among groups. The mechanical femoral and the tibial component alignment (MFCA and MTCA, respectively) were investigated to know the origin of overall mechanical malalignment of the outlier knees. The mean duration of followup was 8 ± 4 years (range, 2–17 years). Thirty-five knees (4%) showed aseptic loosening at 7 ± 4 years (range, 0.1–14 years) and five (1%) showed polyethylene wear at 12 ± 1 years (range, 10-13 years). Tibial loosening (73%) was the most common reason for aseptic revision followed by femoral loosening (30%). Of this cohort, 687 (70%), 250 (25%), and 45 (5%) knees had overall mechanical neutral, varus, and valgus alignment, respectively. Factors associated with the risk of aseptic revision were identified by Cox regression.
Results
The varus outliers (but not the valgus outliers) failed more often than the neutral knees (10% [25 of 250] versus 2% [13 of 687]; odds ratio [OR], 5.8, 95% CI, 2.9–11.5; p < 0.001). Ten-year survivorship free from aseptic revision was lower among varus outliers than among knees with neutral alignment (87% [95% CI, 80%–93%] versus 98% [95% CI, 97%–99%]; p = 0.001). Femoral component varus malpositioning was the main origin of the varus outliers (MFCA = 4.2° ± 2.0°; MTCA = 0.9° ± 1.7°) and was a risk factor for aseptic revision compared with neutral femoral positioning (OR, 14.0; 95% CI, 1.9–105.6; p < 0.001).
Conclusions
This long-film study corresponds to previous short-film studies for the notion that varus malalignment is associated with inferior long-term implant survivorship. Although aseptic loosening occurred most commonly on the tibial side, the primary origin of the overall varus malalignment was femoral component varus malpositioning. Aiming for neutral alignment in TKA still seems to be a reasonable strategy in clinical practice.
Level of Evidence
Level III, therapeutic study.
Introduction
It has long been thought that it is important to achieve neutral alignment in the coronal plane to maximize the survival and clinical outcomes of knee replacement implants after TKA [2, 6, 8, 9, 11, 14, 16, 19, 20, 27, 28]. However, this belief was challenged by studies reporting that varus outliers do not associate with lower implant survival [4, 10, 18, 23, 25, 30]. Interestingly, a recent systematic review [29] and a meta-analysis [15] suggested that these dissenting results may reflect the type of radiographs that are used to measure alignment. Studies based on short films of the anatomic femorotibial angle generally found that postoperative malalignment leads to higher rates of aseptic revision of the implant [2, 9, 14, 27, 28]. By contrast, most studies that used long films to measure mechanical alignment of the hip to ankle reported that postoperative malalignment did not affect TKA longevity [4, 10, 18, 20, 21, 23, 25, 30]. However, the latter studies were conducted with relatively small study populations. Therefore, it remains questionable whether implant longevity is guaranteed if mechanical malalignment is permitted.
Because studies examining the effects of malalignment, defined as deviation from the mechanical axis greater than 3o, have been inconclusive, it is unclear whether surgeons should focus on correcting malalignment and placing all knees having TKAs in neutral alignment. In addition, it is not clear whether malalignment of the tibial or femoral component is more consequential. Short-film studies suggest that varus alignment of the tibial component is a more-common cause of aseptic loosening. Moreover, the common location of loosening is also on the tibial side [2, 8]. However, considering large variations in femoral bowing that can promote inaccurate distal femoral cutting [5, 12], mechanical malalignment of the femoral component that has an extraarticular origin might be underestimated in short-film studies. To the best of our knowledge, there have been no large-scale, long-term studies that investigated the relationship between aseptic revision rate and mechanical alignment of each femoral and tibial component on long-standing radiographs. To address this issue, and to assess whether neutral alignment is needed to assure implant durability, we performed a retrospective large-scale, long-term, long film-based cohort study.
We conducted this long-film study to know (1) whether the risk of aseptic revision for nontraumatic reasons was greater among knees with greater than 3° varus or valgus (defined as “outliers”) than those that were aligned within 3° of neutral on mechanical axis radiographs; and (2) what the failure mechanisms were and whether the malalignment was femoral or tibial in origin, or both, among those in the outlier group beyond 3°.
Patients and Methods
This study was approved by our institutional review board. Between November 1998 and January 2009, we performed 1299 cemented, posterior cruciate ligament-substituting TKAs in 867 patients for primary osteoarthritis. Because the study aim was to determine whether postoperative mechanical alignment, as measured on long-standing radiographs (hip to ankle), is associated with the risk of later aseptic revision for nontraumatic mechanical failures (defined as implant loosening, polyethylene wear, or instability), the following patients were excluded: patients whose postoperative long-standing films after the index surgery were not available (n = 105); patients whose radiographs were not truly in the AP direction (n = 19) and thus were inappropriate for measuring postoperative mechanical alignment; and patients (n = 10) who had a history of osteotomy, hip arthroplasty, or extraarticular deformity that could affect their ipsilateral limb alignment. We also excluded patients (n = 14) with prosthetic joint infection or periprosthetic fractures. According to these exclusion criteria, 773 patients (1151 knees) were identified and enrolled in the study by retrospective review of our database. Of these, 118 patients (169 knees; 15%) who were lost to followup before a minimum of 24 months were excluded from the study. Consequently, 982 knees (85%) in 661 patients (620 women and 41 men) were analyzed here. The mean age of the patients at the time of surgery was 67 ± 6 years (range, 43–85 years), and the mean BMI was 27 ± 3 kg/m2 (range, 17–42 kg/m2). The mean duration of followup was 8 ± 4 years (medial, 8 years; range, 2–17 years), and seven patients (0.6%) had died during followup without undergoing revision surgery.
All TKAs were performed by a senior surgeon (SIB) using a conventional technique without computer assistance. We used only a NexGen® system (LPS or LPS-Flex system; Zimmer, Warsaw, IN, USA) in all patients, without using any other implant design during the study period. This system has highly crosslinked polyethylene components that are sterilized by gamma irradiation and packaged in a nitrogen environment. Preoperatively long-standing AP radiographs (hip to ankle) were obtained to determine the femoral-guide valgus angle, and the desired position of the entry hole for the femoral and tibial intramedullary guide for a perpendicular cut to the mechanical axis. Distal femoral bone was resected using the intramedullary guide, and AP cutting was performed using an anterior referencing system in 3° or 5° external rotation relative to the posterior condylar axis, which was confirmed by Whiteside’s line. Tibial preparation then was done using an intramedullary tibial guide with a cutting block with 7° of posterior slope, according to the manufacturer’s recommendation. After stability was confirmed by ligament balancing using the trial components, the femoral and tibial components were fixed with cement.
Radiographic Evaluation
We attempted to take correct long-standing mechanical axis (hip to knee) radiographs for all patients within 1 year after TKA. These films were used to measure the following mechanical variables: overall mechanical alignment, mechanical femoral component alignment (MFCA), and mechanical tibial component alignment (MTCA). Overall mechanical alignment is determined by measuring the angle between the mechanical axis of the femur and the mechanical axis of the tibia. The area under the curve (AUC) for mechanical alignment for aseptic revision was 0.717 (95% CI, 0.625–0.809). A mechanical alignment of 3.5° was found to be the cutoff value for the mechanical failures, with a sensitivity of 63% and a specificity of 76%. The mechanical alignment was measured in 1o increments without decimals. Therefore, knees that showed postoperative mechanical alignment of 0° ± 3° were considered to have neutral alignment. Varus angles were expressed as positive values, whereas valgus angles were expressed as negative values. Knees were considered to have varus and valgus malalignment if the angle was greater than 3° and less than -3°, respectively. Depending on the postoperative mechanical alignment, the knees undergoing TKA in the study cohort were assigned to one of three groups: neutral group, or the varus (> 3°) group or valgus (< -3°) outlier group. To determine the origin of the malalignment in the outlier groups, the MFCA and MTCA were measured using these long-standing films. These values represent the mechanical alignment of the femoral and tibial components, respectively. MFCA and MTCA were defined as 0° if the distal femoral and proximal tibial component surfaces were perpendicular to the mechanical axis of the femur and tibia, respectively. A positive value indicates varus of the relevant component surface relative to the corresponding mechanical axis, whereas a negative value indicates valgus. To test the reliability of these measurements, 50 patients were selected randomly and all variables were measured twice at 2-week intervals by two orthopaedic surgeons (HIC, BKJ). For all of these measurements, the intraclass correlation coefficient (ICC) of intraobserver reliability was greater than 0.90, whereas the ICC of interobserver reliability was greater than 0.85. Because all measurements were highly reproducible, the measurements made by one researcher (HIC) were used for all subsequent analyses.
Routine weightbearing AP and lateral radiographs were taken at 6 weeks, 3 months, 6 months, 1 year, and every 2 to 3 years thereafter. Progressive radiolucent lines beyond 2 mm and gross shifting of the component that caused subsidence or tilting were defined as aseptic loosening [7]. Aseptic loosening, polyethylene wear, and instability that should be treated by revision surgery were regarded as the endpoint of implant survival.
Statistical Analyses
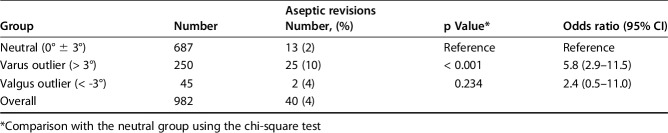
The postoperative hip-to-ankle mechanical alignment of the 982 knees was 1.7° ± 3.2° (range, -11° to 12°). Of these, the preoperative long-films were available for 943 knees and the preoperative mechanical alignment was 10.7° ± 6.1° (range, -17° to 35°). For the 943 knees for which the preoperative mechanical axis radiographs were available, the preoperative mechanical alignment was not associated with aseptic revision (odds ratio [OR], 1.0; 95% CI, 1.0–1.1; p = 0.096). In total, 687 (70%) knees showed neutral postoperative mechanical alignment (0° ± 3°), 250 (25%) were varus greater than 3° outliers, and 45 (5%) were valgus less than -3° outliers. During followup, 35 knees (4%) showed aseptic loosening at 7 ± 4 years (range, 0.1–14 years), and five (1%) showed polyethylene wear at 12 ± 1 years (range, 10-13 years). No patients had instability (Fig. 1). These 40 patients (40 knees) were recommended to have revision surgery and considered as an endpoint for analysis, although only 31 actually underwent revision surgery. The remaining nine did not undergo revision surgery owing to a medical problem or because they did not agree to undergo a reoperation. There were femoral component loosening only (n = 6; 15%), tibial component loosening only (n = 23; 58%), loosening of both components (n = 6; 15%), and polyethylene wear (n = 5; 13%), but no instability. Thus, tibial loosening (n = 29; 73%) was the most-common reason for the aseptic revision, followed by femoral loosening (n = 12; 30%).
Fig. 1.
The distribution of postoperative overall mechanical alignment on long-standing hip-to-ankle radiographs is shown. The aseptic loosening and wear cases are indicated by the red and yellow bars, respectively. PE = polyethylene.
To determine whether the risk of aseptic revision was greater among each outlier than that of knees aligned in 0° ± 3° on mechanical axis radiographs, the varus (> 3°) and valgus (< -3°) outlier groups were compared with the neutral alignment group. Aseptic revision incidence was compared among groups using chi-square tests, and implant survival rates were analyzed using the life table methods with the Gehan-Wilcoxon test (see Appendix, Supplemental Digital Content 1). Patients who died or were lost to followup were considered to be censored at the time of the latest visit.
We found that varus knees did associate with increased rates of aseptic revision (p = 0.002). In the valgus group, there were only two knees with femoral loosening. This group did not differ from the neutral group in terms of survival (p = 0.241). Consequently, only the varus group was subjected to component malalignment analysis. We investigated the MFCA and MTCA in the varus knees to determine the origin of malalignment and its association with aseptic revision. To determine whether the knees with femoral or tibial component varus malalignment (> 3°) had higher aseptic revision rates than those with well-aligned components within 0° ± 3°, respectively, chi-square tests were used. To assess the effect of several covariates on the aseptic revision rate of the outlier groups, multivariate survival analyses were performed using the Cox proportional hazard regression model with the backward selection method. The following covariates were included: age, sex, implant (LPS or LPS-Flex), BMI, MFCA beyond ± 3°, and MTCA beyond ± 3°. All statistical analyses were performed using SPSS, Version 21.0 (IBM Corporation, Armonk, NY, USA).
Results
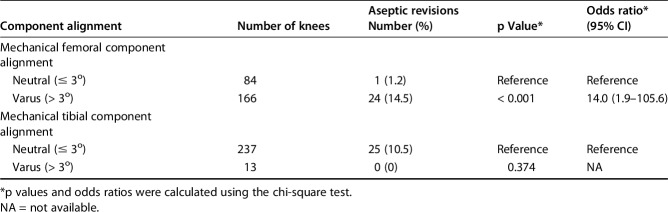
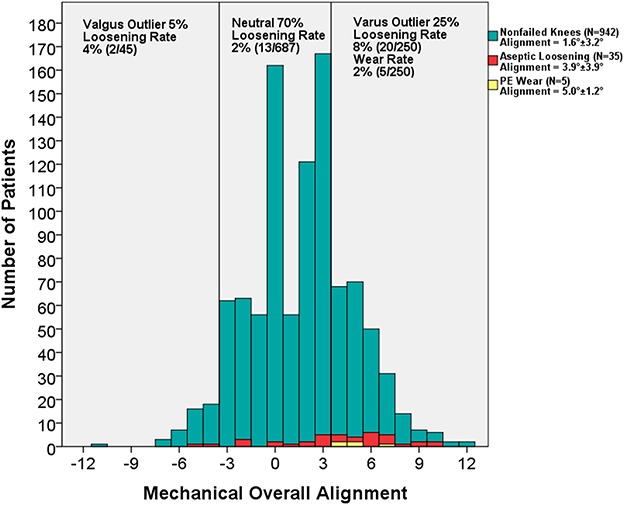
Varus, but not valgus, malalignment of more than 3 degrees from neutral mechanical alignment was associated with increased rates of aseptic revision. Of 40 knees that were recommended to have revision surgery, 13 (two femoral only, eight tibial only, and three with both component loosening) were in the neutral mechanical axis group, 25 (two femoral only, 15 tibial only, three with both component loosening, and five with polyethylene wear) were in the varus outlier mechanical axis group, and two (both with femoral loosening) were in the valgus outlier mechanical axis group (4%). Notably, all five of the knees with polyethylene wear were in the varus outlier group at more than 10 years (mean, 12 ± 1 years; range, 10-13 years) after the index surgery. Relative to the neutral knees, the OR for aseptic revision in the varus group was 5.8 (95% CI, 2.9–11.5; p < 0.001). However, the valgus outlier knees did not differ, with the numbers available, from the neutral knees in terms of aseptic revision rates (OR, 2.4; 95% CI, 0.5–11.0; p = 0.234) (Table 1). The varus knees had lower implant survival with time after surgery than the neutral group (p = 0.002). However, the neutral and valgus knees did not differ in terms of implant survival (p = 0.241) (Fig. 2). Interestingly, the three groups did not differ in terms of 5-year implant survival: in the neutral, varus, and valgus groups, it was 98% (95% CI, 97%–99%), 97% (95% CI, 95%–99%) (versus neutral, p = 0.351), and 98% (95% CI, 93%–100%) (versus neutral, p = 0.757), respectively. However, at 10 years, the probability of survival was lower in the varus group (87%; 95% CI, 80%–93%) than in the neutral group (98%; 95% CI, 97%–99%; p = 0.001). There was no difference between the valgus (95%; 95% CI, 87%–100%) and neutral knees in terms of 10-year probability of survival (p = 0.401). The difference between the varus and neutral knees in terms of survival was even more pronounced at 15 years (73% [95% CI, 62%–84%] versus 94% [95% CI, 88%–100%]; p = 0.001) (Appendix, Supplemental Digital Content 2).
Table 1.
Aseptic revision in knees with postoperative neutral, varus, and valgus mechanical alignment
Fig. 2.
Survival of the implants in the neutral, varus, and valgus groups during followup is shown. The varus outliers had lower survivorship than the neutral group (Gehan-Wilcoxon test, p = 0.002), but there was no difference between the neutral and valgus groups (Gehan-Wilcoxon test, p = 0.241). However, the neutral and varus groups did not differ, with the numbers available, in implant survival until 10 years after the index operation.
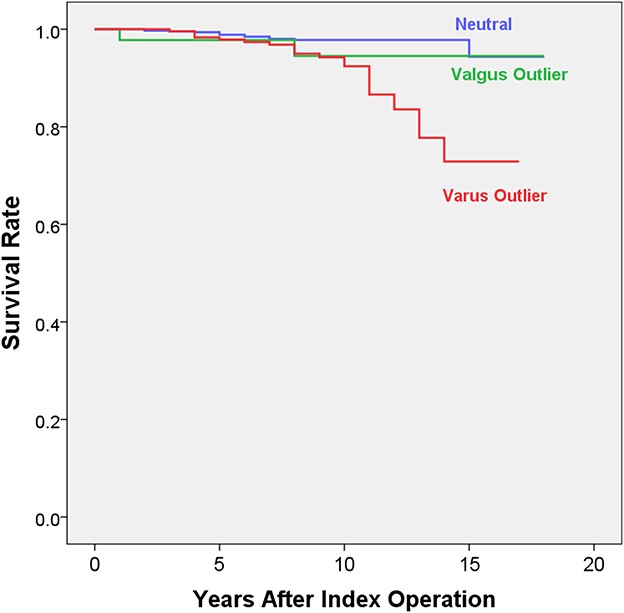
Femoral malalignment was associated with an increased risk of revision, but tibial malalignment was not in the varus outliers. The component alignment analysis in the varus outlier knees showed that the main cause of varus malalignment was femoral component varus malposition. In the 250 varus knees, the mean overall mechanical alignment was 5.7° ± 1.7° (range, 4°–12°), the mean MFCA was 4.2° ± 2.0° (range, -1° to 10°), and the mean MTCA was 0.9° ± 1.7° (range, -3° to 5°). Of these 250 knees, 166 (66%) showed femoral component varus malposition (defined as MFCA > 3°) on long-standing films. By contrast, most of the varus outlier knees (237 of 250; 95%) had well-aligned tibial components (ie, MTCA ≤ 3°) (Fig. 3). Of the 25 varus knees that were treated for aseptic revision during followup, 24 (96%) had femoral component varus greater than 3°. An MFCA of greater than 3° varus was associated with a higher risk of aseptic revision (OR, 14.0; 95% CI, 1.9–105.6; p < 0.001). With respect to the tibia, the knees with well-aligned and malaligned tibial components did not differ, with the numbers available, in terms of aseptic revision incidence (p = 0.374) (Table 2). We found that older age (OR, 0.9; 95% CI, 0.8–0.9; p < 0.001) and increased femoral varus, that is, MFCA greater than 3° (OR, 11.4; 95% CI, 1.5– 85.4; p = 0.018) were associated with aseptic revisions in the varus knees of this series. However, sex (p = 0.985), BMI (p = 0.427), type of femoral component (LPS or LPS-Flex) (p = 0.457), and MTCA (p = 0.983) were not associated with the risk of aseptic revision.
Fig. 3 A-B.
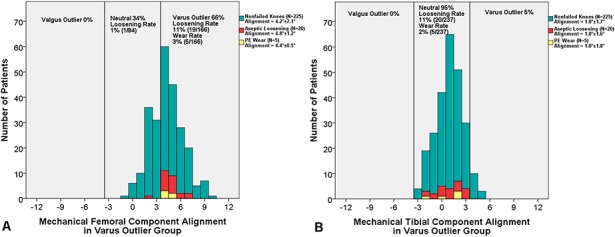
The distributions of (A) mechanical femoral component alignment (MFCA) and (B) mechanical tibial component alignment (MTCA) in the varus outlier group are shown. The histograms indicate that these knees had a propensity toward varus-deviated MFCA and well-aligned MTCA. This suggests that overall malalignment of the varus outlier knees was the result of varus MFCA. Moreover, the knees with MFCA greater than 3° showed aseptic loosening (red bars) more frequently (11%) than the knees with neutral MFCA (1%). PE = polyethylene.
Table 2.
Aseptic revisions in varus outlier knees with mechanical femoral or tibial component malalignment
Discussion
The notion that neutral postoperative alignment is essential to assure long-term implant survival after TKA has been based mostly on short-film studies [2, 9, 14, 27] even though some of them were conducted with large cohorts (more than 1000 knees) and evaluated the outcomes over long durations [15, 29]. However, this is challenged by some studies [18, 21, 25] that used long-standing films to measure mechanical alignment, showing that residual postoperative varus alignment on long mechanical films does not compromise the longevity of the modern knee prosthesis. In addition, considering large variations in femoral bowing [12], mechanical malalignment from an extraarticular origin might be underestimated in short-film studies. We, therefore, conducted a large-scale, long-term, long-film-based cohort study and we found that malalignment exceeding 3o varus of the mechanical axis is associated with inferior long-term implant survivorship and that the primary origin of the overall varus malalignment was femoral component varus malpositioning.
Our study has several limitations. First, the study cohort consisted of patients with osteoarthritis who underwent primary TKA and were identified by retrospective review of a medical database. This retrospective design increases the chance of selection bias. In addition, 118 patients (15% of the knees) were lost to followup before 2 years, therefore our results might be biased by these patients whose long-term results are unknown. Second, only posterior-stabilized fixed bearing prostheses were used in the enrolled patients. Therefore, it may not be possible to generalize our findings to patients in whom cruciate retaining or mobile bearing designs were used. Third, although the high proportion of females in our cohort is a unique characteristic of Asian patients undergoing TKA [13], this also reduces the extent to which our results can be generalized. Fourth, we did not analyze the effect of mechanical malalignment on patient-reported outcomes, including pain, ROM, function, or satisfaction, and the clinical outcomes according to the mechanical (hip to ankle) alignment should be evaluated in a further study. The bias toward varus overall mechanical axis alignment was so prevalent in this series that relatively few knees (45 of 982) met our criteria for a valgus outlier mechanical axis (more than 3o valgus mechanical axis), limiting our ability to statistically distinguish outcomes of the valgus outlier mechanical group from those of the two more heavily populated mechanical axis groups.
Interestingly, a meta-analysis [15] and a systematic review [29] suggested that the main difference between the studies that do [2, 8, 14, 27, 28] and do not [4, 18, 21, 25] find that neutral alignment is essential for implant survival was that they used short and long films, respectively. Considering that the anatomic and mechanical axes correlate [22, 26], it seems more likely that this discrepancy reflects the shortcomings of the studies that found neutrality is not essential such as limited followup or cohort size [4, 10, 25, 30]. Therefore, it remains unclear whether the long-term durability of a TKA will not be compromised by permitting residual malalignment [1, 15, 29]. Our results support the historical view [9, 11, 20, 28], despite that we used long-film measurements of mechanical alignment: varus outliers in mechanical hip-to-ankle alignment were associated with higher rates of aseptic revision. Notably, 10-year survivorship free from aseptic loosening and polyethylene wear was lower among varus outliers than among knees with neutral alignment.
Moreover, we found that femoral component mechanical malalignment (which cannot be detected by short-film anatomic alignment evaluations) impaired overall implant survival. The most straightforward means of achieving a neutral mechanical axis during TKA involves cutting the distal femur and the proximal tibia perpendicularly in the coronal plane to the mechanical axis that runs from the hip center to the ankle center. During conventional TKA without computer assistance (ie, navigation, robotics, or patient-specific instrumentation), it can be more difficult to position the femoral component perpendicular to the mechanical axis than it is to position the tibial component [3, 17, 24]. The lower leg is exposed in the operative field; this allows visual verification of proximal tibial cutting during surgery. By contrast, the perpendicular distal femoral cut relies on the preoperatively planned intramedullary guide axis and the cutting cannot be checked precisely because the hip center cannot be localized if C-arm imaging or navigation is not available. Moreover, the femur is prone to anatomic deformities such as lateral bowing that increase the risk of femoral component malalignment and consequently overall malalignment [12]. Although a couple short-film studies [14, 27] showed that the femoral component is generally aligned better than the tibial component, short films cannot measure the real mechanical femoral alignment and thus cannot detect when extraarticular anatomic variations induce mechanical femoral component malalignment. In the current study using long films, we found that the femoral component was more varus than the tibial component and the femoral component varus malposition also was associated with a higher risk of implant loosening despite that tibial component loosening was the most common site of aseptic loosening in our series. These observations suggest that it may be advisable for surgeons to use long-standing preoperative films to precisely plan the femoral cutting guide axes for the unique anatomy of the patient or consider implementation of some other assistive supporting technology (patient-specific cutting guides, computer assistance, robotic surgery) to limit the prevalence of mechanical axis varus after prior TKA.
This study supports the classic view in the field, namely, that coronal mechanical varus malalignment is associated with poorer long-term implant survivorship. We also showed that short to mid-term followup may not be sufficient to detect the effect of malalignment on implant survival. In addition, we observed that femoral component varus malposition was mainly responsible for the overall varus malalignment in our series and that this was responsible for the increased mechanical failure rate in the varus knees. Long-standing radiographs seems to be the reasonable approach to assess overall mechanical limb alignment because short films cannot detect extraarticular deformities and underestimate femoral component mechanical malalignment.
Footnotes
Each author certifies that he has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the College of Medicine, University of Ulsan, Asan Medical Center, Seoul, Korea.
References
- 1.Abdel MP, Oussedik S, Parratte S, Lustig S, Haddad FS. Coronal alignment in total knee replacement: historical review, contemporary analysis, and future direction. Bone Joint J. 2014;96:857–862. [DOI] [PubMed] [Google Scholar]
- 2.Berend ME, Ritter MA, Meding JB, Faris PM, Keating EM, Redelman R, Faris GW, Davis KE. Tibial component failure mechanisms in total knee arthroplasty. Clin Orthop Relat Res. 2004;428:26–34. [DOI] [PubMed] [Google Scholar]
- 3.Blakeney WG, Khan RJ, Wall SJ. Computer-assisted techniques versus conventional guides for component alignment in total knee arthroplasty: a randomized controlled trial. J Bone Joint Surg Am. 2011;93:1377–1384. [DOI] [PubMed] [Google Scholar]
- 4.Bonner TJ, Eardley WG, Patterson P, Gregg PJ. The effect of post-operative mechanical axis alignment on the survival of primary total knee replacements after a follow-up of 15 years. J Bone Joint Surg Br. 2011;93:1217–1222. [DOI] [PubMed] [Google Scholar]
- 5.Chang CB, Choi JY, Koh IJ, Seo ES, Seong SC, Kim TK. What should be considered in using standard knee radiographs to estimate mechanical alignment of the knee? Osteoarthritis Cartilage. 2010;18:530–538. [DOI] [PubMed] [Google Scholar]
- 6.Choong PF, Dowsey MM, Stoney JD. Does accurate anatomical alignment result in better function and quality of life? Comparing conventional and computer-assisted total knee arthroplasty. J Arthroplasty. 2009;24:560–569. [DOI] [PubMed] [Google Scholar]
- 7.Ewald FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989;248:9–12. [PubMed] [Google Scholar]
- 8.Fang DM, Ritter MA, Davis KE. Coronal alignment in total knee arthroplasty: just how important is it? J Arthroplasty. 2009;24(6 suppl):39–43. [DOI] [PubMed] [Google Scholar]
- 9.Feng EL, Stulberg SD, Wixson RL. Progressive subluxation and polyethylene wear in total knee replacements with flat articular surfaces. Clin Orthop Relat Res. 1994;299:60–71. [PubMed] [Google Scholar]
- 10.Howell SM, Papadopoulos S, Kuznik K, Ghaly LR, Hull ML. Does varus alignment adversely affect implant survival and function six years after kinematically aligned total knee arthroplasty? Int Orthop. 2015;39:2117–2124. [DOI] [PubMed] [Google Scholar]
- 11.Jeffery RS, Morris RW, Denham RA. Coronal alignment after total knee replacement. J Bone Joint Surg Br. 1991;73:709–714. [DOI] [PubMed] [Google Scholar]
- 12.Kim JM, Hong SH, Kim JM, Lee BS, Kim DE, Kim KA, Bin SI. Femoral shaft bowing in the coronal plane has more significant effect on the coronal alignment of TKA than proximal or distal variations of femoral shape. Knee Surg Sports Traumatol Arthrosc. 2015;23:1936–1942. [DOI] [PubMed] [Google Scholar]
- 13.Kim SJ, Basur MS, Park CK, Chong S, Kang YG, Kim MJ, Jeong JS, Kim TK. Crosscultural adaptation and validation of the Korean version of the new Knee Society knee scoring system. Clin Orthop Relat Res. 2017;475:1629–1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim YH, Park JW, Kim JS, Park SD. The relationship between the survival of total knee arthroplasty and postoperative coronal, sagittal and rotational alignment of knee prosthesis. Int Orthop. 2014;38:379–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu HX, Shang P, Ying XZ, Zhang Y. Shorter survival rate in varus-aligned knees after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2016;24:2663–2671. [DOI] [PubMed] [Google Scholar]
- 16.Longstaff LM, Sloan K, Stamp N, Scaddan M, Beaver R. Good alignment after total knee arthroplasty leads to faster rehabilitation and better function. J Arthroplasty. 2009;24:570–578. [DOI] [PubMed] [Google Scholar]
- 17.Maderbacher G, Keshmiri A, Schaumburger J, Zeman F, Birkenbach AM, Craiovan B, Grifka J, Baier C. What is the optimal valgus pre-set for intramedullary femoral alignment rods in total knee arthroplasty? Knee Surg Sports Traumatol Arthrosc. 2016. May 6. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 18.Magnussen RA, Weppe F, Demey G, Servien E, Lustig S. Residual varus alignment does not compromise results of TKAs in patients with preoperative varus. Clin Orthop Relat Res. 2011;469:3443–3450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Matsuda S, Kawahara S, Okazaki K, Tashiro Y, Iwamoto Y. Postoperative alignment and ROM affect patient satisfaction after TKA. Clin Orthop Relat Res. 2013;471:127–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Matsuda S, Miura H, Nagamine R, Urabe K, Harimaya K, Matsunobu T, Iwamoto Y. Changes in knee alignment after total knee arthroplasty. J Arthroplasty. 1999;14:566–570. [DOI] [PubMed] [Google Scholar]
- 21.Matziolis G, Adam J, Perka C. Varus malalignment has no influence on clinical outcome in midterm follow-up after total knee replacement. Arch Orthop Trauma Surg. 2010;130:1487–1491. [DOI] [PubMed] [Google Scholar]
- 22.McGrory JE, Trousdale RT, Pagnano MW, Nigbur M. Preoperative hip to ankle radiographs in total knee arthroplasty. Clin Orthop Relat Res. 2002;404:196–202. [DOI] [PubMed] [Google Scholar]
- 23.Morgan SS, Bonshahi A, Pradhan N, Gregory A, Gambhir A, Porter ML. The influence of postoperative coronal alignment on revision surgery in total knee arthroplasty. Int Orthop. 2008;32:639–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nam D, Vajapey S, Haynes JA, Barrack RL, Nunley RM. Does use of a variable distal femur resection angle improve radiographic alignment in primary total knee arthroplasty? J Arthroplasty. 2016;31(9 suppl):91–96. [DOI] [PubMed] [Google Scholar]
- 25.Parratte S, Pagnano MW, Trousdale RT, Berry DJ. Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am. 2010;92:2143–2149. [DOI] [PubMed] [Google Scholar]
- 26.Petersen TL, Engh GA. Radiographic assessment of knee alignment after total knee arthroplasty. J Arthroplasty. 1988;3:67–72. [DOI] [PubMed] [Google Scholar]
- 27.Ritter MA, Davis KE, Meding JB, Pierson JL, Berend ME, Malinzak RA. The effect of alignment and BMI on failure of total knee replacement. J Bone Joint Surg Am. 2011;93:1588–1596. [DOI] [PubMed] [Google Scholar]
- 28.Ritter MA, Faris PM, Keating EM, Meding JB. Postoperative alignment of total knee replacement: its effect on survival. Clin Orthop Relat Res. 1994;299:153–156. [PubMed] [Google Scholar]
- 29.Vandekerckhove PJ, Lanting B, Bellemans J, Victor J, MacDonald S. The current role of coronal plane alignment in total knee arthroplasty in a preoperative varus aligned population: an evidence based review. Acta Orthop Belg. 2016;82:129–142. [PubMed] [Google Scholar]
- 30.Vanlommel L, Vanlommel J, Claes S, Bellemans J. Slight undercorrection following total knee arthroplasty results in superior clinical outcomes in varus knees. Knee Surg Sports Traumatol Arthrosc. 2013;21:2325–2330. [DOI] [PubMed] [Google Scholar]