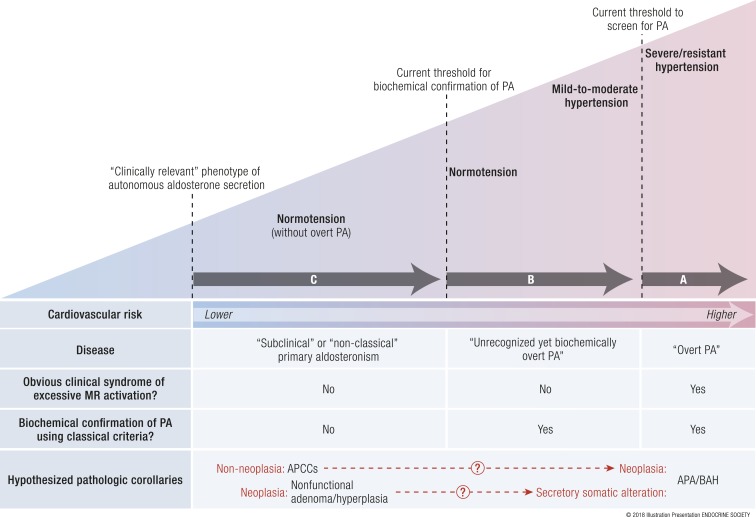
Figure 4.
The severity spectrum of primary aldosteronism. (A) Overt primary aldosteronism. The Endocrine Society clinical practice guidelines recommend screening for primary aldosteronism using the aldosterone-to-renin ratio in severe or resistant hypertension. This practice of screening for a high aldosterone-to-renin ratio (>20 to 30 ng/dL per ng/dL per hour in conventional units or >750 to 830 pmol/L per μg/L per hour in SI units) is highly sensitive for detecting patients with severe hypertensive primary aldosteronism, that is, those with an obvious clinical syndrome of excessive MR activation (hypertension and/or hypokalemia) who are confirmed to have biochemically overt primary aldosteronism and likely to have an APA or bilateral adrenal hyperplasia as the cause of their disease. These cases of overt primary aldosteronism have the highest risk for incident cardiovascular disease. (B) Unrecognized, yet biochemically overt primary aldosteronism. Using confirmatory testing thresholds recommended by the Endocrine Society (see Table 3), human studies have demonstrated that a substantial portion of normotensive and mild-to-moderate hypertensive persons, populations for whom primary aldosteronism screening is not routinely recommended, have unrecognized, yet biochemically overt primary aldosteronism. (C) Subclinical or nonclassical primary aldosteronism. Even below the Endocrine Society recommended thresholds of what is currently considered biochemical confirmation of primary aldosteronism, a continuum of renin-independent aldosterone secretion can be detected among healthy normotensive and moderately hypertensive persons, in whom no obvious clinical syndrome of MR overactivation is apparent. These persons have subtle biochemical evidence of renin-independent aldosteronism (renin suppression with inappropriately “normal” or high aldosterone levels) and higher risk for developing hypertension. This phenotype may best be described as subclinical or nonclassical primary aldosteronism (41). The hypothesized pathologic corollaries remain theoretical and are discussed in “What Causes Primary Aldosteronism?” One theory suggests that the newly described finding of APCCs may represent an aldosterone-secretory abnormality wherein a subset may then acquire neoplastic alterations to transform into APAs or bilateral adrenal hyperplasia. An alternative theory suggests that nonfunctional adrenocortical neoplasia may acquire secretory somatic alterations to become APAs or bilateral adrenal hyperplasia. A combination of both or neither theories may also be possible. BAH, bilateral adrenal hyperplasia; PA, primary aldosteronism. Adapted with permission from Brown JM, Robinson-Cohen C, Luque-Fernandez,MA, et al. The spectrum of subclinical primary aldosteronism and incident hypertension: A cohort study. Ann Intern Med. 2017;167(9):630–641. http://annals.org/aim/article-abstract/2657166/spectrum-subclinical-primary-aldosteronism-incident-hypertension-cohort-study ©American College of Physicians. [© 2018 Illustration Presentation ENDOCRINE SOCIETY]