Abstract
Background
Despite the importance of home enteral nutrition (HEN), there is a lack of understanding within the medical and general community of how HEN impacts the lives of patients and caregivers. Using a theoretical orientation that attends to the materiality of both everyday and medical objects, we explored patients' and family caregivers' everyday experiences of administering feeds during HEN.
Methods
Using the photo‐elicitation interviewing method, patients on HEN and their family caregivers were asked to take up to 10 photographs to portray material items and activities that they considered foundational to HEN. They subsequently narrated their experiences and the participant‐generated photographs in an interview. Participant‐generated photographs (126) and accompanying narratives were analyzed using layered analysis, and results were theorized with attention to both social and material significance of HEN.
Results
Patients and caregivers detailed overcoming misconceptions of HEN, and through their use of photographs, they conveyed their expertise in developing their own HEN feeding systems and practices, that used both the material artifacts provided by the hospital (the tube, syringe, and formula) as well as everyday material items found in the patient's home. More than this, photographs and patient narratives depicted intimate involvement of patients' families in tube feeding. This yielded a more comprehensive understanding of the material and experiential realities of HEN.
Conclusion
Home enteral nutrition was found to be a shared familial experience, that in addition to requiring medical equipment also incorporated ordinary material artifacts within the social setting of the home and family life. To more accurately convey the material, experiential, and social realities of HEN to future patients, our findings underscore the importance of drawing on both visual and textual forms of patient‐produced information in the development of HEN patient educational materials.
Keywords: family caregivers, HEN education, home enteral nutrition, materiality, photo‐elicitation interviewing, tube feeding
Short abstract
Background
Despite the importance of home enteral nutrition (HEN), there is a lack of understanding within the medical and general community of how HEN impacts the lives of patients and caregivers. Using a theoretical orientation that attends to the materiality of both everyday and medical objects, we explored patients' and family caregivers' everyday experiences of administering feeds during HEN.
Methods
Using the photo‐elicitation interviewing method, patients on HEN and their family caregivers were asked to take up to 10 photographs to portray material items and activities that they considered foundational to HEN. They subsequently narrated their experiences and the participant‐generated photographs in an interview. Participant‐generated photographs (126) and accompanying narratives were analyzed using layered analysis, and results were theorized with attention to both social and material significance of HEN.
Results
Patients and caregivers detailed overcoming misconceptions of HEN, and through their use of photographs, they conveyed their expertise in developing their own HEN feeding systems and practices, that used both the material artifacts provided by the hospital (the tube, syringe, and formula) as well as everyday material items found in the patient's home. More than this, photographs and patient narratives depicted intimate involvement of patients' families in tube feeding. This yielded a more comprehensive understanding of the material and experiential realities of HEN.
Conclusion
Home enteral nutrition was found to be a shared familial experience, that in addition to requiring medical equipment also incorporated ordinary material artifacts within the social setting of the home and family life. To more accurately convey the material, experiential, and social realities of HEN to future patients, our findings underscore the importance of drawing on both visual and textual forms of patient‐produced information in the development of HEN patient educational materials.
1. INTRODUCTION
Enteral nutrition (EN) is a life‐sustaining nutritional therapy delivered directly to the stomach via a tube, for patients who have a functional gastrointestinal (GI) tract but are unable to meet their nutritional needs by oral intake. When EN is clinically indicated, it can improve the clinical course, patients' quality of life and prognosis, and can significantly reduce morbidity and mortality rates.1, 2, 3, 4 Enteral nutrition is also preferred to parenteral nutrition, which is delivered via the venous system, as EN is a more physiologic transport route and associated with lower cost and increased safety.1, 3, 4 However, both the placement of enteral feeding tubes and the subsequent provision of EN is not without potential complications.5, 6, 7 Although the data are variable, 5% to 30% of patients can experience complications, with the most prevalent being peristomal infection and pain/granulation tissue around stoma site, as well as clogging, leakage, and dislodgement of the feeding tube.5, 8
In addition to clinical complications, the provision of home enteral nutrition (HEN) to patients who are often quite debilitated has a significant impact on family dynamics, placing a great deal of stress on caregivers whose assistance is crucial to success. Meal times as a ritual and site of social relations hold familial and social significance. Eating or not eating together and attending social gatherings that center around food are experienced differently by patients and their caregivers.5, 9 Exploring the social significance, family dynamics, and embodied experiences as they relate to HEN is an important aspect often overlooked in clinical practice and sociological work.10 Despite the tremendous psychosocial impact of HEN, there is a paucity of data on patient and caregiver perspectives regarding the range of difficulties associated with HEN. What is known, however, is that seeking, accepting, and effectively utilizing support are key factors in HEN users' successful adaptation to HEN programs.9 Therefore, gaining patient and caregiver perspectives enables clinicians to better comprehend the impact HEN has on patients and families, and subsequently individualize their care.11
The objective of this study was to examine the material artifacts involved in the delivery of HEN and to explore patient and caregiver experiences around HEN in order to gain a better understanding of the impact and social significance of EN. We also examined data for any contributing factors toward HEN complications and areas for improved practice integration.
2. METHODS
2.1. Theoretical framework
This study used a “sociomaterial approach,”12, 13 which focused not only on how patients and their caregivers experience tube feeding but also on how they use and assign significance to various material artifacts (such as feeding tube, bag, syringe, formula, food, and drink) to accomplish tube feeding. This postanthropocentric approach asks us to attend to the significance embedded within the assemblages of the human and nonhuman and the relationships between them.10, 14 In the context of health care, these material assemblages and how they are used to provide care are important to attend to, as care that is performed in the home environment is considered mundane and is, thus, overlooked.14 By highlighting the sociomaterial assemblages in the home, we highlight the role of these “ordinary” materials which work within relationships but also mediate them, to perform important and sometimes life‐saving acts of care.10 These acts of care in the home frequently use a combination of medical and ordinary or “mundane” household materials, and play an important role in preserving one's own dignity and self‐care in the face of significant disease and illness.14 Material approaches have been used in the study of food and health care. Food has a distinct material culture that involves the material of food itself, its preparation, and the bodies that ingest it.15 Moreover, food and eating rest within, and are shaped by, broader social relationships.15 As we will argue, what is important for the social study of HEN, caring for another's body and for their food and processes of eating is not only a highly material practice that involves a practical management of various materials and artifacts, but it is also a practice that makes and remakes relationships with every meal that is prepared, shared, and delivered.15
2.2. Recruitment and setting
The study was approved by the Mayo Clinic Institutional Review Board (ID: 14‐009588), Rochester, MN. Patients were recruited from the Mayo Clinic HEN program, which assists 800 new patients on HEN on an annual basis, with the majority (~80%) initiating EN during their hospitalization. Patients were eligible for our study if they were 18 years and older, able to take up to 10 photos in their home, complete an interview, and were within the first 6 weeks of their surgical placement of the enteral tube. Patients were recruited via referrals from the HEN care team personnel who provided names and identifiers of potential patients (up to 50 patients) with upcoming appointments to the research staff. Research staff then reached out to patients via telephone or during patients' routine visit and/or after tube placement. Research staff presented patients with study information including instructions on taking participant‐generated photographs, the photo‐elicitation interview process, consent and privacy authorization information, a request for research participation, and information on nominating a family member for research participation. Patients were requested to nominate at least 1 family member who they deemed to be a primary caregiver, able to take photos in the home of the patient, and willing to complete a photo‐elicitation interview. For patients (n = 8) who were contacted via telephone, a study kit containing a consent form (for patient and family caregiver), a camera, photo memory cards, and instructions for taking and returning pictures were mailed via confidential mailing and return service. Two patients with their family caregivers were recruited and consented during a routine post tube placement visit, after which a study kit was provided to them. Consent to participate included permission to access patients' demographics, disease characteristics via electronic health records, and permission for the research team to use all data gathered including photographs for scientific and educational purposes. All participants signed a written consent form.
Initial enrolment took place between May and December 2015, and resulted in 32 participants. Nine participants (6 patients and 3 caregivers) later declined participation, and the study staff were unable to reach 5 participants (4 patients and 1 caregiver) to schedule interviews. Participant recruitment ceased after photo‐elicitation interviews with 10 patients and 8 caregivers and when the research staff—through concurrent analysis of interview transcripts and photographs—determined that data saturation had been achieved.
2.3. Data collection
2.3.1. Participant‐generated photos
Using the cameras provided by the researchers, participants were asked to take up to 10 photos (10 for patients and 10 for family caregivers) of activities, experiences, feelings, innovations, or items that were considered meaningful and representative of their HEN experience in their home environment. We adopted a reflexive photography approach,16 which enables participants to make decisions on what pictures they will take and which pictures they will provide to researchers for discussion (and in what manner), thereby placing control in the hands of the patients and caregivers as to what pictures and topics will be discussed and how their illness experience and subjectivity will be represented to the researcher in the photo‐elicitation interview.17 All participants were encouraged to review the photographs they themselves took and to delete any photographs which they did not wish to include before sending the cameras back to research staff.
2.3.2. Photo‐elicitation interview
The photo‐elicitation interviews (PEI)18, 19, 20, 21 were conducted from May to December, 2015 and were structured by the ethical guidelines established by photo‐elicitation and visual research methodology scholars.18, 20, 22, 23 This included revisiting consent with participants for publication and use of deidentified photographs and the opportunity for participants to remove any photos for further use in the research project. No participant withdrew pictures from the study. Photo‐elicitation interview is a useful method in circumstances of limited verbal communication, which is common in the patient population we studied. Feeding tubes are often required for head and neck cancers, strokes, and degenerative neurological conditions that affect not only swallowing but also speech. Some of the patients have limited verbal expression because of language disabilities (for example, aphasia in patients with stroke) or speech disabilities in which providing a detailed verbal explanation or description can be both challenging and exhausting. Photo‐elicitation interviews were conducted either in‐person or over the phone, based on patient and caregiver preferences.
In‐person interviews
Upon receipt of cameras and consent forms from participants, a researcher telephoned participants to schedule an interview. Photos were then uploaded onto a secured drive on an institutional laptop computer. On interview day, researchers brought a computer containing participant's photos and interview guides to the preferred interview location as identified by participants. Before each in‐person interview, participants were given the opportunity to review the photos and select the ones they will like to discuss. Six in‐person dyadic interviews (patients and their caregivers) were conducted during routine patients' visits to the clinic: 3 of the interviews were conducted in the hospital's private rooms and 3 conducted at the patients' lodging facility after their clinic visit. One couple and a patient (whose caregiver was not interviewed) were interviewed at their home.
Over‐the‐phone interviews
Upon receipt of cameras and consent forms, pictures were downloaded onto a secure sever. All images on the camera were printed (in pairs) through our institution's media services and labeled with each participants' study ID. Copies of the pictures were mailed to participants and a researcher called participants to schedule an interview over the phone. Before each interview date, a researcher called participants to ensure that they had received their photographs. Three interviews (2 patients and 1 caregiver) were conducted individually over the phone.
All interviews were conducted using a semistructured interview guide. Topics explored include patients' and caregivers' experiences regarding diagnosis leading to nutritional intervention, tube feeding process and what it means to them, information received about the HEN program, general experience with the program, and opportunities for improvement to the program. Participants used the pictures to describe their experiences with HEN, including challenges and improvements that could be made with the overall HEN process. Participants discussed what was in the picture and where, when, and why they took the pictures, allowing the researchers to gain an understanding of the symbolic significance of the photo. Interviews took approximately 50 minutes. All interviews were audio recorded and transcribed verbatim. Patients' disease characteristics and demographics were obtained from electronic health records. In this paper, “participants” refers to both the patients and caregivers who enrolled in the study. Where the use of participants is not applicable, the terms “patients” or “caregivers” are used.
2.4. Analysis
Analysis was guided by a layered approach (Table 1) to ensure the researchers attended to the content of the participant‐generated photographs in conjunction with the narrative produced by participants' during the PEI.24, 25, 26 Using a “layered approach,”24, 25, 26 2 members of the research team (GBA and KC) independently read the 10 interview transcripts alongside a total of 126 participant‐generated photographs, and performed an inductive data analysis. A theoretical orientation to materiality structured both GBA and KC's analytical work.12, 13This meant that they attended to both the human and nonhuman materials and equipment used in tube feeding, and how these were enmeshed in patients' and family caregiver's HEN activities. GBA and KC then met to discuss their independently derived codes and were refined through reaching consensus in the development of a code book. Transcripts were then entered into the qualitative analysis software (Nvivo 11 QSR International Pty Ltd.) for data management and analysis. Findings reported here are self‐report from patients and caregivers as well as caregivers' accounts of patients' experiences.
Table 1.
Layered analysis of patients' and caregivers' experiences
| Stage | Process | Purpose |
|---|---|---|
| 1 | Initial preview of each photograph and related interview transcript, moving repeatedly between transcript and photographs for each participant on a case‐by‐case basis | Seek an understanding of participants' intended representations and how they site themselves within the content of the photograph |
| 2 | Thorough and detailed review of participants' interpretations of their photographs and the context in which they were produced | Develop understanding of patients' and caregivers' tube feeding experiences in the “home” environment. |
| 3 | Reflexive and repetitive constant comparison of the entire photographic collection and interviews in which photographs were tentatively coded and then recategorized with increasing refinement | Code data and emergent themes. Clarify inconsistencies between what we were seeing in the photographs and the participants' narratives |
| 4 | An interpretation of the categories in relation to appropriate theory | We used a sociomaterial perspective, focusing on the human and nonhuman aspects of tube feeding at home for patients and caregivers. |
Adapted from: Balmer, C., F. Griffiths, and J. Dunn, A ‘new normal’: Exploring the disruption of a poor prognostic cancer diagnosis using interviews and participant‐produced photographs. Health. 2015; 19 451–472
3. RESULTS
3.1. Participants
Ten patients and 8 family caregivers took part in the study. Patients' (males = 6) mean age was 58.9 (range 30‐85), with 5 being diagnosed with malignancy, 4 with amyotrophic lateral sclerosis, and 1 with diabetes and Parkinson's disease. All patients stated that they were either on HEN indefinitely or until their condition improved sufficiently so they could sustain themselves using oral nutrition. Caregiver (males = 4) relationships to the patients included mother (1), daughters (2), and spouses (5). All participants were white, non‐Hispanic.
3.2. Findings
The PEI facilitated a highly reflexive conversation between patients, caregivers, and interviewer. Narratives and photographic analysis yielded insights into patient and caregiver experiences with HEN, including how they overcame misconceptions and accepted HEN, how the caregiver's role was reconfigured toward assisting with the logistics of providing HEN, and how complications were managed. Findings presented reflect both individual and collaborative dialogic accounts of patient and caregiver experiences of their daily lives around tube feeding, and in some circumstances, caregivers' comments describe patient's experiences.
3.3. Accepting home enteral nutrition
When HEN was initially broached, patients experienced both favorable and unfavorable reactions. Some felt a big relief for this new way of feeding, while others experienced fear. Most participants mentioned that they had heard negative things about tube feeding or had negative perceptions about HEN and how it works. Many described fear of unknown complications and/or losing their independence in caring for themselves. This often resulted in resistance to HEN and was noted in comments by both patients and caregivers.
“I think it's me, I wanted to be in charge” (patient).
“I was scared at first because he's a diabetic and I was afraid he wouldn't heal [from the surgical placement of the enteral tube]” (caregiver).
However, with education delivered by the HEN team regarding tube feeding and its benefits, those perceptions diminished:
“Once I understood that it was actually a tube that they could put in here as opposed to putting something down my nose and down my throat which would be sticking out … And once I understood that, I was yes to it” (patient).
For many patients, this education was such a significant turning point that it left an impression even about the exam room where they received education about HEN:
“That's the room [pointing to a photo of an exam room] I think that they actually had talked to me about the tube feeding and explained to me where it made sense to me and that's where I made my aha! decision” (patient).
Although there was variable length of time for each participant to accept HEN, participants ultimately characterized HEN as essential and life‐saving. All participants described how tube feeding provided “peace of mind.” Patients and caregivers depicted HEN as their new normal. For example, 1 patient took a photo of her pre‐HEN food juxtaposed with a can of formula on a plate (Figure 1A), and during the PEI, the patient explained that she did not care for a piece of burger and instead accepted the HEN liquid formula as a meal and as the new normal: “at this point it doesn't really matter to me … because I have no appetite so I don't really care” [patient]. One caregiver joked about their new normal by taking pictures of cooking a regular meal, something that she no longer had to do for the HEN patient (Figure 1B):
“I just thought, ‘well there's no more cooking involved, we got that going for us” (caregiver).
Figure 1.
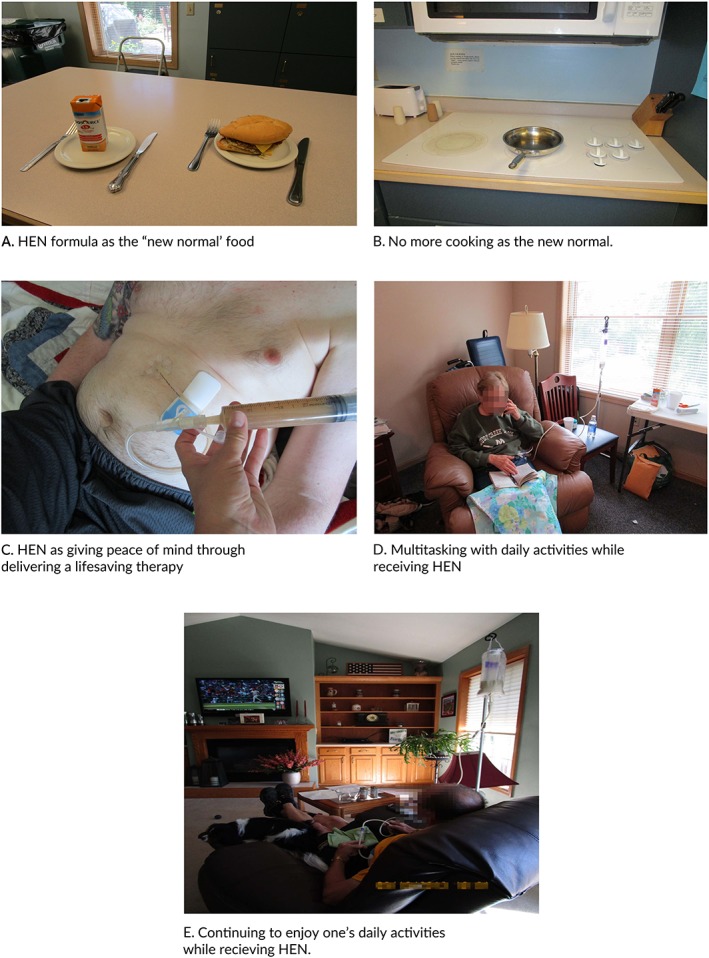
Theme: Accepting home enteral nutrition
In their interviews, participants framed tube feeding as a way to obtain life‐sustaining nutrients and calories, maintain weight and hydration, and to stay healthy. Knowing that they can administer food, medication, and other nutritional supplements via the tube which cannot be given orally gave both patients and caregivers a sense of relief and peace of mind. The centrality of the tube to this peace of mind was frequently depicted in close‐up photographs showing the tube in use with formula or medications (Figure 1C):
“Honestly, it's peace of mind; it's you know, something's not gonna taste good … but he should … have it. [You can] squish it through his tube. We kind of look at it as an advantage. So for me, it's a lot less stress and I think it is for [patient] too” (caregiver).
In their photographs and interviews, patients and caregivers described how they learned quickly to fit the tube feeding into their daily routines, and that this involved multitasking (Figure 1D) and engaging in the same daily activities that one enjoyed before HEN (Figure 1E):
“I'm talking on the phone … writing in my journal” (patient).
“He can watch TV, he can read the paper, he can sit and hold his dog … it doesn't stop you from doing what you wanna do” (caregiver).
Indicating the centrality of family care to the success of HEN as a therapeutic option, a key component of a patient's eventual acceptance of HEN was, in fact, acceptance by family members and caregivers. Family member acceptance often served as a prelude to a patient's ability to confront and plan for their future.
3.4. Duty to care
Families were repeatedly portrayed in photographs (Figure 2A‐D) administering feeds, or being engaged in intimate family social life while the HEN patient was tube feeding. Highlighting the strength of the family as a social unit in HEN experiences (rather than the HEN patient alone), families were often described in interviews through the use of plural pronouns (“we” and “our”):
“we make everything pretty much family oriented, except for bathroom duties” (caregiver, Figure 2A).
Figure 2.
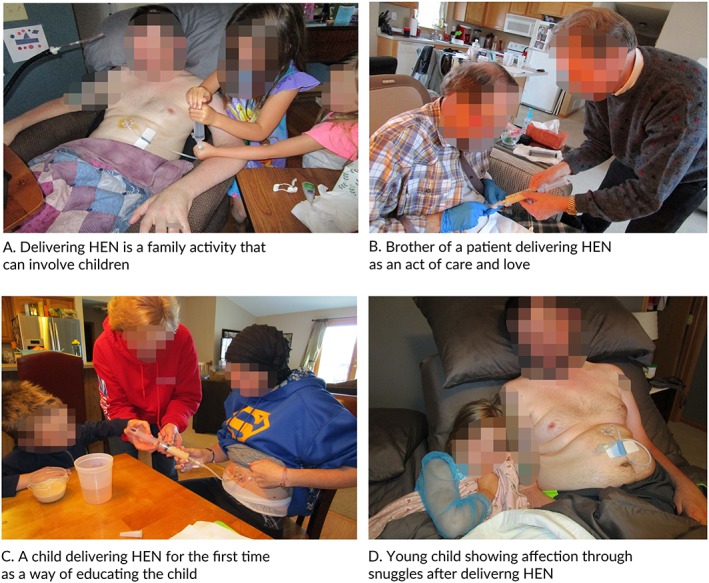
Theme: Duty to care
Together, they accepted and became engaged in the process of coping with HEN, which included collective adjustment to new routines and looking for ways to make HEN work. For instance, caregivers described having a sense of duty toward a patient's care, indicative of an unquestioning commitment to the patient, which in many cases echoes the unspoken duty to care within families and close relationships. Patients acknowledged the critical role of their family and shared their gratitude:
“I guess I don't know how people can do it alone. I just have such a good support system and a good family and good friends. They've really stepped up; they keep calling and texting and messaging and it's just an overwhelming experience of love and God shining through.”
Figures 2A‐D portray how tube feeding is integrated into family and social life and the degree of family involvement in HEN. Also, the photos reveal the degree to which family members interface with, or use, the medical material artifacts of tube feeding, and how much some patients want to involve caregivers even when they do not have the need. For example, while talking about his photograph depicting his brother feeding him (Figure 2B), 1 patient described his gratitude for his brother's feeding of him, even though he could have done it by himself:
“That's my brother … I'm just sitting there, I'm comfortable. He′s hooking it up, I can do it myself but he was doing it for me” (patient).
Both HEN patients (Figure 2C) and caregivers (Figure 2D) described an unintended benefit of involving family members in HEN care, especially involving children, as they enjoyed helping with tube feeding and, therefore, helping the patient:
“this is the first night we went to go see my nephew, and we pretended him (sic) to feed my belly. So he was all into that” (patient, Figure 2C).
“I thought it was a very sweet moment and the tube does not interfere with anything showing love or, you know, their affection. She helped feed dad and now she sat down with him to snuggle” (caregiver, Figure 2D).
The caregiver role varied depending on how much the patient could do, what they needed assistance with, or how much involvement patients wanted in their care. Both photographs and interview narratives revealed that caregivers' physical tasks included helping prepare and deliver the tube feeding or cleaning equipment after a feed. More broadly, it also included accompanying the patient to appointments and assistance with getting dressed. Despite the hardships associated with caregiving, many family caregivers were able to provide emotional support for the patients including making jokes, which helped with accepting the situation and adjusting to the new daily routines.
3.5. Devising a system that works
Tube feeding at home was characterized as something that needed planning. Patients and caregivers devised systems that used both medical and household items arranged in such a way that they were easily accessible, or “assembled in readiness.” Such sociomaterial assemblages involved collecting and ordering feeding tubes, food, charts, cookie sheets, and other household materials to provide an orderly structure that facilitated the sequential steps required to tube feed (Figure 3A‐C). The photographs depicting the assembly of materials reveal the material work of patients and caregivers doing tube feeding.
Figure 3.
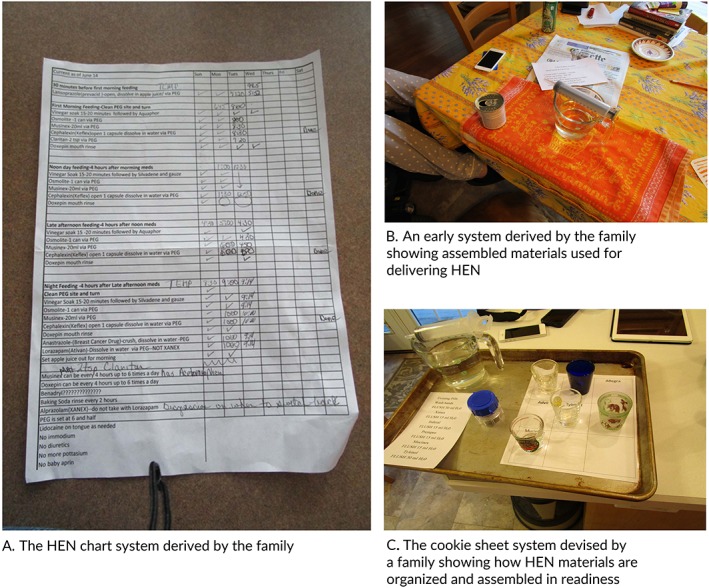
Theme: Devising a system that works
Each patient‐caregiver dyad created unique sociomaterial assemblages that worked for them, with regard to feed location, feed coordination and scheduling, and the post feed ritual of flushing the tube after feeding. Patients and caregivers described how their routine evolved and was refined with their growing experience over time. For example, 1 family initially used an index card system to schedule and coordinate feedings, but that later evolved into a more elaborate chart (Figure 3A) that was used to identify the timing and quantity of feedings. This chart was photographed and described by 1 caregiver:
“Since there's 4 of us that sort of, ah, go over to mom's house … each day, we know we're doing the right thing at the right time … You know it tells us exactly mom needs to have her neck soaked, [or] she's gonna be having a can of osmolite, [or] now she's gonna take this … we've all gone through the training, everybody knows what they're doing. It means a lot because we, gotta have that organization to bring her from where she's at. So you know that's why [we're] all really committed you know like we're each going over once a day … following this [chart] … To follow through and make sure she heals” (caregiver).
Another family described a feeding system that began with a series of household items, including a table cloth, shot glass, measuring cup, and a syringe (Figure 3B):
“..the start of our process, um we used [a] step‐by‐step basis. When you're just starting out with this, it's nice to have a checklist, ah, after a while you get it down pretty good” (caregiver).
This approach subsequently evolved into the use of a “cookie sheet system” (Figure 3C) which presented new materials deemed more useful and appropriate that were structured in a more organized and efficient way. This system was photographed by a caregiver and described as follows:
“… [that] photo there is sort of the evolution of this basic system where I just printed off a grid and we use a cookie sheet to move it around … the mechanics are a little easier … because of the spout on it, it makes it an easy place to park the syringe when you're not using it, it sits there easily” (caregiver).
The caregiver described how the cookie sheet system also allowed caregivers to enroll support from other family members as it was easy to understand and served as a training tool for other family members to become caregivers.
“… it's easy to have them on a cookie sheet and an unanticipated benefit is that … if somebody comes, in who's unfamiliar with this, it makes it easy to see how it all works” (caregiver).
Thus, consistent with our material approach to the study of HEN, we find that there are a range of interactions between humans (patients and caregivers) and nonhuman materials (household items, medical equipment, documents) that produce a sociomaterial system that work for patients and caregivers alike.
3.6. Challenges of tube feeding
From a cultural anthropology standpoint, bodily orifices are considered to be particularly vulnerable points of the body that are surrounded by cultural rituals (such as eating and hygiene) that, when analyzed, reveal a culture's social structures, social relations, and practices.27 In the case of HEN, the newly created stoma (the site at which the feeding tube enters the patient's body) featured heavily in the participant‐generated photographs, and revealed intimate portrayals of the rituals of family involvement in the delivery of enteral nutrition, the additional care needed by those with severe illness, and the challenges of maintaining a healthy stoma site. Photographs and interviews conveyed both the mechanical or physical complications of the stoma site, such as a leaking tube or the tube falling out. Some HEN patients described the stoma as “sore,” “swollen,” and “infected” and reported bloating, constipation, diarrhea, and nausea which are gastrointestinal symptoms associated with tube feeding. Many participants were caught off guard by having food residue in the tube and wished to convey this to novice HEN patients and their caregivers (Figure 4A):
Figure 4.

Theme: Challenges of tube feeding
“… making sure they know it's gonna back up into the tube. I do not think that was something they [health care team] told us. We kind of figured that it would [back up], you know, with motion” (caregiver).
Similarly, some participants did not know how to respond to possible infection and wanted to warn future HEN patients of infection (Figure 4B):
“You can't let that stuff go. So, if they're wondering, ‘should I get help?’ Get the help. Don't think, ‘gee I wonder if I should call the doctor?’ No, don't call the doctor! Go to the doctor!” (caregiver).
The visual portrayals of these adverse effects in participants' photographs were often couched in the need for better education or the need to educate future HEN patients and caregivers. Participants described how adverse events were not expected and that they had to exercise judgement as to when to call for help from the clinic's HEN team or partnered infusion company. They expressed the need for greater specificity and concreteness in patient educational material about what to expect with HEN. Through narrating their own photographs, participants wanted to convey to others that certain adverse effects can only be learned from the actual HEN experience and could not necessarily be known through standard educational materials.
Despite the challenges of tube feeding, patients and caregivers portrayed HEN positively in what they are still able to do. Through their photographs and interview, participants explained that HEN did not get in the way of “showing love” in the family home and that it did not stop patients from doing what they love. Participants felt that it was very important to convey to future patients that tube feeding was feasible, could accommodate a patient's life and interests, and is not something to be feared.
4. DISCUSSION
This study offers an in‐depth understanding of HEN in the care practices that occur around the stoma site which could be used to communicate to help future HEN patients understand how HEN may help one's illness experience, including alleviating fears and negative perceptions. Although participants in the current study attested that they received comprehensive information about HEN, they identified a need for ongoing education regarding the practical logistics of doing HEN. Using a visual methodology and a theoretical approach that focuses on the materials in the home and how they are used in the daily HEN practices, patients and caregivers were enabled to portray their experiences in a comprehensive manner. This coproduction of data in the form of participant‐produced photographic images in conjunction with photo‐elicitation interviewing ensured that participants decided what, when, and how to represent their subjectivity and illness experience at home.17 This research enabled participants to control the process of image production, dissemination, and narration17 with regard to their intimate practices of HEN and related care of their stomal site. In doing so, this research produced an in‐depth understanding of how HEN patients and caregivers make sense of HEN as a medical intervention, and how it is positively managed by patients and caregivers, in spite of potential sources of complication or difficulty.
The photographs conveyed the material artifacts involved in tube feeding regimes and their social significance in how they enabled caregivers and the wider family to be involved in delivering care. The photos portray the arrangement of the feeding equipment and convey a sense of both patients' and caregivers' innovative, organized, well‐thought‐out logics that constitute their collaborative practices. The sociomaterial perspective used in this study suggests that the patterns of interaction between patients, caregivers, and HEN equipment go beyond the normative engagement with objects and educational materials.12, 13, 28, 29 It revealed that the original highly prescribed process of tube feeding changes to an innovative practice through a process of immersion in the home context with the assistance of the family. Home enteral nutrition, in fact, is not simply a medical nutritional intervention. Rather, the examples of the cookie sheet and index cards reveal that tube feedings are variously devised “systems” that emerge from the creative innovation of caregivers and patients who use medical equipment in conjunction with “everyday” material artifacts found in the home, such as cookie sheets, glassware, trays, and documents. A feeding system, like any other system, has to work. Moreover, it needs to provide enough information for safe administration of feeds, and communication between the current caregiver and the next one. Importantly, like an earlier study,9 this study also reveals that these systems were derived from the experiences of patients and their family caregivers to suit the context and availability of materials in their own homes as the chief care environment.
Social support has been widely recognized as beneficial to both the physical and mental well‐being of patients, and certain disease diagnosis (eg, cancer) have been known to bring families closer.30 The findings of this study demonstrate tube feeding as an activity that is not only dependent on an individual but entangled within and produced by an assemblage of materials, familial relationships, and social interactions. Family lives were carefully managed, and HEN resources had to be consciously mobilized. Participants, especially the caregivers, creatively devised systems that work and included photos of friends and family members who have been involved in the feeding experience. These representations show how tube feeding is integrated into family and social lives of patients which, in turn, provided additional meaning to the feeding experience, particularly for the HEN patient and for family members who were children. However, sharing the experience of HEN with the family did come with boundaries that were set by the patient or caregiver (or both) in social situations to maintain a patient's independence and privacy. Collectively, these insights can be used to orient health professionals and families to the care of HEN patients in the home context, and to the materials and relationships that are required to deliver successful HEN.
Peer‐to‐peer education has been widely recognized in behavioral research and in promoting healthy behaviors among patients.31, 32, 33, 34 In the wider context of an identified need for more HEN education material, our findings demonstrate the potential for patient‐generated and caregiver‐generated visual data to be used in the development of peer‐to‐peer educational materials. Participants provided visual images of what they would like other patients and caregivers to learn from their experiences. These images portray both undesirable effects of tube feeding and positive perspectives of HEN. This finding reiterates the importance of visual patient educational materials35, 36, 37 which enhance patient understanding when compared to text materials alone. Providers and HEN care teams may alter teaching materials to include patient‐generated and caregiver‐generated photos of HEN experiences to enhance the likelihood that education materials include relevant photos and other visual aids that reflect actual experiences of HEN.
4.1. Limitations
We are aware of some limitations of this study. Asking participants to engage in taking photographs as part of the photo‐elicitation interviewing methodology may have impacted recruitment of participants for this study, as seen by the smaller number of participants recruited and the withdrawal of consent. Nine participants who had initially enrolled and consented to the study withdrew their consent. They reported reasons as lack of interest (n = 4); patient had developed other complications related to their diagnosis, or became too ill to participate (n = 3); or discomfort with the visual aspect (n = 2). Secondly, our findings are not derived from a representative sample: the study was performed at a single tertiary referral medical center. In addition, all of the study participants were Caucasian; thus, the data may not reflect the perspectives of individuals from diverse racial or ethnic backgrounds, nor did we purposively sample for education and socioeconomic backgrounds. The use of dyadic interviews may be limiting to the data obtained, especially as caregivers tried to respond on behalf of patients.
Nonetheless, using participant‐produced photographs and photo‐elicitation interviewing is empowering for participants as they have control over image creation and meaning making,17 and yields a better recall of experiences and participants' memories and elicits longer and more comprehensive interviews.18, 19, 20 Participants' descriptions of their challenges with HEN were placed positively in the context of patients' education using photographs to show other patients what could go wrong, which could not have been possible using only interviews. The use of dyadic interviews was also helpful: in addition to helping fill in each other's gaps and memory lapses, the technique enabled caregivers to act as “prompts” or “translators” during interviews. The theoretical perspective12, 13 applied to our data highlighted the interactions between people, and material artifacts revealed how both HEN activities and participants' knowledge shaped new ways to coordinate care for tube feeding patients and the potential for new directions in patient education materials.
Our study suggests that a strong focus on a social‐material culture is needed to comprehensively understand the impact of the home on nutritional interventions, and why patients may report such diverse experiences. Awareness of how tube feeding unfolds at home, particularly the social and material interaction, contributes to an increased understanding of the different ways and variations to how HEN is accomplished by patients and their family caregivers.
4.2. Conclusion
The findings of this study emphasize the highly contextual, innovative, and unique social and material practices accomplished by both patients and family members when HEN is integrated into home life. Health professionals need to understand these intricacies and accomplishments within the home context to tailor much‐needed support and educational services to HEN patients and their families.9 The successful delivery of HEN is a shared accomplishment between HEN patients and their caregivers. Herein exists an opportunity for both HEN patients and caregivers to be involved in teaching novice families that the process of tube feeding can lend itself to family life, thus alleviating their initial fears of tube feeding. One way of doing this is to use patient‐generated and caregiver‐generated photographic material that depicts the rich, context‐specific, and intimate familial practices of successful HEN delivery in patient education material.
FUNDING
This project received an internal funding from the Care Experience Program within Mayo Clinic's Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery.
CONFLICT OF INTEREST
The authors declare no conflict of interests.
AUTHOR CONTRIBUTIONS
Conceptualization: Drs. Manpreet Mundi, Ryan Hurt, Katherine Carroll, Joan Griffin
Formal analysis: Drs. Gladys Asiedu, Katherine Carroll
Funding acquisition: Drs. Manpreet Mundi, Ryan Hurt, Katherine Carroll, Joan Griffin
Investigation: Drs. Manpreet Mundi, Katherine Carroll, Gladys Asiedu
Methodology: Drs. Manpreet Mundi, Katherine Carroll, Gladys Asiedu
Software: Drs. Katherine Carroll, Gladys Asiedu
Visualization: Drs. Manpreet Mundi, Katherine Carroll, Gladys Asiedu
Writing original draft preparation: Drs. Manpreet Mundi, Gladys Asiedu, Katherine Carroll, Joan Griffin, Ryan Hurt
Writing—review, and editing: Drs. Manpreet Mundi, Gladys Asiedu, Katherine Carroll, Joan Griffin, Ryan Hurt
Asiedu GB, Carroll K, Griffin JM, Hurt RT, Mundi M. Home enteral nutrition: Use of photo‐elicitation to capture patient and caregiver experiences. Health Sci Rep. 2018;1:e56 10.1002/hsr2.56
REFERENCES
- 1. Klek S, Hermanowicz A, Dziwiszek G, et al. Home enteral nutrition reduces complications, length of stay, and health care costs: Results from a multicenter study. Am J Clin Nutr. 2014;100(2):609‐615. [DOI] [PubMed] [Google Scholar]
- 2. McClave SA, Taylor BE, Martindale RG, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). J Parenter Enteral Nutr. 2016;40(2):159‐211. [DOI] [PubMed] [Google Scholar]
- 3. Seres DS, Valcarcel M, Guillaume A. Advantages of enteral nutrition over parenteral nutrition. Ther Adv Gastroenter. 2013;6(2):157‐167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Weimann A, Braga M, Harsanyi L, et al. ESPEN guidelines on enteral nutrition: Surgery including organ transplantation. Clin Nutr. 2006;25(2):224‐244. [DOI] [PubMed] [Google Scholar]
- 5. Brotherton A, Abbott J, Aggett P. The impact of percutaneous endoscopic gastrostomy feeding upon daily life in adults. J Hum Nutr Diet. 2006;19(5):355‐367. [DOI] [PubMed] [Google Scholar]
- 6. Cawsey SI, Soo J, Gramlich LM. Home enteral nutrition: Outcomes relative to indication. Nutr Clin Pract. 2010;25(3):296‐300. [DOI] [PubMed] [Google Scholar]
- 7. Dreesen M, Pironi L, Wanten G, et al. Outcome indicators for home parenteral nutrition care: Point of view from adult patients with benign disease. JPEN J Parenter Enteral Nutr. 2015;39(7):828‐836. [DOI] [PubMed] [Google Scholar]
- 8. McClave SA, Chang WK. Complications of enteral access. Gastrointest Endosc. 2003;58(5):739‐751. [DOI] [PubMed] [Google Scholar]
- 9. Thompson CW, Durrant L, Barusch A, Olson L. Fostering coping skills and resilience in home enteral nutrition (HEN) consumers. Nutr Clin Pract. 2006;21(6):557‐565. [DOI] [PubMed] [Google Scholar]
- 10. Buse C, Martin D, Nettleton S. Conceptualising ‘materialities of care’: Making visible mundane material culture in health and social care contexts. Sociol Health Illn. 2018;40(2):243‐255. [DOI] [PubMed] [Google Scholar]
- 11. Charon R. Narrative medicine—a model for empathy, reflection, profession, and trust. Jama‐J Am Med Assoc. 2001;286(15):1897‐1902. [DOI] [PubMed] [Google Scholar]
- 12. Fenwick T. Sociomateriality in medical practice and learning: Attuning to what matters. Med Educ. 2014;48(1):44‐52. [DOI] [PubMed] [Google Scholar]
- 13. Fenwick T, Edwards R, Sawchuk P. Emerging approaches in educational research: Tracing the sociomaterial. London: Routledge; 2011. [Google Scholar]
- 14. Brownlie J, Spandler H. Materialities of mundane care and the art of holding one's own. Sociol Health Illn. 2018;40(2):256‐269. [DOI] [PubMed] [Google Scholar]
- 15. Ellis J. Family food practices: Relationships, materiality and the everyday at the end of life. Sociol Health Illn. 2018;40(2):353‐365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Clark CD. The autodriven interview: A photographic viewfinder into children's experience. Vis Sociol. 1999;14(1):39‐50. [Google Scholar]
- 17. Mannay D. Visual, narrative and creative research methods: Application, reflection and ethics. London and New York: Routledge; 2016. p.152. [Google Scholar]
- 18. Collier JJ. Photography in anthropology: A report on two experiments [in] American anthropologist. Am Anthropol. 1957;59:843‐859. [Google Scholar]
- 19. Harper D. Visualizing structure: Reading surfaces of social life. Qual Sociol. 1997;20(1):57‐77. [Google Scholar]
- 20. Harper D. Talking about pictures: A case for photo elicitation. Vis Stud. 2002;17(1):13‐26. [Google Scholar]
- 21. Harrison B. Seeing health and illness worlds—using visual methodologies in a sociology of health and illness: a methodological review. Sociol Health Illn. 2002;24(6):856‐872. [Google Scholar]
- 22. Bugos E, Frasso R, FitzGerald E, True G, Adachi‐Mejia AM, Cannuscio C. Practical guidance and ethical considerations for studies using photo‐elicitation interviews. Prev Chronic Dis. 2014;11:E189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Cox S, Drew S, Guillemin M, Howell C, Warr D, Waycott J. Guidlelines for ethical visual research methods. Melbourne: The University of Melbourne; 2014. [Google Scholar]
- 24. Balmer C, Griffiths F and Dunn J. A 'new normal': Exploring the disruption of a poor prognostic cancer diagnosis using interviews and participant‐produced photographs. Health (London) 2015; 19: 451–472, 5. [DOI] [PubMed] [Google Scholar]
- 25. Dowdall GW, Golden J. Photographs as data: Analysis of images from a mental hospital. Qual Sociol. 1989;12(2):183‐213. [Google Scholar]
- 26. Oliffe JL, Bottorff JL, Kelly M, Halpin M. Analyzing participant produced photographs from an ethnographic study of fatherhood and smoking. Res Nurs Health. 2008;31(5):529‐539. [DOI] [PubMed] [Google Scholar]
- 27. Douglas M. Purity and danger. London and New York: Routledge; 1966. [Google Scholar]
- 28. Nystrom S, Dahlberg J, Edelbring S, Hult H, Dahlgren MA. Debriefing practices in interprofessional simulation with students: A sociomaterial perspective. BMC Med Educ. 2016;16(1):148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Zuiderent‐Jerak T. Embodied interventions—interventions on bodies: experiments in practices of science and technology studies and hemophilia care. Sci Technol Hum Values. 2009;35:677‐710. [Google Scholar]
- 30. Thomsen TG, Hansen SR, Wagner L. How to be a patient in a palliative life experience? A qualitative study to enhance knowledge about coping abilities in advanced cancer patients. J Psychosoc Oncol. 2011;29(3):254‐273. [DOI] [PubMed] [Google Scholar]
- 31. Crawford J, Frisina A, Hack T, Parascandalo F. A peer health educator program for breast Cancer screening promotion: Arabic, Chinese, South Asian, and Vietnamese immigrant women's perspectives. Nurs Res Pract. 2015;2015:947245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Dew K, Chamberlain K, Hodgetts D, Norris P, Radley A, Gabe J. Home as a hybrid centre of medication practice. Sociol Health Illn. 2014;36(1):28‐43. [DOI] [PubMed] [Google Scholar]
- 33. Gozum S, Karayurt O, Kav S, Platin N. Effectiveness of peer education for breast cancer screening and health beliefs in Eastern Turkey. Cancer Nurs. 2010;33(3):213‐220. [DOI] [PubMed] [Google Scholar]
- 34. Nisbeth Jensen M, Fage‐Butler AM. Antenatal group consultations: Facilitating patient‐patient education. Patient Educ Couns. 2016;99(12):1999‐2004. [DOI] [PubMed] [Google Scholar]
- 35. Neuner‐Jehle S, Senn O, Wegwarth O, Rosemann T, Steurer J. How do family physicians communicate about cardiovascular risk? Frequencies and determinants of different communication formats. BMC Fam Pract. 2011;12(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Osmar K, Webb D. From idea to implementation: Creation of an educational picture book for radiation therapy patients. J Cancer Educ. 2015;30(1):193‐196. [DOI] [PubMed] [Google Scholar]
- 37. Tae JW, Lee JC, Hong SJ, et al. Impact of patient education with cartoon visual aids on the quality of bowel preparation for colonoscopy. Gastrointest Endosc. 2012;76(4):804‐811. [DOI] [PubMed] [Google Scholar]


