Abstract
Total hip arthroplasty through an anterior approach has been increasing in popularity amongst surgeons and patients.
Anterior approach hip arthroplasty seems to offer improved early outcomes in terms of pain, rehabilitation and length of stay.
No difference in long-term outcomes has been shown between anterior and posterior or lateral approaches.
Proper formal training, utilization of fluoroscopy and adequate experience can mitigate risks of complications and improve early and medium-term outcomes.
Cite this article: EFORT Open Rev 2018;3:574-583. DOI: 10.1302/2058-5241.3.180023.
Keywords: anterior approach, complications, hip arthroplasty, learning curve, outcomes
Introduction
The anterior approach to the hip was originally described by Carl Hueter in 1817, in his work Der Grundriss der Chirurgie. However, it was Smith-Petersen who popularized the approach in the US and the English-speaking world, after describing it in 1917. In the early 20th century, the anterior approach was regularly used to treat hip dysplasia. In the middle of the century the approach was utilized to treat femoral neck fractures and implant the first hip prostheses with varying degrees of success. Scepticism regarding inadequate exposure and the huge success of the Charnley prosthesis shifted the focus of attention towards the lateral and posterolateral approaches.1 The work of the Judet brothers and Keggi helped re-popularize the anterior approach in the 1980s. With the continued improvement of implants, outcomes and techniques, the muscle damage caused by the lateral and posterolateral approaches to the abductors and external rotators started to cause concern,2 and interest in the muscle-sparing anterior approach was renewed, with the works of Matta et al,3 Berger,4 Kennon et al,5 Siguier et al6 and others presenting excellent results and updates in technique.
In recent years a growing number of surgeons have been using the anterior approach for hip arthroplasty, as well as resurfacing and femoral neck fractures. The muscle-sparing nature of the approach and the improved early results of the anterior approach as well as the favourable dislocation rate reported have tempted many surgeons and patients to switch to the anterior approach. This has not been without criticism, however, focusing on the steep learning curve, high rate of perioperative complications, early revision rate and limited extensibility.
Materials and methods
A systematic review of the literature was conducted in Medline and the Cochrane database (Fig. 1) Searches were carried out using the following terms: “anterior approach hip”, “anterior approach total hip”, and “anterior approach hip arthroplasty”; subsequent separate searches for the subthemes were conducted using the keywords: “anterior approach hip dislocation”, “anterior approach hip fracture”, “anterior approach hip nerve”, “anterior approach hip infection”, “anterior approach hip revision”, “anterior approach hip learning curve”, and “anterior approach hip complication”. The literature search was limited to articles published in the last 20 years. The search revealed 2102 results in PubMed, and 1020 records in the Cochrane database. After title review and checking that the studies included human subjects exclusively, the search yielded 30 and 217 abstracts in the Cochrane and PubMed databases, respectively. Following abstract review a total of 78 articles were retrieved and were considered eligible for full-text review. An additional 22 articles were extracted after full-text review, whereas 12 were discarded due to ineligibility after review. Thus, a total of 88 articles were included in our systematic review.
Fig. 1.
PRISMA 2009 flow diagram.
We have divided results into potential documented advantages and disadvantages and analysed different important points separately.
Advantages
Early postoperative pain scores and patient-reported outcomes
Randomized controlled trials
The largest prospective randomized controlled trial (RCT) is that of Mjaaland et al7 who compared the immediate peri- and postoperative results of 83 anterior approach (DAA) total hip arthroplasty patients with 80 patients who underwent a lateral approach (LA). They found a significant difference in early pain scores in favour of the DAA despite increased Creatinine Kinase in the DAA group. Improved WOMAC, HHS and SF-36 scores in DAA patients compared to LA persisting up to one year postoperatively were shown in the RCT of Restrepo et al,8 who followed the patients for two years. Improved early postoperative pain scores of DAA versus LA patients were recorded by Nistor et al9 in an RCT including 25 patients per group during the learning curve of the surgeons. D’Arrigo et al,10 in an RCT, compared the DAA with the anterolateral (AL), LA and a mini LA. A six-week follow-up showed that the DAA and LA approaches were associated with significantly higher WOMAC scores. Zhao et al11 compared 60 DAA with 60 posterior approach (PA) total hip arthroplasty (THA) patients for a minimum of six months. The DAA group had improved postoperative pain scores, whereas UCLA hip score and HHS were significantly better at the three-month follow-up, but interestingly not at the final follow-up at six months. Similar were the results of another RCT by Barrett et al,12 who found the DAA to be superior to the PA in terms of early postoperative pain scores and walking distance, HHS and Hip disability and Osteoarthritis Outcome Score (HOOS) during the first three months. Improved early pain scores without difference in outcome scores between DAA and PA THA patients were reported in the RCTs of Cheng et al13 and Christensen et al,14 with the latter reporting earlier discard of walking aides in the DAA group. On the other hand the study from Rykov et al15 showed no difference in outcome scores at six weeks between DAA and PA. Furthermore, Taunton et al16 showed the mini PA being superior in terms of WOMAC and SF-12 mental scores at three-week follow-up, with the DAA patients achieving earlier ambulation without assistance. No difference was found at the later follow-up intervals.
Meta-analyses
Currently there are no large RCTs comparing the early and medium-term outcomes of different surgical approaches for THA. In the current literature the DAA seems to be superior to the LA and equal to or superior to the posterior approaches. To offset the small number of patients in the RCTs, meta-analyses have been conducted. Miller et al17 pooled data from 13 prospective comparative studies comparing the anterior and posterior approaches for short-term (three-month) outcomes, concluding that the anterior approach was superior in terms of pain scores and hip function. Similarly, Putananon et al18 conducted a meta-analysis using data from 14 RCTs showing the superiority of the anterior approach in terms of early outcomes compared to the lateral and posterior. On the contrary, Higgins et al19 in their meta-analysis of 17 studies, including both prospective and retrospective, found no significant difference in outcomes between anterior and posterior approaches. However, they found superiority of the anterior approach in terms of reduced hospitalization and dislocation rate.
Large retrospective studies
Large samples of patients are usually found in the retrospective studies, such as the one from Sibia et al20 comparing 1457 DAA THA patients with 1241 PA patients, concluding that the anterior approach demonstrated significantly higher HHS and pain relief at the three to six-month follow-up but not at one year postoperatively. Malek et al,21 on the other hand, compared 265 DAA with 183 PA THA patients, finding no significant difference in outcomes at a median follow-up of 18 months. The comparison between the anterior and lateral approach in the larger retrospective studies favours the former in terms of short-term outcome scores,22–24 whereas Alecci et al25 demonstrated improved pain scores in the anterior group.
Length of hospitalization
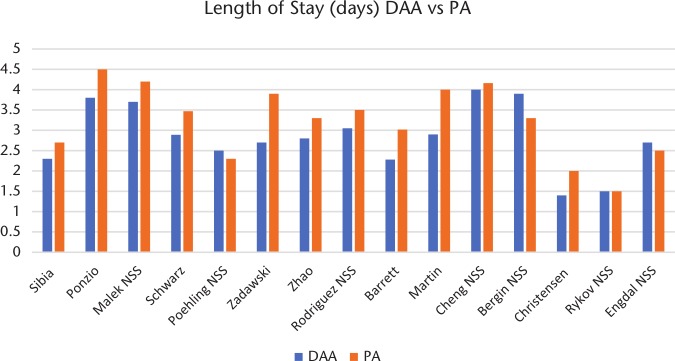
In the majority of studies the length of hospitalization of patients undergoing hip arthroplasty through an anterior approach is significantly reduced compared with their posterior approach counterparts.11–15,20,21,26–32 Results are shown in Figure 2.
Fig. 2.
Comparison of length of stay between anterior approach (DAA) and posterior approach (PA).
Note. NSS, not statistically significant.
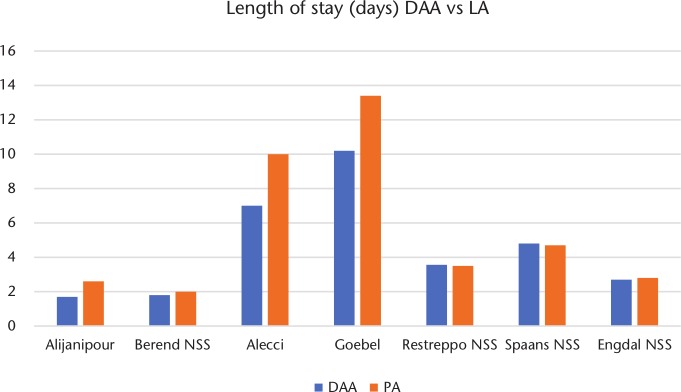
The same trend of reduced hospital stay is seen when comparing the anterior to the lateral approach; however, this comparison has not been extensively investigated in the literature (Fig. 3).8,23,25,33–36
Fig. 3.
Comparison of length of stay between anterior approach (DAA) and lateral approach (LA).
Note. NSS, not statistically significant.
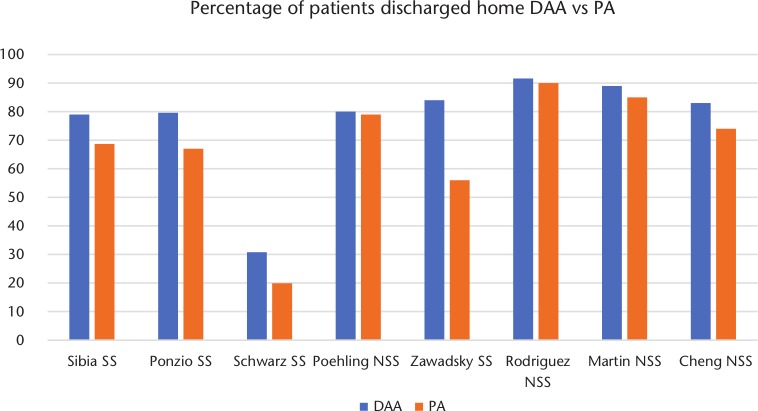
Discharge destination
The improved postoperative recovery seems to favourably affect the percentage of patients discharged to their homes versus a rehabilitation facility in the DAA patients. In the largest series to date comparing discharge destination between DAA and PA patients, Ponzio et al26 and Sibia et al20 report significantly higher percentages of DAA THA patients being discharged home compared to PA THA patients. The same trend is seen in the literature13,27–31 without reaching statistical significance in series with smaller numbers of patients. The same is the case for DAA THA patients compared to LA THA in the series of Berend23 and Alecci25 (Fig. 4).
Fig. 4.
Comparison of discharge destination between anterior approach (DAA) and posterior approach (PA).
Note. NSS, not statistically significant; SS, statistically significant.
Dislocations
The reported dislocation rate for the anterior approach has been consistently low in the literature. Barnett et al,37 in the largest published series of DAA comprising 5090 cases, report a dislocation rate of 0.23%. Similarly, the Anterior Total Hip Arthroplasty Collaborative Investigators38 in another multi-centre study report a 0.6% rate of dislocation in a series of 1277 THA. Sariali et al39 in 1764 cases demonstrated a dislocation rate of 1,5%; however, only 0.11% required revision surgery. Cidambi et al40 and Mirza et al41 have similar results with a rate of 0.2% in 1120 cases and 0.4% in 1035 cases, respectively. Most of the dislocations in the anterior approach patients tend to happen in the first three to four weeks postoperatively, as shown by Siguier et al6 and Tamaki et al,42 who report that 60% and 75% of dislocations respectively occurred in the first month. The meta-analyses of Lee and Marconi43 and de Geest et al44 show similar findings, with 1.2% and 0.6% of dislocations in DAA THA patients. Sheth et al45 report in a registry study a lower dislocation rate for the anterior and anterolateral approaches compared to the posterior approach.
Soft tissue damage and gait analysis
The muscle-sparing nature of the anterior approach to the hip has been considered one of its main advantages. However, the evaluation of muscle damage and its clinical sequelae has not been so consistent with this theoretical advantage. In a cadaveric study comparing the anterior and posterior approaches, Meneghini et al46 found significantly more damage caused to the rotators, piriformis and gluteus minimus in the posterior approach specimens, and muscle damage caused at the tensor fascia lata and rectus femoris in the anterior approach specimens. The authors report that the piriformis muscle was transected in 50% of the anterior cases to gain access to the femur, a rate that we have not encountered elsewhere, and which depends on the surgeon’s experience and technique. Biochemical markers have been used to detect the levels of muscle damage in a series of studies comparing the anterior to the posterior approach.11,15,32,47,48 The trend was for DAA patients to have lower perioperative values of Creatine Kinase (CK), C-reactive Protein (CRP), Interleukin-6 (IL-6) and lower postoperative pain scores; however, these comparisons did not always reach statistical significance. The RCTs of Mjaaland et al and De Anta-Díaz et al compare the effect of anterior versus lateral approach on muscle damage. Mjaaland et al7 find higher postoperative CK values in the DAA group but at the same time lower visual analogue pain scores. De Anta-Díaz et al49 reported lower postoperative values of CK, IL-6, CRP and Erythrocyte Sedimentation Rate (ESR in the anterior group. Similarly, the anterior approach led to lower postoperative myoglobin values compared to the lateral in an RCT by Nistor et al.9 These findings clearly demonstrate the effect of the surgeon’s skill on the potential muscle damage and possibly question their associated clinical significance. Postoperative pain and recovery speed better reflect the damage of the soft tissue envelope.
Correlation of muscle damage with MRI studies has shown significantly higher rates of gluteus medius and minimus fatty atrophy in lateral approach patients at six months and one year postoperatively,49,50,51 whereas posterior approach patients predictably displayed higher muscle atrophy in the hip rotators.50 The potential effect of the anterior approach on the tensor fascia lata (TFL) is somewhat disputed, with one study49 showing thinning of the TFL, whereas another showed no damage.51
Gait analysis laboratories have been used in recent studies to evaluate the effect of surgical approach on gait patterns. The anterior approach is shown to have improved early rotation range of motion (ROM)52 and pelvic tilt closer to normal53 compared to the posterior, but no clinically significant differences seem to emerge.36,54 Similarly, comparison of the anterior and lateral/anterolateral approaches in postoperative gait patterns show that the anterior approach has some advantages in terms of velocity,55,56 and closer to normal gait parameters.53,57,58 The ultimate clinical effect of gait pattern alteration remains unclear, as well as the optimal way to evaluate the effect of surgical approach on muscle tissue.
Simultaneous bilateral procedures
The perioperative safety of same-day bilateral THA (BTHA) surgery compared to staged BTHA within one year has been shown in the largest series from Poultsides et al,59 with 1946 same-day bilateral THA (973 patients) with comparable complication rates to staged bilateral procedures. Tamaki et al60 also report low complication rates in 325 patients undergoing 650 THA. The only published series comparing the anterior and posterior approaches in bilateral THA is that from Watts et al,61 in their retrospective analysis of 40 patients undergoing bilateral THA (19 DAA, 21 PA). The authors found no significant difference in complication rates; operative and anaesthesia times were significantly higher in the DAA group. On the contrary, a significantly higher percentage of DAA patients were discharged home.
Ease of fluoroscopy use
One of the big advantages of the anterior approach is the unencumbered use of intraoperative fluoroscopy. The effect of fluoroscopy in adequate cup positioning has been clearly demonstrated in terms of reducing abduction and version outliers.11,30,62–64
Hip resurfacing
The anterior approach can be utilized even in hip resurfacing as demonstrated by Benoit et al65 and Kreuzer et al.66 The advantages are the preservation of femoral head vascularity by sparing the medial femoral circumflex artery (MFCA), combined with the lack of associated morbidity of trochanteric osteotomy compared to surgical hip dislocation. Benoit et al65 reported no need to convert to an extensile approach or early revisions in their series; however, the DAA patients had significantly more cups with an increased angle than the surgical dislocation cohort, although none over 55 degrees. Both authors recommend that a surgeon experienced in DAA THA should undertake this type of procedure.
Disadvantages
Proximal and distal extension of the skin incision
One of the major points of criticism of DAA is the potentially limited extensibility and possible obscure intraoperative exposure. In a cadaveric study, Grob et al67 found that the distal extension between TFL and vastus lateralis (VL) endangers the transverse and descending branches of the lateral femoral circumflex artery (LFCA) along with their accompanying motor branches for VL and vastus intermedius (VI), cautioning against possible denervation of these two muscles. The authors advocated using the subvastus approach to pass cerclage wires as a safer route for the neurovascular structures. Ghijselings et al68 conducted a cadaveric anatomical study and demonstrated that the position of the distal neurovascular bundles is, for the most part, stable in reference to anatomical landmarks, and predictable. They concluded that distal extension is feasible and proximal femoral cerclage wiring can be safely performed. Nogler and Thaler69 in their cadaveric study showed that by dividing the iliotibial band and utilizing the subvastus rather than the intervastus approach, a safe distal access can be easily achieved. The proximal aspect of the approach can be easily extended utilizing the originally described Smith-Petersen approach. This approach has been successfully used, especially in complex revision cases where reconstruction of anterior and medial wall defects was deemed necessary.70
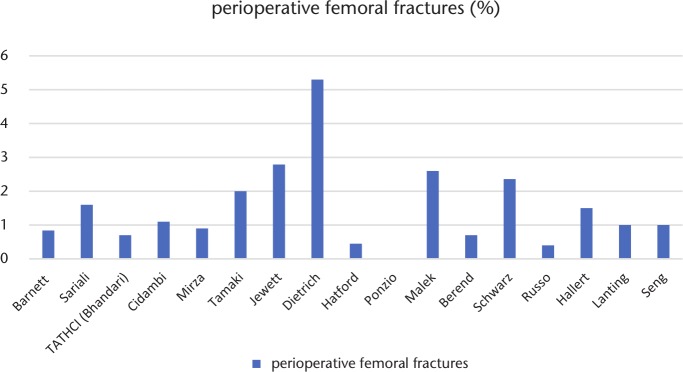
Intraoperative complications during the learning curve
Another major point of criticism of the anterior approach is the high complication rate, especially early in the learning curve of the approach. Most notably, intraoperative fractures have been related with difficulty in exposing and manipulating the femur during femoral stem preparation (Fig. 5). Based on the current literature the rates of intraoperative femoral fractures range from 0% to 5.3%.21,23,24,26,27,37–41,71–77 There is a trend for lower incidence for larger volume centres and surgeons. Recent meta-analyses of DeGeest et al44 and Lee et al43 report rates of 1.3% and 2.3%, respectively. Comparing the intraoperative facture rate between anterior, posterior and lateral approaches in the last years the majority of studies do not demonstrate a statistically significant difference,11,23,25–27,30,35,62,78 although there is a trend for higher rates in the anterior approach. Malek et al21 found significantly higher fracture rates in the DAA group compared to the posterior approach patients. The majority of these fractures do not necessitate further action or are dealt with using intraoperative cerclage wiring or longer stems in cases of diaphyseal involvement. It is noteworthy that perioperative complications seem to be surgeon-related, as shown by the multi-centre study of the Anterior Total Hip Arthroplasty Collaborative Investigators, and several other articles focusing on the learning curve effect. The definition of the learning curve is relatively elusive; reports claim the first 25,79 36,24 50,25,29,76 60,80 or 100 cases81 as the cut-off point for reduction in complications and operative time. In a single surgeon series of 500 DAA THAs, Hartford and Bellino found no difference after the 100 cases, but noted a change in complications from 5% (9% fractures) in the first hundred to 2% (1% fractures) in the last hundred cases.74 Other studies support that the combination of an experienced hip surgeon and proper use of fluoroscopy may not increase the complication rate during the learning curve period.81,82
Fig. 5.
Perioperative femoral fractures.
Early mechanical complication and cementing technique
Early revision due to femoral stem under-sizing and inadequate femoral stem positioning and fixation have been associated with the anterior approach, especially early on in the learning curve, possibly due to inadequate exposure and visibility.38,44,81,83,84 Ponzio et al,26 on the other hand, found a reduced rate of early revision compared to the posterior approach in a retrospective study of 4538 THA cases, interestingly including the learning curve in the anterior hip group. The Anterior Total Hip Arthroplasty Collaborative Investigators,38 in a multi-centre study of 1277 DAA THA cases, report an early revision rate of 2.7%, of which 1.3% is attributed to femoral loosening, and note that there was a significant correlation between surgeon and early revision. The adequacy of the exposure even for cementation has been demonstrated in a cadaveric study by Mayr et al,85 who found no difference in cement mantle between the lateral and the anterior approach.
As for the femoral component positioning, varus implantation has been reported in as many as 7.5% of cases82 during the learning curve, but there does not seem to be a difference in comparison to posterior or lateral approaches,35,63 and in some studies significantly better stem positioning has been achieved with the anterior approach,12 possibly due to the intraoperative use of fluoroscopy.
Surgical site infection and role of obesity
Some concern has arisen regarding wound complications in patients treated with DAA, especially in obese patients. Watts et al86 report similar rates of wound complications between DAA (1.7%) and PA (1.9%) patients. The authors note that obesity had a significantly negative effect on wound complications in the DAA group. In line with the aforementioned study, Russo et al75 found a significantly increased risk for wound and/or any major complication in obese DAA patients compared with non-obese patients. On the contrary, Purcell et al,87 in a retrospective study of 4651 patients, found no difference in infection rates and wound complications between obese DAA and obese PA patients, although obese patients had a significantly higher probability of wound complications than non-obese patients in both groups.
Conclusion
The anterior approach to the hip is a safe, muscle-sparing, and fully extensible approach offering potentially great short and medium-term advantages in total hip arthroplasty patients. No study to date has demonstrated a benefit in the long-term survivorship and outcomes of direct anterior THA over posterior or lateral approaches. Nonetheless the early outcomes are making the approach increasingly attractive and popular to both surgeons and patients, especially in light of the tendency to underplay the potential risks in favour of the benefits that was observed in a recent survey amongst US surgeons.88 As with most minimally invasive surgical techniques, a great deal of training and skill is required in order to be able to enjoy the advantages and avoid the potentially catastrophic complications. The learning curve is inevitable, as with any new skill or technique, and the early results appear to be surgeon-dependent. We believe that surgeon’s experience, didactic cadaveric workshops and formal training either in the form of fellowships or extended visits to centres and surgeons specializing in the technique, together with the use of intraoperative fluoroscopy, mitigate the risks for early complication and improve short- and medium-term outcomes.
Footnotes
ICMJE Conflict of interest statement: None declared.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Rachbauer F, Kain MSH, Leunig M. The history of the anterior approach to the hip. Orthop Clin North Am 2009;40:311–320. [DOI] [PubMed] [Google Scholar]
- 2. Masonis JL, Bourne RB. Surgical approach, abductor function, and total hip arthroplasty dislocation. Clin Orthop Relat Res 2002;405:46–53. [DOI] [PubMed] [Google Scholar]
- 3. Matta JM, Shahrdar C, Ferguson T. Single-incision anterior approach for total hip arthroplasty on an orthopaedic table. Clin Orthop Relat Res 2005;441:115–124. [DOI] [PubMed] [Google Scholar]
- 4. Berger RA. Total hip arthroplasty using the minimally invasive two-incision approach. Clin Orthop Relat Res 2003;417:232–241. [DOI] [PubMed] [Google Scholar]
- 5. Kennon RE, Keggi JM, Wetmore RS, Zatorski LE, Huo MH, Keggi KJ. Total hip arthroplasty through a minimally invasive anterior surgical approach. J Bone Joint Surg Am 2003;85-A Suppl 4:39–48. [DOI] [PubMed] [Google Scholar]
- 6. Siguier T, Siguier M, Brumpt B. Mini-incision anterior approach does not increase dislocation rate: a study of 1037 total hip replacements. Clin Orthop Relat Res 2004;426:164–173. [DOI] [PubMed] [Google Scholar]
- 7. Mjaaland KE, Kivle K, Svenningsen S, Pripp AH, Nordsletten L. Comparison of markers for muscle damage, inflammation, and pain using minimally invasive direct anterior versus direct lateral approach in total hip arthroplasty: a prospective, randomized, controlled trial. J Orthop Res 2015;33:1305–1310. [DOI] [PubMed] [Google Scholar]
- 8. Restrepo C, Parvizi J, Pour AE, Hozack WJ. Prospective randomized study of two surgical approaches for total hip arthroplasty. J Arthroplasty 2010;25:671–679. [DOI] [PubMed] [Google Scholar]
- 9. Nistor DV, Caterev S, Bolboacă SD, Cosma D, Lucaciu DOG, Todor A. Transitioning to the direct anterior approach in total hip arthroplasty. Is it a true muscle sparing approach when performed by a low volume hip replacement surgeon? Int Orthop 2017;41:2245–2252. [DOI] [PubMed] [Google Scholar]
- 10. D’Arrigo C, Speranza A, Monaco E, Carcangiu A, Ferretti A. Learning curve in tissue sparing total hip replacement: comparison between different approaches. J Orthop Traumatol 2009;10:47–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Zhao HY, De Kang P, Xia YY, Shi XJ, Nie Y, Pei FX. Comparison of early functional recovery after total hip arthroplasty using a direct anterior or posterolateral approach: a randomized controlled trial. J Arthroplasty 2017;32:3421–3428. [DOI] [PubMed] [Google Scholar]
- 12. Barrett WP, Turner SE, Leopold JP. Prospective randomized study of direct anterior vs postero-lateral approach for total hip arthroplasty. J Arthroplasty 2013;28:1634–1638. [DOI] [PubMed] [Google Scholar]
- 13. Cheng TE, Wallis JA, Taylor NF, et al. A prospective randomized clinical trial in total hip arthroplasty: comparing early results between the direct anterior approach and the posterior approach. J Arthroplasty 2017;32:883–890. [DOI] [PubMed] [Google Scholar]
- 14. Christensen CP, Jacobs CA. Comparison of patient function during the first six weeks after direct anterior or posterior total hip arthroplasty (THA): a randomized study. J Arthroplasty 2015;30:94–97. [DOI] [PubMed] [Google Scholar]
- 15. Rykov K, Reininga IHF, Sietsma MS, Knobben BAS, ten Have BLEF. Posterolateral vs direct anterior approach in total hip arthroplasty (POLADA Trial): a randomized controlled trial to assess differences in serum markers. J Arthroplasty 2017;32:3652–3658.e1. [DOI] [PubMed] [Google Scholar]
- 16. Taunton MJ, Mason JB, Odum SM, Springer BD. Direct anterior total hip arthroplasty yields more rapid voluntary cessation of all walking aids: a prospective, randomized clinical trial. J Arthroplasty 2014;29(suppl):169–172. [DOI] [PubMed] [Google Scholar]
- 17. Miller LE, Gondusky JS, Bhattacharyya S, Kamath AF, Boettner F, Wright J. Does surgical approach affect outcomes in total hip arthroplasty through 90 days of follow-up? A systematic review with meta-analysis. J Arthroplasty 2018;33:1296–1302. [DOI] [PubMed] [Google Scholar]
- 18. Putananon C, Tuchinda H, Arirachakaran A, Wongsak S, Narinsorasak T, Kongtharvonskul J. Comparison of direct anterior, lateral, posterior and posterior-2 approaches in total hip arthroplasty: network meta-analysis. Eur J Orthop Surg Traumatol 2018;28:255–267. [DOI] [PubMed] [Google Scholar]
- 19. Higgins BT, Barlow DR, Heagerty NE, Lin TJ., Anterior vs. posterior approach for total hip arthroplasty: a systematic review and meta-analysis. J Arthroplasty 2015;30:419–434. [DOI] [PubMed] [Google Scholar]
- 20. Sibia US, Turner TR, MacDonald JH, King PJ. The impact of surgical technique on patient reported outcome measures and early complications after total hip arthroplasty. J Arthroplasty 2017;32:1171–1175. [DOI] [PubMed] [Google Scholar]
- 21. Malek IA, Royce G, Bhatti SU, et al. A comparison between the direct anterior and posterior approaches for total hip arthroplasty: the role of an ‘enhanced recovery’ pathway. Bone Joint J 2016;98–B:754–760. [DOI] [PubMed] [Google Scholar]
- 22. Amlie E, Havelin LI, Furnes O, et al. Worse patient-reported outcome after lateral approach than after anterior and posterolateral approach in primary hip arthroplasty: a cross-sectional questionnaire study of 1,476 patients 1–3 years after surgery. Acta Orthop 2014;85:463–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Berend KR, Lombardi AV, Seng BE, Adams JB. Enhanced early outcomes with the anterior supine intermuscular approach in primary total hip arthroplasty J Bone Joint Surg [Am] 2009;91(suppl 6):107–120. [DOI] [PubMed] [Google Scholar]
- 24. Seng BE, Berend KR, Ajluni AF, Lombardi AV. Anterior-supine minimally invasive total hip arthroplasty: defining the learning curve. Orthop Clin North Am 2009;40:343–350. [DOI] [PubMed] [Google Scholar]
- 25. Alecci V, Valente M, Crucil M, Minerva M, Pellegrino CM, Sabbadini DD. Comparison of primary total hip replacements performed with a direct anterior approach versus the standard lateral approach: perioperative findings. J Orthop Traumatol 2011;12:123–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ponzio DY, Poultsides LA, Salvatore A, Lee YY, Memtsoudis SG, Alexiades MM. In-hospital morbidity and postoperative revisins after direct anterior vs posterior total hip arthroplasty. J Arthroplasty 2018;33:1421–1425.e1. [DOI] [PubMed] [Google Scholar]
- 27. Schwartz BE, Sisko ZW, Mayekar EM, Wang OJ, Gordon AC. Transitioning to the direct anterior approach in total hip arthroplasty: is it safe in the current health care climate? J Arthroplasty 2016;31:2819–2824. [DOI] [PubMed] [Google Scholar]
- 28. Poehling-Monaghan KL, Kamath AF, Taunton MJ, Pagnano MW. Direct anterior versus miniposterior tha with the same advanced perioperative protocols: surprising early clinical results. Clin Orthop Relat Res 2014;473:623–631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Zawadsky MW, Paulus MC, Murray PJ, Johansen MA. Early outcome comparison between the direct anterior approach and the mini-incision posterior approach for primary total hip arthroplasty: 150 consecutive cases. J Arthroplasty 2014;29:1256–1260. [DOI] [PubMed] [Google Scholar]
- 30. Rodriguez JA, Deshmukh AJ, Rathod PA, et al. Does the direct anterior approach in THA offer faster rehabilitation and comparable safety to the posterior approach? Clin Orthop Relat Res 2014;472:455–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Martin CT, Pugely AJ, Gao Y, Clark CR. A comparison of hospital length of stay and short-term morbidity between the anterior and the posterior approaches to total hip arthroplasty. J Arthroplasty 2013;28:849–854. [DOI] [PubMed] [Google Scholar]
- 32. Bergin PF, Doppelt JD, Kephart CJ, et al. Comparison of minimally invasive direct anterior versus posterior total hip arthroplasty based on inflammation and muscle damage markers. J Bone Joint Surg [Am] 2011;93:1392–1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Alijanipour P, Patel RP, Naik TU, Parvizi J. Heterotopic ossification in primary total hip arthroplasty using the direct anterior vs direct lateral approach. J Arthroplasty 2017;32:1323–1327. [DOI] [PubMed] [Google Scholar]
- 34. Goebel S, Steinert AF, Schillinger J, et al. Reduced postoperative pain in total hip arthroplasty after minimal-invasive anterior approach. Int Orthop 2012;36:491–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Spaans AJ, Van Den Hout JAAM, Bolder SBT. High complication rate in the early experience of minimally invasive total hip arthroplasty by the direct anterior approach. Acta Orthop 2012;83:342–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Engdal M, Foss OA, Taraldsen K, Husby VS, Winther SB. Daily physical activity in total hip arthroplasty patients undergoing different surgical approaches. Am J Phys Med Rehabil 2017;96:473–478. [DOI] [PubMed] [Google Scholar]
- 37. Barnett SL, Peters DJ, Hamilton WG, Ziran NM, Gorab RS, Matta JM. Is the anterior approach safe? early complication rate associated with 5090 consecutive primary total hip arthroplasty procedures performed using the anterior approach. J Arthroplasty 2016;31:2291–2294. [DOI] [PubMed] [Google Scholar]
- 38. Anterior Total Hip Arthroplasty Collaborative Investigators, Bhandari M, Matta J, et al. Outcomes following the single-incision anterior approach to total hip arthroplasty: a multicenter observational study. Orthop Clin North Am 2009;40:329–342. [DOI] [PubMed] [Google Scholar]
- 39. Sariali E, Leonard P, Mamoudy P. Dislocation after total hip arthroplasty using Hueter anterior approach. J Arthroplasty 2008;23:266–272. [DOI] [PubMed] [Google Scholar]
- 40. Cidambi KR, Barnett SL, Mallette PR, Patel JJ, Nassif NA, Gorab RS. Impact of femoral stem design on failure after anterior approach total hip arthroplasty. J Arthroplasty 2018;33:800–804. [DOI] [PubMed] [Google Scholar]
- 41. Mirza AJ, Lombardi AV, Morris MJ, Berend KR. A mini-anterior approach to the hip for total joint replacement: optimising results: improving hip joint replacement outcomes. Bone Joint J 2014;96B:32–35. [DOI] [PubMed] [Google Scholar]
- 42. Tamaki T, Oinuma K, Miura Y, Higashi H, Kaneyama R, Shiratsuchi H. Epidemiology of dislocation following direct anterior total hip arthroplasty: a minimum 5-year follow-up study. J Arthroplasty 2016;31:2886–2888. [DOI] [PubMed] [Google Scholar]
- 43. Lee GC, Marconi D. Complications following direct anterior hip procedures: costs to both patients and surgeons. J Arthroplasty 2015;30:98–101. [DOI] [PubMed] [Google Scholar]
- 44. De Geest T, Fennema P, Lenaerts G, De Loore G. Adverse effects associated with the direct anterior approach for total hip arthroplasty: a Bayesian meta-analysis. Arch Orthop Trauma Surg 2015;135:1183–1192. [DOI] [PubMed] [Google Scholar]
- 45. Sheth D, Cafri G, Inacio MCS, Paxton EW, Namba RS. Anterior and anterolateral approaches for tha are associated with lower dislocation risk without higher revision risk. Clin Orthop Relat Res 2015;473:3401–3408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Meneghini RM, Pagnano MW, Trousdale RT, Hozack WJ. Muscle damage during MIS total hip arthroplasty: Smith-Peterson versus posterior approach. Clin Orthop Relat Res 2006;453:293–298. [DOI] [PubMed] [Google Scholar]
- 47. Pilot P, Kerens B, Draijer W, et al. Is minimally invasive surgery less invasive in total hip replacement? A pilot study. Injury 2006;37S:S17–S23. [DOI] [PubMed] [Google Scholar]
- 48. Poehling-Monaghan KL, Taunton MJ, Kamath AF, Trousdale RT, Sierra RJ, Pagnano MW. No correlation between serum markers and early functional outcome after contemporary THA. Clin Orthop Relat Res 2017;475:452–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. De Anta-Díaz B, Serralta-Gomis J, Lizaur-Utrilla A, Benavidez E, López-Prats FA. No differences between direct anterior and lateral approach for primary total hip arthroplasty related to muscle damage or functional outcome. Int Orthop 2016;40:2025–2030. [DOI] [PubMed] [Google Scholar]
- 50. Agten CA, Sutter R, Dora C, Pfirrmann CWA. MR imaging of soft tissue alterations after total hip arthroplasty: comparison of classic surgical approaches. Eur Radiol 2016;27:1312–1321. [DOI] [PubMed] [Google Scholar]
- 51. Bremer AK, Kalberer F, Pfirrmann CWA, Dora C. Soft-tissue changes in hip abductor muscles and tendons after total hip replacement: comparison between the direct anterior and the transgluteal approaches. Bone Joint J 2011;93–B:886–889. [DOI] [PubMed] [Google Scholar]
- 52. Rathod PA, Orishimo KF, Kremenic IJ, Deshmukh AJ, Rodriguez JA. Similar improvement in gait parameters following direct anterior & posterior approach total hip arthroplasty. J Arthroplasty 2014;29:1261–1264. [DOI] [PubMed] [Google Scholar]
- 53. Petis S, Howard J, Lanting B, Jones I, Birmingham T, Vasarhelyi E. Comparing the anterior, posterior and lateral approach: gait analysis in total hip arthroplasty. Can J Surg 2017;60:3217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Maffiuletti NA, Impellizzeri FM, Widler K, et al. Spatiotemporal parameters of gait after total hip replacement: anterior versus posterior approach. Orthop Clin North Am 2009;40:407–415. [DOI] [PubMed] [Google Scholar]
- 55. Klausmeier V, Lugade V, Jewett BA, Collis DK, Chou LS. Is there faster recovery with an anterior or anterolateral THA? A pilot study. Clin Orthop Relat Res 2010;468:533–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Mayr E, Nogler M, Benedetti MG, et al. A prospective randomized assessment of earlier functional recovery in THA patients treated by minimally invasive direct anterior approach: a gait analysis study. Clin Biomech (Bristol, Avon) 2009;24:812–818. [DOI] [PubMed] [Google Scholar]
- 57. Lugade V, Wu A, Jewett B, Collis D, Chou LS. Gait asymmetry following an anterior and anterolateral approach to total hip arthroplasty. Clin Biomech (Bristol, Avon) 2010;25:675–680. [DOI] [PubMed] [Google Scholar]
- 58. Lamontagne M, Varin D, Beaulé PE. Does the anterior approach for total hip arthroplasty better restore stair climbing gait mechanics? J Orthop Res 2011;29:1412–1417. [DOI] [PubMed] [Google Scholar]
- 59. Poultsides LA, Triantafyllopoulos GK, Memtsoudis SG, Do HT, Alexiades MM, Sculco TP. Perioperative morbidity of same-day and staged bilateral total hip arthroplasty. J Arthroplasty 2017;32:2974–2979.e1. [DOI] [PubMed] [Google Scholar]
- 60. Tamaki T, Oinuma K, Miura Y, Higashi H, Kaneyama R, Shiratsuchi H. Perioperative complication rate of one-stage bilateral total hip arthroplasty using the direct anterior approach. J Orthop Sci 2016;21:658–661. [DOI] [PubMed] [Google Scholar]
- 61. Watts CD, Houdek MT, Wyles CC, Sierra RJ, Trousdale RT, Taunton MJ. Direct anterior versus posterior simultaneous bilateral total hip arthroplasties: no major differences at 90 days. Am J Orthop 2016;45:E373–E378. [PubMed] [Google Scholar]
- 62. Nakata K, Nishikawa M, Yamamoto K, Hirota S, Yoshikawa H. A clinical comparative study of the direct anterior with mini-posterior approach: two consecutive series. J Arthroplasty 2009;24:698–704. [DOI] [PubMed] [Google Scholar]
- 63. Kobayashi H, Homma Y, Baba T, et al. Surgeons changing the approach for total hip arthroplasty from posterior to direct anterior with fluoroscopy should consider potential excessive cup anteversion and flexion implantation of the stem in their early experience. Int Orthop 2016;40:1813–1819. [DOI] [PubMed] [Google Scholar]
- 64. Lin TJ, Bendich I, Ha AS, Keeney BJ, Moschetti WE, Tomek IM. A comparison of radiographic outcomes after total hip arthroplasty between the posterior approach and direct anterior approach with intraoperative fluoroscopy. J Arthroplasty 2017;32:616–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Benoit B, Gofton W, Beaulé PE. Hueter anterior approach for hip resurfacing: assessment of the learning curve. Orthop Clin North Am 2009;40:357–363. [DOI] [PubMed] [Google Scholar]
- 66. Kreuzer S, Leffers K, Kumar S. Direct anterior approach for hip resurfacing: surgical technique and complications. Clin Orthop Relat Res 2011;469:1574–1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Grob K, Monahan R, Gilbey H, Yap F, Filgueira L, Kuster M. Distal extension of the direct anterior approach to the hip poses risk to neurovascular structures: an anatomical study. J Bone Jt Surg, Am Vol (CD-ROM Ed) 2015;97:126–132. [DOI] [PubMed] [Google Scholar]
- 68. Ghijselings SGM, Driesen R, Simon JP, Corten K. Distal extension of the direct anterior approach to the hip: a cadaveric feasibility study. J Arthroplasty 2017;32:300–303. [DOI] [PubMed] [Google Scholar]
- 69. Nogler MM, Thaler MR. The direct anterior approach for hip revision: accessing the entire femoral diaphysis without endangering the nerve supply. J Arthroplasty 2017;32:510–514. [DOI] [PubMed] [Google Scholar]
- 70. Spanyer JM, Beaumont CM, Yerasimides JG. The extended direct anterior approach for column augmentation in the deficient pelvis: a novel surgical technique, and case series report. J Arthroplasty 2017;32:515–519. [DOI] [PubMed] [Google Scholar]
- 71. Tamaki T, Jonishi K, Miura Y, Oinuma K, Shiratsuchi H. Cementless tapered-wedge stem length affects the risk of periprosthetic femoral fractures in direct anterior total hip arthroplasty. J Arthroplasty 2018;33:805-809. [DOI] [PubMed] [Google Scholar]
- 72. Jewett BA, Collis DK. High complication rate with anterior total hip arthroplasties on a fracture table. Clin Orthop Relat Res 2011;469:503–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Dietrich M, Kabelitz M, Dora C, Zingg PO. Perioperative fractures in cementless total hip arthroplasty using the direct anterior minimally invasive approach: reduced risk with short stems. J Arthroplasty 2018;33:548-554. [DOI] [PubMed] [Google Scholar]
- 74. Hartford JM, Bellino MJ. The learning curve for the direct anterior approach for total hip arthroplasty: a single surgeon’s first 500 cases. Hip Int 2017;27:483–488. [DOI] [PubMed] [Google Scholar]
- 75. Russo MW, Macdonell JR, Paulus MC, Keller JM, Zawadsky MW. Increased complications in obese patients undergoing direct anterior total hip arthroplasty. J Arthroplasty 2015;30:1384–1387. [DOI] [PubMed] [Google Scholar]
- 76. Hallert O, Li Y, Brismar H, Lindgren U. The direct anterior approach: initial experience of a minimally invasive technique for total hip arthroplasty. J Orthop Surg Res 2012;7:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Lanting BA, Odum SM, Cope RP, Patterson AH, Masonis JL. Incidence of perioperative events in single setting bilateral direct anterior approach total hip arthroplasty. J Arthroplasty 2015;30:465–467. [DOI] [PubMed] [Google Scholar]
- 78. Sendtner E, Borowiak K, Schuster T, Woerner M, Grifka J, Renkawitz T. Tackling the learning curve: comparison between the anterior, minimally invasive (Micro-hip®) and the lateral, transgluteal (Bauer) approach for primary total hip replacement. Arch Orthop Trauma Surg 2011;131:597–602. [DOI] [PubMed] [Google Scholar]
- 79. York PJ, Logterman SL, Hak DJ, Mavrogenis A, Mauffrey C. Orthopaedic trauma surgeons and direct anterior total hip arthroplasty: evaluation of learning curve at a level I academic institution. Eur J Orthop Surg Traumatol 2017;27:421–424. [DOI] [PubMed] [Google Scholar]
- 80. Melman WPR, Mollen BP, Kollen BJ, Verheyen CCPM. First experiences with the direct anterior approach in lateral decubitus position: learning curve and 1 year complication rate. Hip Int 2015;25:251–257. [DOI] [PubMed] [Google Scholar]
- 81. de Steiger RN, Lorimer M, Solomon M. What is the learning curve for the anterior approach for total hip arthroplasty? Clin Orthop Relat Res 2015;473:3860–3866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Homma Y, Baba T, Kobayashi H, et al. Safety in early experience with a direct anterior approach using fluoroscopic guidance with manual leg control for primary total hip arthroplasty: a consecutive one hundred and twenty case series. Int Orthop 2016;40:2487–2494. [DOI] [PubMed] [Google Scholar]
- 83. Eto S, Hwang K, Huddleston JI, Amanatullah DF, Maloney WJ, Goodman SB. The direct anterior approach is associated with early revision total hip arthroplasty. J Arthroplasty 2017;32:1001–1005. [DOI] [PubMed] [Google Scholar]
- 84. Brun O-CL, Månsson L, Nordsletten L. The direct anterior minimal invasive approach in total hip replacement: a prospective departmental study on the learning curve. Hip Int 2018;28:156-160. [DOI] [PubMed] [Google Scholar]
- 85. Mayr E, Krismer M, Ertl M, Kessler O, Thaler M, Nogler M. Uncompromised quality of the cement mantle in Exeter femoral components implanted through a minimally-invasive direct anterior approach. A prospective, randomised cadaver study. J Bone Joint Surg Br 2006;88:1252–1256. [DOI] [PubMed] [Google Scholar]
- 86. Watts CD, Houdek MT, Wagner ER, Sculco PK, Chalmers BP, Taunton MJ. High risk of wound complications following direct anterior total hip arthroplasty in obese patients. J Arthroplasty 2015;30:2296–2298. [DOI] [PubMed] [Google Scholar]
- 87. Purcell RL, Parks NL, Cody JP, Hamilton WG. Comparison of wound complications and deep infections with direct anterior and posterior approaches in obese hip arthroplasty patients. J Arthroplasty 2018;33:220–223. [DOI] [PubMed] [Google Scholar]
- 88. Shofoluwe AI, Naveen NB, Inabathula A, et al. Internet promotion of direct anterior approach total hip arthroplasty by members of the American association of hip and knee surgeons. J Arthroplasty 2018;33:167–170.e1. [DOI] [PubMed] [Google Scholar]