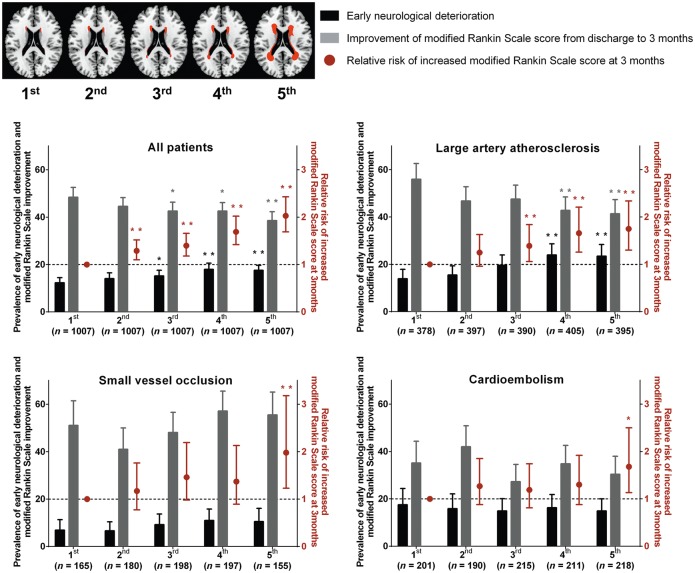
Figure 1.
Graphical summary of the major results of this study. Predicted prevalence of early neurological deterioration/post-discharge improvement of modified Rankin Scale score and relative risk of increased modified Rankin Scale score at 3 months: the impact of WMH volume, generally and by stroke subtype. Top left: Topographical frequency-volume maps that were generated by using the quantitative magnetic resonance data of the 5035 patients of this study, as previously reported in our study (n = 2699 patients with first-ever acute ischaemic stroke) using the Kim statistical WMH scoring system: a graphical reference system allowing the quantitative estimation of the severity of WMHs as a percentile rank score (Ryu et al., 2014). First to fifth (WMH volume quintile) images correspond to 10, 30, 50, 70 and 90 percentile maps, respectively. Predicted prevalence of early neurological deterioration and improvement of modified Rankin Scale score (from discharge to 3 months) were derived from multiple logistic regression analysis with adjustment for age, NIHSS score, sex, body mass index, hypertension, diabetes, hyperlipidemia, smoking, coronary artery disease, atrial fibrillation, prior use of statin, haemoglobin, total cholesterol, fasting glucose, and log-transformed infarct volume on diffusion-weighted image. Black or grey bars represent predicted prevalence with 95% CI (left y-axis). Red dots and lines indicate adjusted ORs with 95% CI for the relative risk of increased modified Rankin Scale score at 3 months by ordinal logistic regression analysis. *P < 0.05 and **P < 0.01 compared with the first quintile of WMHs.