Fig. 6.
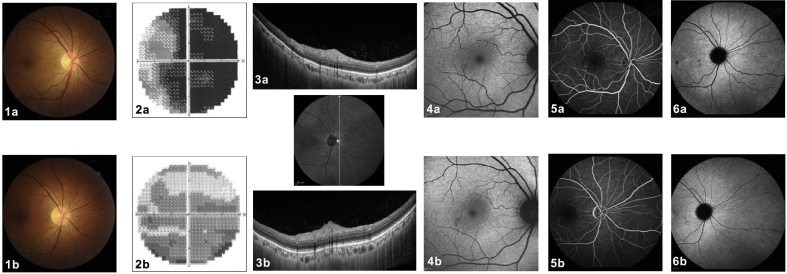
Photoreceptoritis. A 46-year-old man presented with sudden and profound visual loss in his right eye. Upon ocular examination, the best corrected visual acuity (BCVA) was hand motion in the right eye and 20/20 in the left eye. Anterior segment biomicroscopy and intraocular pressure were normal in both eyes. (1a) Color fundus photographs of the right eye revealed no abnormalities. (2a) The visual field of the right eye revealed global and severe sensitivity depression (mean defect −25.75 dB). (3a) Cross-sectional optical coherence tomography (OCT) through the nasal periphery demonstrated an absence of the hyperreflective ellipsoid zone. (4a) Fundus autofluorescence (FAF) showed no significant alterations. (5a) The retinal vasculature was normal on fluorescein angiography (FA) and (6a) no perfusion anomaly (no hypofluorescent areas) was seen on indocyanine green angiography (ICGA). Five months later, BCVA improved to 1/20 in the right eye. (1b) Fundus color photography was unchanged. (2b) The visual fields improved (mean defect −11.96 dB) and (3b) cross-sectional follow-up OCT, scanned in the same location, demonstrated the reappearance of a still disrupted hyperreflective ellipsoid zone, explaining the better visual field performance. (4b) FAF, (5b) FA, and (6b) ICGA did not present relevant abnormalities. This case represents a primary photoreceptoritis with no other clinical signs and no sign of a choriocapillaris perfusion anomaly.