Figure 1.
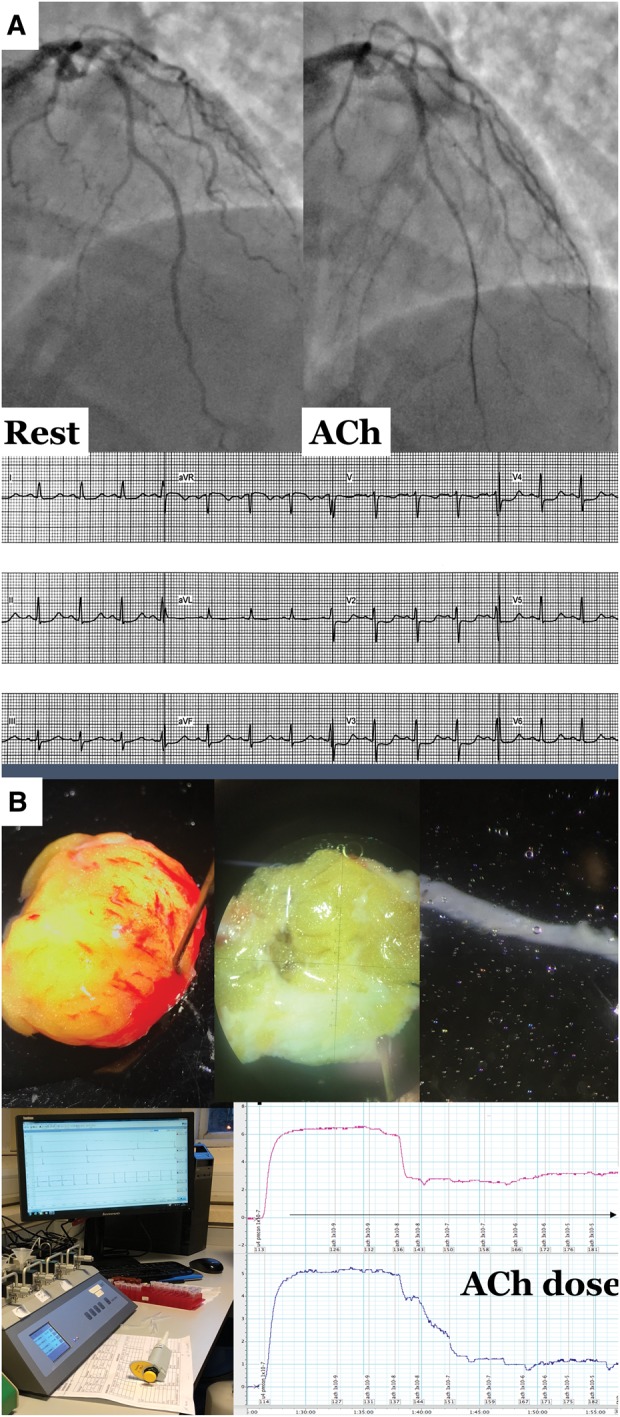
(A) Illustrative case of microvascular angina. (B) Gluteal biopsy procedure, dissection of resistance artery, and myography workstation. (A) A 43-year-old female smoker with family history of early cardiovascular disease was referred for invasive angiography with 12 months of typical angina and positive stress ECG. Recruited into British Heart Foundation CorMicA study with findings of non-obstructive atheroma in the left anterior descending coronary artery. Pressure wire assessment confirmed profoundly reduced coronary flow reserve (1.3) but non-obstructive physiology (fractional flow reserve 0.86) and normal index of microvascular resistance with adenosine (index of microcirculatory resistance 18). Acetylcholine testing confirmed microvascular spasm to acetylcholine (reproduction of typical angina, ST segment deviation and <90% epicardial vasoconstriction to acetylcholine. (B) Surgical gluteal skin fat biopsy with dissection of resistance artery under light microscopy. Peripheral resistance arteries were harvested and set-up for our wire myography protocol. The myography tracing shows a cumulative concentration-response curve to dilator agonist acetylcholine. We averaged the relaxation at each concentration compared to baseline confirming reduced maximal relaxation to this probe of endothelial function. Overall this lady was diagnosed with microvascular angina (typical angina, proven coronary microvascular dysfunction) with evidence of widespread peripheral endothelial dysfunction.
