Abstract
Unconjugated bilirubin is considered a potent antioxidant when present at moderate levels. However, at high concentrations, it produces severe neurological damage and death associated with kernicterus due to oxidative stress and other mechanisms. While it is widely recognized that oxidative stress by different toxic insults results in severe damage to cellular macromolecules, especially to DNA, no data are available either on DNA damage in the brain triggered by hyperbilirubinemia during the neonatal period or on the activation of DNA repair mechanisms. Here, using a mouse model of neonatal hyperbilirubinemia, we demonstrated that DNA damage occurs in vivo in the cerebellum, the brain region most affected by bilirubin toxicity. We studied the mechanisms associated with potential toxic action of bilirubin on DNA in in vitro models, which showed significant increases in DNA damage when neuronal and nonneuronal cells were treated with 140 nM of free bilirubin (Bf), as determined by γH2AX Western blot and immunofluorescence analyses. Cotreatment of cells with N-acetyl-cysteine, a potent oxidative-stress inhibitor, prevented DNA damage by bilirubin, supporting the concept that DNA damage was caused by bilirubin-induced oxidative stress. Bilirubin treatment also activated the main DNA repair pathways through homologous recombination (HR) and nonhomologous end joining (NHEJ), which may be adaptive responses to repair bilirubin-induced DNA damage. Since DNA damage may be another important factor contributing to neuronal death and bilirubin encephalopathy, these results contribute to the understanding of the mechanisms associated with bilirubin toxicity and may be of relevance in neonates affected with severe hyperbilirubinemia.
1. Introduction
Neonatal jaundice is a frequent condition resulting mainly from the temporary delay in the activation of bilirubin conjugation in the liver [1] or from genetic mutations in the UGT1A1 gene, with the permanent loss of bilirubin conjugation activity, a condition such as the Crigler-Najjar syndromes [2]. Prolonged and severe hyperbilirubinemia may be toxic for the developing nervous system, resulting in serious neurological damage and death associated with kernicterus [3].
During bilirubin-induced neurotoxicity, different molecular pathways are activated, ranging from mitochondrial damage and oxidative stress to endoplasmic reticulum (ER) stress response and inflammation [4]. Several in vitro and in vivo data demonstrated a main role of oxidative stress in cytotoxicity, when high, toxic, bilirubin concentrations are present. In fact, incubation of synaptic vesicles, tissue culture cells, and primary cell cultures of neurons, oligodendrocytes, and astrocytes with bilirubin resulted in increases in oxidative stress and cytotoxicity [4–12]. In vivo studies in Gunn rats show high levels of lipid peroxidation by sulphadimethoxine-induced hyperbilirubinemia [13]. Studies in hyperbilirubinemic Ugt1−/− mice showed an impairment of antioxidant defenses with the activation of key oxidative stress markers [14–16].
It is widely recognized that increases in oxidative stress by a number of different insults result in severe damage to cellular macromolecules, especially to DNA [17, 18]. However, few data are available on the effects of bilirubin in DNA damage and its repair mechanisms.
Studies of DNA damage in peripheral lymphocytes of hyperbilirubinemic newborns do not provide conclusive evidence [19–24], while during postmortem analyses of cases affected by bilirubin encephalopathy, 8-hydroxy-2′-deoxyguanosine (8-OHG) was present only in half of the cases [25]. More recent data show increased DNA strand breaks and apurinic sites in peripheral blood mononuclear cells (PBMCs) of Gunn rats (a nonlethal model of neonatal hyperbilirubinemia), compared to wild-type (WT) Wistar controls [26], and the increases in 8-OHG and γH2AX concentrations after treating tissue culture cells with bilirubin [12].
Still, no information is available regarding the effects of bilirubin on DNA damage in vivo, during neonatal development, the most critical period of neuronal susceptibility to bilirubin toxicity during postnatal brain development, and in vitro on DNA damage and DNA repair mechanisms in tissue culture cells treated with bilirubin.
In the present work, we studied the generation of DNA damage by bilirubin in vivo, using a very severe lethal mouse model of neonatal hyperbilirubinemia closely reproducing the human condition [27]. We also investigated the induction of DNA damage by bilirubin in neuronal and nonneuronal cells and the activation of the main DNA repair pathways: homologous recombination (HR) and nonhomologous end joining (NHEJ).
2. Materials and Methods
2.1. Animals
Mice were housed and handled according to institutional guidelines. Ethical and experimental procedures were reviewed and approved by the ICGEB board, with full respect to the EU Directive 2010/63/EU for animal experimentation. Ugt1−/− mice with a FVB/NJ background were generated as previously described [27, 28]. Homozygous mutant animals were obtained from heterozygous Ugt1+/− matings. Ugt1+/+ (WT) littermates were used as controls. Animals used in this study were at least 99.8% FVB/NJ genetic background, obtained after more than ten backcrosses with WT FVB/NJ mice. Mice were kept in a temperature-controlled environment with a 12/12 h light/dark cycle. They received a standard chow diet and water ad libitum.
2.2. Biochemical Analysis of Plasma Samples
Total bilirubin (TB) determinations in plasma were performed as previously described [27] and in the same animals that were used in Figure 1 by Western blot (WB).
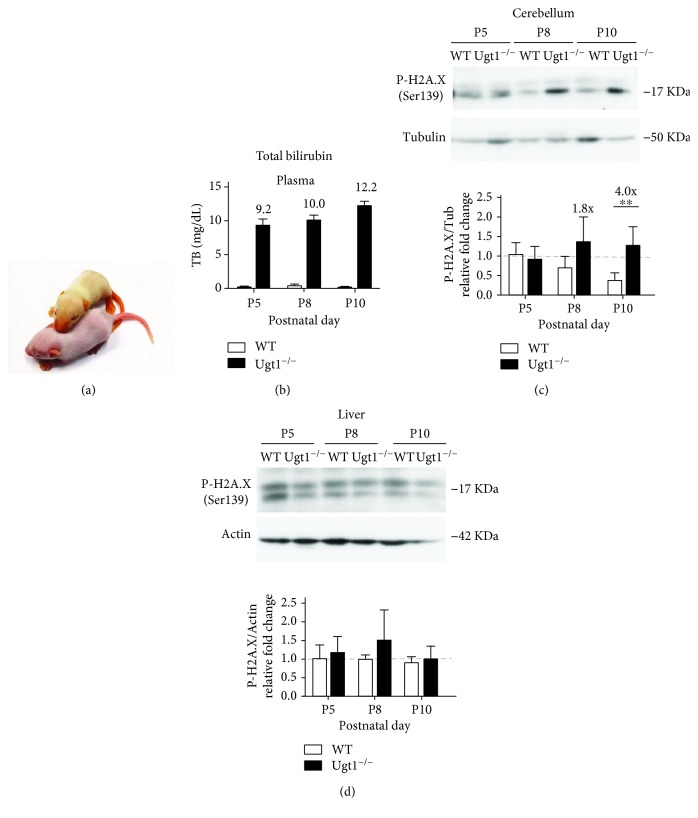
Figure 1.
In vivo analysis of DNA damage in hyperbilirubinemic mice. Hyperbilirubinemic Ugt1−/− mice (a) were used to determine the levels of plasma bilirubin (b) and γH2AX (c and d) at different time points (P5, P8, and P10). Western blot analyses of the cerebella and liver of wild-type (WT) and mutant mice were performed using a γH2AX-specific antibody. The γH2AX signal was quantified and normalized (β-tubulin for the cerebellum, and actin for the liver). The values above the bars (c; P8 and P10) indicate the fold increase of the signal present in mutant tissues with respect to age-matched WT tissues. Five animals were analyzed per each genotype and time point. Two-way ANOVA; ∗∗ P < 0.01.
2.3. Preparation of Total Protein Extracts and Western Blot from Tissues
The selected organs were analyzed as previously described [28]. Briefly, cerebella and livers harvested at postnatal day (P) 5, P8, and P10 were dissected and homogenized in lysis buffer (150 mM NaCl, 1% NP-40, 0.5% DOC, 0.1% SDS, 50 mM Tris HCl pH 8, 2× protease inhibitors, 1× phosphatase inhibitors) and analyzed by WB. Primary anti-γH2AX (Ser 139) antibody (Millipore, Milan, Italy) was diluted 1 : 2000 in 5% milk Tris HCl-buffer saline-Tween (TBST); anti-PARP antibody (#9542, Cell Signaling) was diluted 1 : 5000 in 5% milk TBST. Anti-tubulin mAb E7 (Developmental Studies Hybridoma Bank, Iowa City, IA) or anti-actin (Sigma-Aldrich) antibodies were used as loading controls.
2.4. Cell Culture
SH-SY5Y cells were cultured in Eagle's minimum essential medium F12 (EMEM/F12, Sigma-Aldrich) supplemented with 15% fetal calf serum (FCS), 1% antibiotic + antimycotic solution (Sigma-Aldrich A5955), 1% MEM nonessential amino acid solution (Sigma-Aldrich M7145). HeLa DR-GFP and HeLa cells were cultured in Dulbecco's modified Eagle's medium (DMEM, Thermo Fisher Scientific, Gibco) supplemented with 10% FCS and 1% antibiotic + antimycotic solution (Sigma-Aldrich A5955). The HeLa DR-GFP cell line was generously provided by Dr. Enrico Avvedimento [29].
2.5. Unconjugated Bilirubin (UCB) Treatment
UCB was purified using the method of Ostrow et al. [30], divided in aliquots and stored at −20°C until use. The total UCB concentration needed to reach the concentration of free bilirubin (Bf) 70 and 140 nM was determined using a previously described protocol [31]. UCB needed to reach the desired concentrations of Bf dissolved in 0.6% DMSO, and appropriate amounts of UCB were added to culture media in order to reach the desired Bf and measured spectrophotometrically at 468 nm.
2.6. MTT Assay for Cellular Viability
The MTT test for cellular viability was performed as previously described [32]. For a detailed description, see Supplementary Materials (available here).
2.7. Cell Transfection
For a detailed description, see Supplementary Materials.
2.8. SDS PAGE and WB Analysis
For a detailed description, see Supplementary Materials.
2.9. Immunofluorescence (IF) Analysis
For a detailed description, see Supplementary Materials.
2.10. Statistical Analyses
The Graphpad Prism package was used to analyze the data. All data were represented as mean ± SD. P < 0.05 was considered significant. Depending on the experimental design, Student's t-test, one-way ANOVA, or two-way ANOVA with Bonferroni's post hoc comparison tests was used, as indicated in the legends to the figures.
3. Results
3.1. Neonate Mice with Severe Hyperbilirubinemia Have DNA Damage in the Cerebellum
We have previously demonstrated key roles of oxidative stress and inflammation in bilirubin neurotoxicity in the cerebellum of hyperbilirubinemic Ugt1−/− neonatal mice [15, 16]. In the present study, we investigated whether bilirubin-induced oxidative stress is associated with increased DNA damage in vivo in hyperbilirubinemic Ugt1−/− neonatal mice (Figure 1(a)). In these animals, plasma bilirubin levels increased during the first days of life due to the absence of glucuronidation activity (Figure 1(b)), reaching toxic levels that result in the death of all pups before P15 (with 50% mortality at P11) [16, 27]. Since the cerebellum is the most affected region of the brain in this mouse strain, with no other organs damaged [27, 28, 33], we determined the levels of the phosphorylated histone H2AX (γH2AX) in the cerebellum of mutant pups at different time points. γH2AX is a well-recognized, highly specific, and sensitive molecular marker for monitoring DNA damage [34]. In addition, we also analyzed liver samples of the same animals to verify whether other organs were affected by bilirubin-induced DNA damage. WB of cerebellar γH2AX showed a time-dependent increase in the levels of γH2AX in the cerebellum of Ugt1−/− mice versus age-matched normobilirubinemic WT littermates, with significant differences at P8 and P10 (Figure 1(c)), time points that are critical for neuro-susceptibility to bilirubin toxicity [27]. On the contrary, no obvious differences were observed in the liver (Figure 1(d)). These results demonstrated that bilirubin-induced DNA damage occurred during severe neonatal hyperbilirubinemia, suggesting that DNA damage may be associated with bilirubin neurotoxicity in vivo.
3.2. Bilirubin-Induced DNA Damage In Vitro
After having demonstrated the presence of DNA damage in vivo in the cerebellum of hyperbilirubinemic Ugt1−/− mice, we used a simpler experimental setup using in vitro cell cultures to study the associated mechanisms.
We first confirmed the toxicity of bilirubin to neuronal SH-SY5Y human cells by incubating the cells with the quantified Bf concentrations in the presence of FCS. Bilirubin concentration was adjusted to reach 70 or 140 nM of Bf using the modified peroxidase assay [31] as described in Materials and Methods. Cell viability decreased after 4 h treatment with both 70 and 140 nM Bf concentrations and further decreased at 24 h, reaching 60% with 140 nM Bf (Supplementary Figure 1). Based on these findings and previous results [12, 32, 35–37], the 140 nM Bf concentration was selected for the next set of experiments.
To determine the toxic effects of high levels of bilirubin on DNA, cells were incubated with 140 nM Bf for different times (up to 48 h) and the levels of γH2AX determined by WB analysis. Incubation of SH-SY5Y cells with bilirubin resulted in a significant increase in the γH2AX signal, reaching a maximum at 48 h (Figures 2(a) and 2(b)), confirming the presence of bilirubin-induced DNA damage as observed in vivo (Figure 1). Untreated (UT) and DMSO-treated (vehicle) cells showed similar γH2AX levels, thereby ruling out any effect due to DMSO.
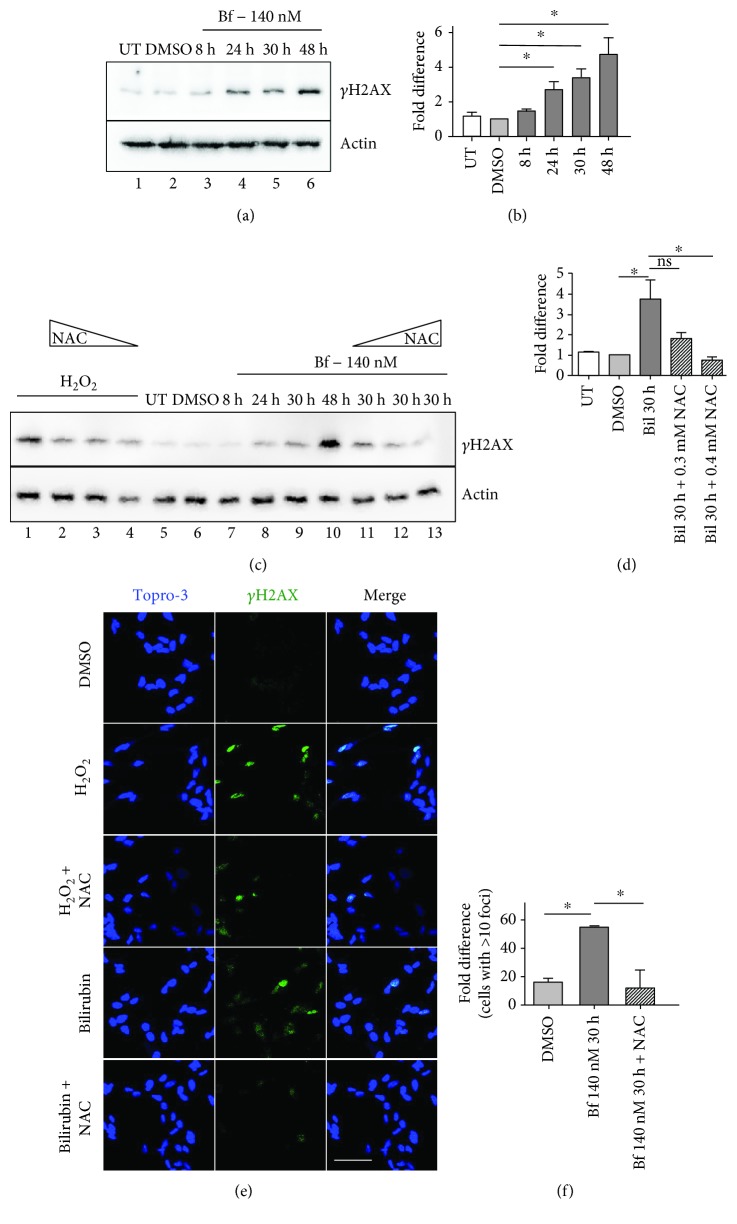
Figure 2.
Bilirubin-induced oxidative stress causes DNA damage in SH-SY5Y cells. SH-SY5Y cells were treated with 140 nM free bilirubin (Bf) for different time points (8, 24, 30, and 48 h; lanes 3-6). DMSO (0.6% DMSO, bilirubin solvent) served as controls (lane 2). Cells were collected at the indicated time points, and the levels of γH2AX were determined by Western blot analysis and quantified (mean of three independent experiments (b)); (c, d) SH-SY5Y cells were treated with H2O2 (lanes 1-4) or 140 nM Bf for different times, as indicated (lanes 7-13). In lanes 2-4 and 11-13, cells were treated with H2O2 or 140 nM Bf for 48 h plus N-acetyl-cysteine (NAC) treatment (0.1, 0.3, or 0.4 mM). γH2AX was determined by Western blot, quantified and normalized (actin). (d) Quantification of two independent experiments; (e, f) SH-SY5Y cells were treated with H2O2 or 140 nM bilirubin for 30 h, with or without NAC (0.4 mM) treatment, as described in Materials and Methods. γH2AX foci were determined by immunofluorescence. Cells containing more than 10 foci were considered positive. The scale bar corresponds to 30 μM; (f) quantification from two independent experiments. Values represented as mean ± SD. One-way ANOVA with Bonferroni's post hoc test was applied for statistical analysis. ∗ P < 0.05; NS: not significative; UT: untreated cells.
Next, to determine whether the observed increase in γH2Ax was the consequence of bilirubin-induced oxidative stress, cells were incubated with bilirubin in the presence or absence of N-acetyl cysteine (NAC), a powerful exogenous antioxidant. Incubation of cells with H2O2, a potent generator of reactive oxygen species (ROS), was used as a positive control. In fact, the levels of γH2AX induced by H2O2 decreased after NAC treatment (Figure 2(c), lanes 2-4). As observed in lanes 11-13 (Figures 2(c) and 2(d)), NAC treatment inhibited DNA damage in a dose-dependent manner.
We further confirmed these results by immunofluorescence (IF) analysis of treated cells (Figures 2(e) and 2(f)). Treatment of SH-SY5Y cells with bilirubin resulted in ~50% of cells having γH2AX foci, proportion that was reduced to control levels with NAC treatment.
These results indicate that bilirubin-induced oxidative stress appears to be the main mechanism causing DNA damage in vitro.
To gain a deeper insight in the associated mechanisms, we determined poly(ADP-ribose) polymerase (PARP) levels in the cerebella of mutant mice at P10. PARP has an important role in DNA repair, and at the same time, it modulates inflammation by activating nuclear factor κB (NFκB) [38]. We observed an increase in the cleaved form of PARP at P10 (Supplementary Figure 2), concomitantly with the maximum increase in inflammatory response reported for this animal model [16]. These data suggest that bilirubin-induced DNA damage response and inflammation may be associated in vivo.
3.3. Bilirubin Stimulates Nonhomologous End Joining (NHEJ) and Homologous Recombination (HR) DNA Repair Pathways In Vitro
We then investigated the mechanisms of DNA double-strand break (DSB) repair in the presence of toxic levels of Bf. To determine the effect of bilirubin in NHEJ and HR DNA repair pathways, we used HeLa cells and the HeLa DR-GFP cell lines [29]. We first determined HeLa DR-GFP cell viability after a bilirubin toxic insult at different time points by exposing cells to 140 nM Bf (Supplementary Figure 3). As expected, the viability of cells decreased in a time-dependent manner, reaching 45% after 24 h.
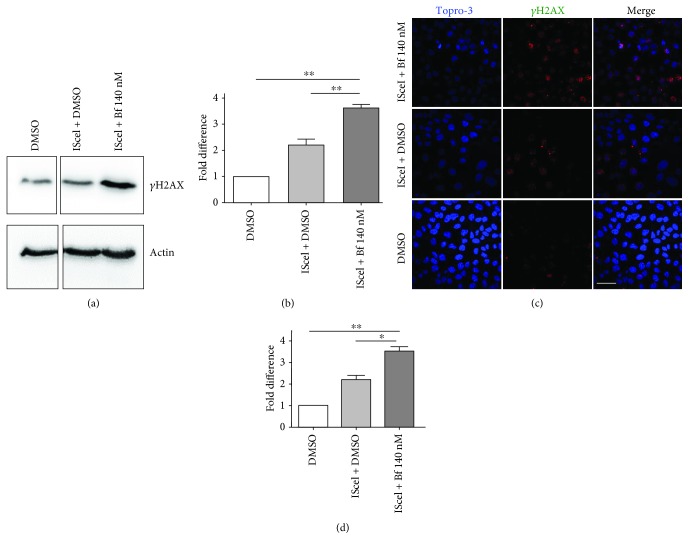
To study the HR-mediated DNA repair mechanism in vitro, we used the HeLa DR-GFP cell line [29]. We determined the levels of γH2AX by WB and IF in these cells upon bilirubin and ISceI treatment combinations. We observed that transfection with the ISceI-encoding plasmid increased γH2AX signaling, as determined both by WB and IF. γH2AX levels were further increased in ISceI-transfected cells treated with 140 nM Bf (Figure 3). These results indicated that the amount of DSB is increased by bilirubin treatment.
Figure 3.
Bilirubin-induced DNA damage in HeLa DR-GFP cells. (a, b) Western blot analysis of HeLa DR-GFP cells transfected with a plasmid encoding the ISceI endonuclease (pCBA IsceI) and treated with DMSO (control) or 140 nM free bilirubin (Bf). γH2AX levels were determined by Western blot analysis, quantified and normalized (actin). (b) Quantification from three independent experiments. (c, d) HeLa DR-GFP cells were treated as described in (a) and (b), and γH2AX foci were determined by immunofluorescence. Cells containing more than 10 foci were considered positive. (f) Quantification from two independent experiments. One-way ANOVA with Bonferroni's post hoc test was used to perform statistical analysis. ∗ P < 0.05; ∗∗ P < 0.01.
The HeLa DR-GFP HR reporter cell line contains a single genomic integration of the DR-GFP recombination reporter construct [29], which has two differentially inactivated versions of a tandemly repeated (DR) GFP, developed by Pierce et al. [39]. The upstream GFP gene (Cassette I), under the transcriptional control of the CMV enhancer and chicken β-actin promoter, is interrupted by an ISceI restriction enzyme site, a rare-cutting endonuclease [40]. Introduction of the ISceI site leads to the formation of in-frame stop codons inactivating Cassette I. The downstream GFP fragment (Cassette II) is truncated at the 5′ and 3′ ends, resulting in a truncated and inactive GFP product (Figure 4(a)). Transient transfection with a plasmid encoding the ISceI endonuclease generates a DSB, which enhances HR between the two cassettes and thereby production of active GFP that can be quantified by flow cytometry (Figure 4(a)) [29].
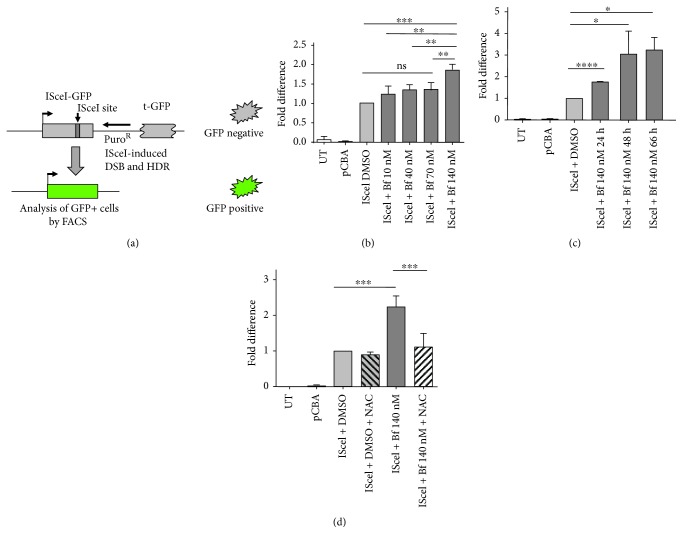
Figure 4.
Bilirubin-induced oxidative stress modulates homologous recombination. (a) Schematic diagram of the DR-GFP system. (b) HeLa DR-GFP cells were transfected with a plasmid encoding the IsceI endonuclease (pCBA IsceI) and treated with different amounts of Bf (from 10 to 140 nM). Cells were analyzed for GFP fluorescence by FACS analysis 72 h posttransfection. Data were normalized for transfection efficiency using renilla luciferase activity, encoded by a cotransfected plasmid. (c) HeLa DR-GFP cells were transfected with the ISceI plasmid and treated for different times with 140 nM Bf. Data was normalized for transfection efficiency by transfecting cells with eGFP in parallel wells. (d) HeLa DR-GFP cells were cotransfected with a plasmid encoding IsceI (pCBA IsceI) and plasmid encoding renilla luciferase (pHRG-TK renilla). 6-7 h after transfection, 140 nM Bf was added to cells, with or without N-acetyl cysteine (NAC) treatment, as described in Materials and Methods. Data were normalized for transfection efficiency using renilla activity in the same well. Values were represented as mean ± SD. One-way ANOVA with Bonferroni's post hoc test was used to perform statistical analysis. ∗ P < 0.05; ∗∗ P < 0.01; ∗∗∗ P < 0.001; ∗∗∗∗ P < 0.0001.
We then determined the modulation of HR-mediated DNA repair by bilirubin-induced oxidative stress using the HeLa DR-GFP cell line (Figure 4(a)) [29]. Transfection of DR-GFP cells with the IsceI-encoding plasmid resulted in a significant increase in GFP-positive cells compared to the pCBA control plasmid (Figure 4(b) and Supplementary Figure 4). Incubation of the ISceI-transfected cells with increasing amounts of Bf resulted in a dose-dependent increase of HR, reaching a statistically significant difference at 140 nM Bf. Similarly, we also observed a time-dependent increase in HR in cells treated with ISceI plus bilirubin, reaching a plateau at 66 h (Figure 4(c) and Supplementary Figure 4). To determine whether the increase in HR by bilirubin was associated with oxidative stress, ISceI-transfected cells were treated with bilirubin and NAC. We observed that NAC treatment reduced HR to the levels of the IsceI control (without bilirubin treatment) (Figure 4(d) and Supplementary Figure 4) suggesting that the increase in HR was associated with the bilirubin-induced increase in oxidative stress.
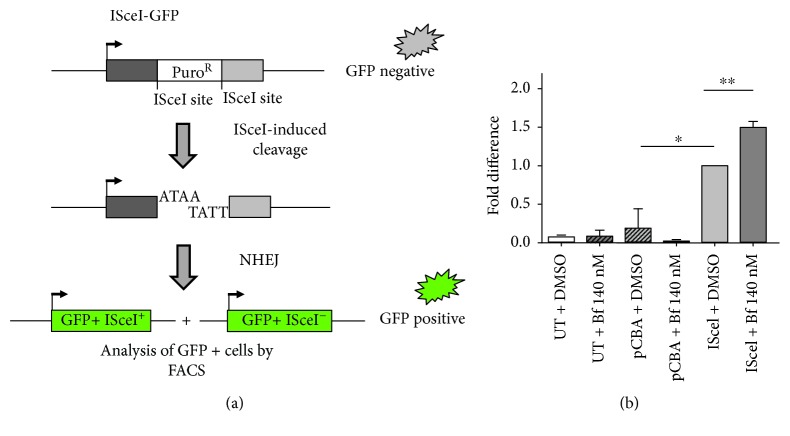
Next, to determine the potential increase in NHEJ, we used a reporter vector specifically designed to detect multiple classes of NHEJ events [41]. The EJ5-GFP vector contains a promoter that is separated from a GFP-coding cassette by a puromycin-resistance gene. This gene is flanked by two ISceI sites which is a rare-cutting endonuclease [40]. Upon digestion with ISceI provided by a second plasmid, the puromycin cassette is removed and the two ISceI-induced DSBs are joined by NHEJ. This results in the restoration of the GFP gene transcription by the promoter, now joined to the GFP expression cassette. GFP-positive cells were quantified by FACS analysis (Figure 5(a) and Supplementary Figure 5).
Figure 5.
Bilirubin-induced NHEJ in HeLa cells. (a) Schematic representation of pIM EJ5 GFP reporter plasmid used for nonhomologous end joining (NHEJ) experiments. (b) HeLa cells were cotransfected with pIM EJ5 GFP plasmid encoding the NHEJ reporter and a plasmid encoding renilla luciferase (pHRG-TK renilla). Bilirubin (140 nM Bf) or DMSO (control) was added to cells 6-7 h after transfection. Cells were analyzed for GFP fluorescence 72 h posttransfection by fluorescence-activated cell sorting (FACS) analysis. The graph represents the quantification of two independent experiments. Data were normalized for transfection efficiency using renilla luciferase activity. One-way ANOVA with Bonferroni's post hoc test was used to perform statistical analysis. Values are represented as mean ± SD. ∗ P < 0.05; ∗∗ P < 0.01.
Hela cells were transfected with the EJ5-GFP reporter plasmid, with or without the ISceI-coding plasmid (or pCBA control plasmid), and treated with 140 nM Bf or DMSO (vehicle). A plasmid encoding renilla luciferase (pHRG-TK renilla) was used to normalize for differences in transfection efficiency. Incubation with ISceI plus DMSO resulted in a significant increase in GFP-positive cells. The proportion of GFP-positive cells further increased after the incubation of the cells with 140 nM Bf, strongly suggesting the modulation of NHEJ by bilirubin.
4. Discussion
Bilirubin is considered a physiologically important antioxidant [42], with beneficial effects at mildly elevated concentrations, and can neutralize ROS and prevent oxidative damage [43–53]. However, at higher concentrations, bilirubin is toxic to the developing brain, leading to bilirubin encephalopathy or, in the most severe cases, to irreversible neurological damage and death due to kernicterus [3, 54]. Several in vitro and in vivo studies, including ours, have shown that oxidative stress generated by elevated concentrations of bilirubin is a key mechanism of bilirubin-induced cell toxicity [5, 8–15, 32].
In the present study, we have shown the effects of toxic concentrations of bilirubin to induce DNA damage and modulate DNA repair mechanisms. We first studied the levels of the sensitive DNA damage marker γH2AX [34] in the cerebella of Ugt1−/− mice versus age-matched normobilirubinemic littermates, revealing the presence of DNA damage in vivo. Notably, since these animals reproduce the major features of the Crigler-Najjar syndrome type I, such as the absence of bilirubin glucuronidation activity, severe neonatal hyperbilirubinemia, bilirubin neurotoxicity with cerebellar abnormalities, and death soon after birth if untreated [27, 28], these results may be clinically relevant.
DNA lesions may result in chromosomal translocation, deletions, and cell cycle arrest by stalling of replication forks [55]. Accordingly, alterations in cell proliferation by bilirubin have already been proposed [56–59] and have been documented in both tissue culture cells exposed to bilirubin [12] and the cerebellum of Gunn rats [60]. Likewise, the apoptosis-mediated neuronal death observed in the cerebellum of Ugt1−/− pups [15, 16, 27] could be associated to some extent with the increased oxidative stress-induced DNA lesions in these animals.
DNA damage by bilirubin in Crigler-Najjar patients has never been directly addressed. Studies in babies with neonatal hyperbilirubinemia demonstrated DNA damage effects on peripheral blood after intensive phototherapy treatment. However, these studies showed controversial results regarding the presence of DNA damage in untreated (or prephototherapy) jaundiced babies compared to control normal groups [19–22, 24] and were performed in peripheral cells, which may have different susceptibility to bilirubin-induced oxidative stress than bilirubin-target organs. In fact, we have shown a time-dependent increase in DNA damage in the cerebellum, which is the most affected organ in the Ugt1−/− hyperbilirubinemic model [27], while no DNA damage occurred in an unaffected tissue such the liver, which presents a higher total tissue bilirubin concentration compared to the cerebellum [61]. This observation is very intriguing as previous studies suggested the induction of oxidative stress in liver cell lines after bilirubin treatment [9, 37], an effect not observed in vivo. These discrepancies may be related to differences between in vitro and in vivo conditions, to the higher susceptibility of the developing cerebellum to oxidative stress (compared to the liver), and to differences in the levels of antioxidant enzymes in the liver vs. cerebellum [62].
Importantly, when we investigated the effects of bilirubin in vitro by incubating neuronal and nonneuronal cells with concentrations of bilirubin normally found in jaundiced patients, we not only reported the induction of DNA damage as determined by γH2AX analysis but also demonstrated that it is caused by the prooxidant toxic action of the pigment. In fact, treatment with NAC, a potent antioxidant, prevented bilirubin-induced DNA damage and also DNA damage generated by H2O2, a widely recognized ROS generator and DNA damage inducer. These results strongly support the idea that bilirubin-induced oxidative stress is an important determinant of neurotoxicity [7, 37] and that DNA damage is caused by the increase in ROS upon bilirubin exposure. We have also reported the activation of PARP, suggesting a close connection between inflammation and DNA damage by bilirubin-induced toxicity. Interestingly, PARP modulates inflammation through the activation of NFκB [38], a transcription factor upregulated in this animal model [16] and in neuronal cell cultures exposed to toxic levels of bilirubin [36]. However, further studies will be necessary to provide deeper mechanistic insights.
Our data are in line with our previous published results, showing the increase in ROS levels after incubation of cells with bilirubin [11, 12]. Cells treated with bilirubin showed an increase in intracellular ROS associated with decreased survival [11]. SH-SY5Y cells treated with bilirubin differentially expressed proteins involved in oxidative stress response such as PARK7/DJ-1, a multifunctional neuroprotective protein, a key protective factor in UCB-induced cell damage [12]. Bilirubin treatment also resulted in the reduction of cell proliferation and increase of DNA damage, as observed by increases in 8-OHG and γH2AX content [12]. Studies in hyperbilirubinemic Ugt1−/− mice showed an increase in heme oxygenase-I (HO-1) levels in activated microglia cells in the cerebella at P8 and P10. However, other genes involved in oxidative stress response were unaffected [16], suggesting that the presence of a partial in vivo response to this severe insult is unable to prevent or revert the damage. When the cerebellar proteome of P4 Ugt1−/− newborn mice bearing the more severe C57Bl/6 genetic background was analyzed, we observed the impairment of oxidative stress defenses and an increase in cell death in the cerebella of these mice [15].
The findings presented here raise important concerns on the potential risks of carcinogenesis and mutagenic consequences of bilirubin, when present at very high plasma concentrations. Although no significant DNA damage is found in Gilbert patients and Gunn rats [26], no information is available from patients having permanently higher levels of UCB such as Crigler-Najjar syndrome (CNS) type I and II patients. In addition, depending on the country heath system, these patients may undergo liver transplantation early in childhood, limiting the possibility to obtain information related to tumor development in high bilirubin conditions in the long term. The potential risks of carcinogenesis are also limited by other confounding factors present after liver transplantation, such as life-long immunosuppression to avoid organ rejection, a treatment that increases the risk of developing tumors [63, 64]. Thus, these results may be important for CNS patients that do not undergo liver transplantation early in age. Because phototherapy treatment is less efficacious after growth and pubertal development, adult CNS patients may have very high levels of plasma bilirubin with sporadic spikes of even higher levels of plasma bilirubin [65], putting them at risk of DNA damage. In fact, the accumulation of DNA lesions in other scenarios contributes to neuronal cell death [66], a phenomenon observed in specific regions of the brain both in hyperbilirubinemic patients and rodent animal models [15, 27, 67, 68].
The data presented in this work show that bilirubin increases DNA repair capacity as a result of the oxidative stress-induced DNA damage. Cells activate DNA damage response pathways to correct the genetic lesions. For DSB repair, two main mechanisms are active: NHEJ [69] and HR [70]. We evaluated HR and NHEJ DNA repair mechanisms using specific reporter systems [29, 39–41]. Both DNA repair mechanisms were stimulated by the bilirubin treatment, as demonstrated by a significantly increased frequency of GFP-positive cells after their incubation with bilirubin. The effect was also consequent to bilirubin-induced oxidative stress since NAC treatment reduced HR to basal levels. We propose that the stimulation of HR and NHEJ pathways may be an adaptive response of the cell to repair DNA damage mediated by bilirubin.
5. Conclusions
In spite of the many proposed mechanisms leading to neurotoxicity during neonatal severe hyperbilirubinemia, including oxidative stress, no data are available on DNA damage in vivo and in the response mechanisms triggered by hyperbilirubinemia.
The results presented here contribute to the understanding of the mechanisms associated with bilirubin neurotoxicity. We demonstrated that (a) DNA damage occurs in vivo in jaundiced newborn mice; (b) DNA damage is caused by bilirubin-induced oxidative stress; and (c) bilirubin treatment activates HR and NHEJ DNA repair mechanisms. Further studies are needed to reveal whether bilirubin-induced oxidative stress also results in RNA oxidation or affects the cell response at different levels.
We believe that these results are of relevance for neonates with severe hyperbilirubinemia and for patients suffering from the Crigler-Najjar syndrome, since DNA damage may contribute to neuronal death and bilirubin encephalopathy.
Acknowledgments
The work was supported by the International Centre for Genetic Engineering and Biotechnology intramural funds to AFM and by the FIF intramural grant to CT. Thanks are due to Sandra Leal for her help in the preparation of purified unconjugated bilirubin, to Eduard Ayuso and Lawrence Banks for fruitful discussions during the initial experimental design, and to Eleonora Vianello for her help in the initial experimental steps. The authors would like to thank Dr. Enrico Avvedimento for the kind gift of HeLa DR-GFP cells. The authors would also like to thank Dr. Marco Bestagno for his help with FACS analysis. Also, thanks are due to the animal house facility for the help in animal care.
Data Availability
The data used to support the findings of this study are included within the article and the Supplementary Materials.
Conflicts of Interest
The authors report no conflicts of interest.
Supplementary Materials
Supplementary Figure 1: bilirubin is toxic to SH-SY5Y cells. Supplementary Figure 2: cerebella from mutant mice show PARP activation. Supplementary Figure 3: bilirubin treatment affects the viability of HeLa cells. Supplementary Figure 4: data from Figure 4. FACS analysis data of homologous recombination experiments. Supplementary Figure 5: data from Figure 5. FACS analysis data of nonhomologous end joining experiments.
References
- 1.Gourley G. R. Bilirubin metabolism and kernicterus. Advances in Pediatrics. 1997;44:173–229. [PubMed] [Google Scholar]
- 2.Bosma P. J. Inherited disorders of bilirubin metabolism. Journal of Hepatology. 2003;38(1):107–117. doi: 10.1016/S0168-8278(02)00359-8. [DOI] [PubMed] [Google Scholar]
- 3.Watchko J. F., Tiribelli C. Bilirubin-induced neurologic damage — mechanisms and management approaches. The New England Journal of Medicine. 2013;369(21):2021–2030. doi: 10.1056/NEJMra1308124. [DOI] [PubMed] [Google Scholar]
- 4.Brites D. The evolving landscape of neurotoxicity by unconjugated bilirubin: role of glial cells and inflammation. Frontiers in Pharmacology. 2012;3:p. 88. doi: 10.3389/fphar.2012.00088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brito M. A., Brites D., Butterfield D. A. A link between hyperbilirubinemia, oxidative stress and injury to neocortical synaptosomes. Brain Research. 2004;1026(1):33–43. doi: 10.1016/j.brainres.2004.07.063. [DOI] [PubMed] [Google Scholar]
- 6.Brito M. A., Rosa A. I., Falcão A. S., et al. Unconjugated bilirubin differentially affects the redox status of neuronal and astroglial cells. Neurobiology of Disease. 2008;29(1):30–40. doi: 10.1016/j.nbd.2007.07.023. [DOI] [PubMed] [Google Scholar]
- 7.Brito M. A., Lima S., Fernandes A., et al. Bilirubin injury to neurons: contribution of oxidative stress and rescue by glycoursodeoxycholic acid. Neurotoxicology. 2008;29(2):259–269. doi: 10.1016/j.neuro.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 8.Genc S., Genc K., Kumral A., Baskin H., Ozkan H. Bilirubin is cytotoxic to rat oligodendrocytes in vitro. Brain Research. 2003;985(2):135–141. doi: 10.1016/S0006-8993(03)03037-3. [DOI] [PubMed] [Google Scholar]
- 9.Oakes G. H., Bend J. R. Early steps in bilirubin-mediated apoptosis in murine hepatoma (Hepa 1c1c7) cells are characterized by aryl hydrocarbon receptor-independent oxidative stress and activation of the mitochondrial pathway. Journal of Biochemical and Molecular Toxicology. 2005;19(4):244–255. doi: 10.1002/jbt.20086. [DOI] [PubMed] [Google Scholar]
- 10.Seubert J. M., Darmon A. J., El-Kadi A. O., D'Souza S. J., Bend J. R. Apoptosis in murine hepatoma hepa 1c1c7 wild-type, C12, and C4 cells mediated by bilirubin. Molecular Pharmacology. 2002;62(2):257–264. doi: 10.1124/mol.62.2.257. [DOI] [PubMed] [Google Scholar]
- 11.Cesaratto L., Calligaris S. D., Vascotto C., et al. Bilirubin-induced cell toxicity involves PTEN activation through an APE1/Ref-1-dependent pathway. Journal of Molecular Medicine. 2007;85(10):1099–1112. doi: 10.1007/s00109-007-0204-3. [DOI] [PubMed] [Google Scholar]
- 12.Deganuto M., Cesaratto L., Bellarosa C., et al. A proteomic approach to the bilirubin-induced toxicity in neuronal cells reveals a protective function of DJ-1 protein. Proteomics. 2010;10(8):1645–1657. doi: 10.1002/pmic.200900579. [DOI] [PubMed] [Google Scholar]
- 13.Daood M. J., Hoyson M., Watchko J. F. Lipid peroxidation is not the primary mechanism of bilirubin-induced neurologic dysfunction in jaundiced Gunn rat pups. Pediatric Research. 2012;72(5):455–459. doi: 10.1038/pr.2012.111. [DOI] [PubMed] [Google Scholar]
- 14.Yueh M. F., Chen S., Nguyen N., Tukey R. H. Developmental onset of bilirubin-induced neurotoxicity involves toll-like receptor 2-dependent signaling in humanized UDP-glucuronosyltransferase1 mice. The Journal of Biological Chemistry. 2014;289(8):4699–4709. doi: 10.1074/jbc.M113.518613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bortolussi G., Codarin E., Antoniali G., et al. Impairment of enzymatic antioxidant defenses is associated with bilirubin-induced neuronal cell death in the cerebellum of Ugt1 KO mice. Cell Death & Disease. 2015;6(5):p. e1739. doi: 10.1038/cddis.2015.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vodret S., Bortolussi G., Jasprova J., Vitek L., Muro A. F. Inflammatory signature of cerebellar neurodegeneration during neonatal hyperbilirubinemia in Ugt1 (−/−) mouse model. Journal of Neuroinflammation. 2017;14(1):p. 64. doi: 10.1186/s12974-017-0838-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cooke M. S., Evans M. D., Dizdaroglu M., Lunec J. Oxidative DNA damage: mechanisms, mutation, and disease. The FASEB Journal. 2003;17(10):1195–1214. doi: 10.1096/fj.02-0752rev. [DOI] [PubMed] [Google Scholar]
- 18.Kryston T. B., Georgiev A. B., Pissis P., Georgakilas A. G. Role of oxidative stress and DNA damage in human carcinogenesis. Mutation Research. 2011;711(1-2):193–201. doi: 10.1016/j.mrfmmm.2010.12.016. [DOI] [PubMed] [Google Scholar]
- 19.Karakukcu C., Ustdal M., Ozturk A., Baskol G., Saraymen R. Assessment of DNA damage and plasma catalase activity in healthy term hyperbilirubinemic infants receiving phototherapy. Mutation Research. 2009;680(1-2):12–16. doi: 10.1016/j.mrgentox.2009.07.016. [DOI] [PubMed] [Google Scholar]
- 20.Karadag A., Demirin H., Dogan D. G., Aslan M., Tatli M. M. Phototherapy, hyperbilirubinemia and genotoxicity in newborns. Mutation Research. 2010;697(1-2):p. 68. doi: 10.1016/j.mrgentox.2010.01.005. author reply 69. [DOI] [PubMed] [Google Scholar]
- 21.Tatli M. M., Minnet C., Kocyigit A., Karadag A. Phototherapy increases DNA damage in lymphocytes of hyperbilirubinemic neonates. Mutation Research. 2008;654(1):93–95. doi: 10.1016/j.mrgentox.2007.06.013. [DOI] [PubMed] [Google Scholar]
- 22.Ramy N., Ghany E. A., Alsharany W., et al. Jaundice, phototherapy and DNA damage in full-term neonates. Journal of Perinatology. 2016;36(2):132–136. doi: 10.1038/jp.2015.166. [DOI] [PubMed] [Google Scholar]
- 23.Mesbah-Namin S. A., Shahidi M., Nakhshab M. An increased genotoxic risk in lymphocytes from phototherapy-treated hyperbilirubinemic neonates. Iranian Biomedical Journal. 2017;21(3):182–189. doi: 10.18869/acadpub.ibj.21.3.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yahia S., Shabaan A. E., Gouida M., et al. Influence of hyperbilirubinemia and phototherapy on markers of genotoxicity and apoptosis in full-term infants. European Journal of Pediatrics. 2015;174(4):459–464. doi: 10.1007/s00431-014-2418-z. [DOI] [PubMed] [Google Scholar]
- 25.Hachiya Y., Hayashi M. Bilirubin encephalopathy: a study of neuronal subpopulations and neurodegenerative mechanisms in 12 autopsy cases. Brain & Development. 2008;30(4):269–278. doi: 10.1016/j.braindev.2007.08.013. [DOI] [PubMed] [Google Scholar]
- 26.Wallner M., Antl N., Rittmannsberger B., et al. Anti-genotoxic potential of bilirubin in vivo: damage to DNA in hyperbilirubinemic human and animal models. Cancer Prevention Research. 2013;6(10):1056–1063. doi: 10.1158/1940-6207.CAPR-13-0125. [DOI] [PubMed] [Google Scholar]
- 27.Bortolussi G., Baj G., Vodret S., Viviani G., Bittolo T., Muro A. F. Age-dependent pattern of cerebellar susceptibility to bilirubin neurotoxicity in vivo in mice. Disease Models & Mechanisms. 2014;7(9):1057–1068. doi: 10.1242/dmm.016535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bortolussi G., Zentilin L., Baj G., et al. Rescue of bilirubin-induced neonatal lethality in a mouse model of Crigler-Najjar syndrome type I by AAV9-mediated gene transfer. The FASEB Journal. 2012;26(3):1052–1063. doi: 10.1096/fj.11-195461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cuozzo C., Porcellini A., Angrisano T., et al. DNA damage, homology-directed repair, and DNA methylation. PLoS Genetics. 2007;3(7, article e110) doi: 10.1371/journal.pgen.0030110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ostrow J. D., Mukerjee P., Tiribelli C. Structure and binding of unconjugated bilirubin: relevance for physiological and pathophysiological function. Journal of Lipid Research. 1994;35(10):1715–1737. [PubMed] [Google Scholar]
- 31.Roca L., Calligaris S., Wennberg R. P., et al. Factors affecting the binding of bilirubin to serum albumins: validation and application of the peroxidase method. Pediatric Research. 2006;60(6):724–728. doi: 10.1203/01.pdr.0000245992.89965.94. [DOI] [PubMed] [Google Scholar]
- 32.Giraudi P. J., Bellarosa C., Coda-Zabetta C. D., Peruzzo P., Tiribelli C. Functional induction of the cystine-glutamate exchanger system Xc − activity in SH-SY5Y cells by unconjugated bilirubin. PLoS One. 2011;6(12, article e29078) doi: 10.1371/journal.pone.0029078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bortolussi G., Zentillin L., Vaníkova J., et al. Life-long correction of hyperbilirubinemia with a neonatal liver-specific AAV-mediated gene transfer in a lethal mouse model of Crigler Najjar syndrome. Human Gene Therapy. 2014;25(9):844–855. doi: 10.1089/hum.2013.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mah L. J., El-Osta A., Karagiannis T. C. γH2AX: a sensitive molecular marker of DNA damage and repair. Leukemia. 2010;24(4):679–686. doi: 10.1038/leu.2010.6. [DOI] [PubMed] [Google Scholar]
- 35.Calligaris R., Bellarosa C., Foti R., et al. A transcriptome analysis identifies molecular effectors of unconjugated bilirubin in human neuroblastoma SH-SY5Y cells. BMC Genomics. 2009;10(1):p. 543. doi: 10.1186/1471-2164-10-543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Qaisiya M., Brischetto C., Jasprova J., Vitek L., Tiribelli C., Bellarosa C. Bilirubin-induced ER stress contributes to the inflammatory response and apoptosis in neuronal cells. Archives of Toxicology. 2017;91(4):1847–1858. doi: 10.1007/s00204-016-1835-3. [DOI] [PubMed] [Google Scholar]
- 37.Qaisiya M., Coda Zabetta C. D., Bellarosa C., Tiribelli C. Bilirubin mediated oxidative stress involves antioxidant response activation via Nrf2 pathway. Cellular Signalling. 2014;26(3):512–520. doi: 10.1016/j.cellsig.2013.11.029. [DOI] [PubMed] [Google Scholar]
- 38.Swindall A. F., Stanley J. A., Yang E. S. PARP-1: friend or foe of DNA damage and repair in tumorigenesis? Cancers. 2013;5(4):943–958. doi: 10.3390/cancers5030943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pierce A. J., Johnson R. D., Thompson L. H., Jasin M. XRCC3 promotes homology-directed repair of DNA damage in mammalian cells. Genes & Development. 1999;13(20):2633–2638. doi: 10.1101/gad.13.20.2633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jasin M. Genetic manipulation of genomes with rare-cutting endonucleases. Trends in Genetics. 1996;12(6):224–228. doi: 10.1016/0168-9525(96)10019-6. [DOI] [PubMed] [Google Scholar]
- 41.Bennardo N., Cheng A., Huang N., Stark J. M. Alternative-NHEJ is a mechanistically distinct pathway of mammalian chromosome break repair. PLoS Genetics. 2008;4(6, article e1000110) doi: 10.1371/journal.pgen.1000110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stocker R., Yamamoto Y., McDonagh A. F., Glazer A. N., Ames B. N. Bilirubin is an antioxidant of possible physiological importance. Science. 1987;235(4792):1043–1046. doi: 10.1126/science.3029864. [DOI] [PubMed] [Google Scholar]
- 43.Bulmer A. C., Blanchfield J. T., Toth I., Fassett R. G., Coombes J. S. Improved resistance to serum oxidation in Gilbert’s syndrome: a mechanism for cardiovascular protection. Atherosclerosis. 2008;199(2):390–396. doi: 10.1016/j.atherosclerosis.2007.11.022. [DOI] [PubMed] [Google Scholar]
- 44.Vitek L., Ostrow J. D. Bilirubin chemistry and metabolism; harmful and protective aspects. Current Pharmaceutical Design. 2009;15(25):2869–2883. doi: 10.2174/138161209789058237. [DOI] [PubMed] [Google Scholar]
- 45.Bulmer A. C., Verkade H. J., Wagner K. H. Bilirubin and beyond: a review of lipid status in Gilbert’s syndrome and its relevance to cardiovascular disease protection. Progress in Lipid Research. 2013;52(2):193–205. doi: 10.1016/j.plipres.2012.11.001. [DOI] [PubMed] [Google Scholar]
- 46.Vítek L., Jirsa M., Jr, Brodanová M., et al. Gilbert syndrome and ischemic heart disease: a protective effect of elevated bilirubin levels. Atherosclerosis. 2002;160(2):449–456. doi: 10.1016/S0021-9150(01)00601-3. [DOI] [PubMed] [Google Scholar]
- 47.Novotny L., Vitek L. Inverse relationship between serum bilirubin and atherosclerosis in men: a meta-analysis of published studies. Experimental Biology and Medicine. 2003;228(5):568–571. doi: 10.1177/15353702-0322805-29. [DOI] [PubMed] [Google Scholar]
- 48.Perlstein T. S., Pande R. L., Creager M. A., Weuve J., Beckman J. A. Serum total bilirubin level, prevalent stroke, and stroke outcomes: NHANES 1999-2004. The American Journal of Medicine. 2008;121(9):781–788.e1. doi: 10.1016/j.amjmed.2008.03.045. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kundur A. R., Singh I., Bulmer A. C. Bilirubin, platelet activation and heart disease: a missing link to cardiovascular protection in Gilbert’s syndrome? Atherosclerosis. 2015;239(1):73–84. doi: 10.1016/j.atherosclerosis.2014.12.042. [DOI] [PubMed] [Google Scholar]
- 50.Jangi S., Otterbein L., Robson S. The molecular basis for the immunomodulatory activities of unconjugated bilirubin. The International Journal of Biochemistry & Cell Biology. 2013;45(12):2843–2851. doi: 10.1016/j.biocel.2013.09.014. [DOI] [PubMed] [Google Scholar]
- 51.Molzer C., Huber H., Steyrer A., et al. Bilirubin and related tetrapyrroles inhibit food-borne mutagenesis: a mechanism for antigenotoxic action against a model epoxide. Journal of Natural Products. 2013;76(10):1958–1965. doi: 10.1021/np4005807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Horsfall L. J., Nazareth I., Pereira S. P., Petersen I. Gilbert’s syndrome and the risk of death: a population-based cohort study. Journal of Gastroenterology and Hepatology. 2013;28(10):1643–1647. doi: 10.1111/jgh.12279. [DOI] [PubMed] [Google Scholar]
- 53.Horsfall L. J., Nazareth I., Petersen I. Cardiovascular events as a function of serum bilirubin levels in a large, statin-treated cohort. Circulation. 2012;126(22):2556–2564. doi: 10.1161/CIRCULATIONAHA.112.114066. [DOI] [PubMed] [Google Scholar]
- 54.Shapiro S. M. Bilirubin toxicity in the developing nervous system. Pediatric Neurology. 2003;29(5):410–421. doi: 10.1016/j.pediatrneurol.2003.09.011. [DOI] [PubMed] [Google Scholar]
- 55.Hoeijmakers J. H. J. Genome maintenance mechanisms for preventing cancer. Nature. 2001;411(6835):366–374. doi: 10.1038/35077232. [DOI] [PubMed] [Google Scholar]
- 56.Ollinger R., Bilban M., Erat A., et al. Bilirubin: a natural inhibitor of vascular smooth muscle cell proliferation. Circulation. 2005;112(7):1030–1039. doi: 10.1161/CIRCULATIONAHA.104.528802. [DOI] [PubMed] [Google Scholar]
- 57.Ollinger R., Kogler P., Troppmair J., et al. Bilirubin inhibits tumor cell growth via activation of ERK. Cell Cycle. 2007;6(24):3078–3085. doi: 10.4161/cc.6.24.5022. [DOI] [PubMed] [Google Scholar]
- 58.Ollinger R., Yamashita K., Bilban M., et al. Bilirubin and biliverdin treatment of atherosclerotic diseases. Cell Cycle. 2007;6(1):39–43. doi: 10.4161/cc.6.1.3700. [DOI] [PubMed] [Google Scholar]
- 59.Rao P., Suzuki R., Mizobuchi S., Yamaguchi T., Sasaguri S. Bilirubin exhibits a novel anti-cancer effect on human adenocarcinoma. Biochemical and Biophysical Research Communications. 2006;342(4):1279–1283. doi: 10.1016/j.bbrc.2006.02.074. [DOI] [PubMed] [Google Scholar]
- 60.Robert M. C., Furlan G., Rosso N., et al. Alterations in the cell cycle in the cerebellum of hyperbilirubinemic Gunn rat: a possible link with apoptosis? PLoS One. 2013;8(11, article e79073) doi: 10.1371/journal.pone.0079073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Vodret S., Bortolussi G., Schreuder A. B., et al. Albumin administration prevents neurological damage and death in a mouse model of severe neonatal hyperbilirubinemia. Scientific Reports. 2015;5(1):p. 16203. doi: 10.1038/srep16203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Carrillo M. C., Kanai S., Sato Y., Kitani K. Age-related changes in antioxidant enzyme activities are region and organ, as well as sex, selective in the rat. Mechanisms of Ageing and Development. 1992;65(2-3):187–198. doi: 10.1016/0047-6374(92)90035-C. [DOI] [PubMed] [Google Scholar]
- 63.Haagsma E. B., Hagens V. E., Schaapveld M., et al. Increased cancer risk after liver transplantation: a population-based study. Journal of Hepatology. 2001;34(1):84–91. doi: 10.1016/S0168-8278(00)00077-5. [DOI] [PubMed] [Google Scholar]
- 64.Herrero J. I., Lorenzo M., Quiroga J., et al. De novo neoplasia after liver transplantation: an analysis of risk factors and influence on survival. Liver Transplantation. 2005;11(1):89–97. doi: 10.1002/lt.20319. [DOI] [PubMed] [Google Scholar]
- 65.Sellier A. L., Labrune P., Kwon T., Boudjemline A. M., Deschenes G., Gajdos V. SSIEM. JIMD Reports - Case and Research Reports, 2011/2. JIMD Reports, vol 2. Berlin, Heidelberg: Springer; 2011. Successful plasmapheresis for acute and severe unconjugated hyperbilirubinemia in a child with Crigler Najjar type I syndrome; pp. 33–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chan P. H. Reactive oxygen radicals in signaling and damage in the ischemic brain. Journal of Cerebral Blood Flow and Metabolism. 2001;21(1):2–14. doi: 10.1097/00004647-200101000-00002. [DOI] [PubMed] [Google Scholar]
- 67.Shapiro S. M. Definition of the clinical spectrum of kernicterus and bilirubin-induced neurologic dysfunction (BIND) Journal of Perinatology. 2005;25(1):54–59. doi: 10.1038/sj.jp.7211157. [DOI] [PubMed] [Google Scholar]
- 68.Shapiro S. M., Bhutani V. K., Johnson L. Hyperbilirubinemia and kernicterus. Clinics in Perinatology. 2006;33(2):387–410. doi: 10.1016/j.clp.2006.03.010. [DOI] [PubMed] [Google Scholar]
- 69.Lieber M. R. The mechanism of human nonhomologous DNA end joining. The Journal of Biological Chemistry. 2008;283(1):1–5. doi: 10.1074/jbc.R700039200. [DOI] [PubMed] [Google Scholar]
- 70.San Filippo J., Sung P., Klein H. Mechanism of eukaryotic homologous recombination. Annual Review of Biochemistry. 2008;77(1):229–257. doi: 10.1146/annurev.biochem.77.061306.125255. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figure 1: bilirubin is toxic to SH-SY5Y cells. Supplementary Figure 2: cerebella from mutant mice show PARP activation. Supplementary Figure 3: bilirubin treatment affects the viability of HeLa cells. Supplementary Figure 4: data from Figure 4. FACS analysis data of homologous recombination experiments. Supplementary Figure 5: data from Figure 5. FACS analysis data of nonhomologous end joining experiments.
Data Availability Statement
The data used to support the findings of this study are included within the article and the Supplementary Materials.