Abstract
Objective
Statins have several pleiotropic effects, but the literature regarding the possible relationship between statins use and outcomes in knee osteoarthritis (OA) is limited. We investigated whether statins use is associated with lower risk of radiographic (ROA), radiographic symptomatic knee OA (SxOA) and pain in North American people.
Methods
A total of 4,448 community-dwelling adults from the Osteoarthritis Initiative were followed-up for 4 years. Statins use (including the time from baseline and the type) was defined through self-report information and confirmed by a trained interviewer. Knee OA outcomes included incident (1) ROA, (2) SxOA, as the new onset of a combination of a painful knee and ROA, (3) knee pain worsening, i.e. a Western Ontario and McMaster Universities Osteoarthritis Index difference between baseline and each annual exam ≥14%.
Results
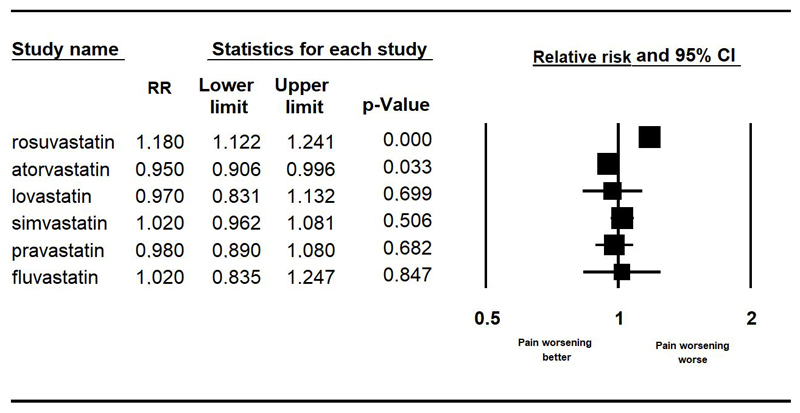
At baseline, 1,127 participants (=25.3%) used statins. Based on a multivariable Poisson regression analysis with robust variance estimators, any statins use was not associated with lower risk of pain worsening (relative risk, RR=0.97; 95%CI, confidence intervals: 0.93-1.02), incident ROA or SxOA. However, statins use > 5 years (RR=0.91; 95%CI: 0.83-0.997) and atorvastatin use (RR=0.95; 95%CI: 0.91-0.996) were associated with a reduced risk of developing pain, whilst rosuvastatin to a higher risk (RR=1.18; 95%CI: 1.12-1.24). The adjustment for the propensity score confirmed these findings.
Conclusion
The effect of statins use on knee OA outcomes remains unclear, although in our study those using statins for over five years and those using atorvastatin reported a significant lower risk of developing knee pain.
Keywords: osteoarthritis, statins, aged, Osteoarthritis Initiative, pain, knee osteoarthritis
Introduction
Statins are competitive inhibitors of hydroxymethyl-glutaryl-coenzyme reductase, an enzyme involved in the cholesterol biosynthesis.(1) These medications are commonly used for treating hypercholesterolemia.(1, 2) In addition to their primary indication, there is growing evidence that statins also have important pleiotropic effects, such as the improvement of endothelial dysfunction, stabilization of atherosclerotic plaques, increased nitric oxide bioavailability, antioxidant properties, and inhibition of inflammatory responses.(1, 3)
Inflammation plays a pivotal role in the development and progression of knee osteoarthritis (OA)(4, 5), the most common form of osteoarthritis worldwide.(6) It was reported that statins have multiple effects on inflammation at cellular and extra-cellular level, including reduction in inflammatory cytokines and T cell activation.(7) Given that many of these systems are influential on OA, it is possible that statins may have a role in altering the course of the progression of knee OA and its symptomatology, which may be counteracted by the well-known muscle ache, developed under long-term statins use. In fact, statin use has a well-established side effect of muscle ache and statins exacerbate declines in muscle performance and lead to increase in falls risk, that are associated with aging, without a significant decrease in muscle mass.(8)
The literature regarding the effect of statins on OA outcomes (such as progression and pain) is, however, limited to a few studies. In the Rotterdam study, 2,921 older participants were followed-up over 6.5 years. In this research, statins use was associated with more than a 50% reduction in overall progression of knee OA.(9) However, in another large cohort with a follow-up of 8 years, older women taking statins at baseline were found to be at an increased risk of hip OA(10), whilst the authors did not report any data regarding knee OA. Although these studies have advanced our knowledge regarding the effect of statins use in OA, some limitations and unanswered questions persist. First, only a radiographical diagnosis of OA was used. Therefore, the effect of statins on pain due to OA is not known, but could be of clinical importance.(11) Second, the number of covariates used for adjustments was generally low introducing possible residual confounding in these findings. Finally, these studies did not use propensity score matching, a method that seems the most appropriate in comparing the effect of medications in observational studies.(12)
Given this background, we aimed to investigate whether statins use is associated with lower risk of radiographic (ROA), radiographic symptomatic knee OA (SxOA) and pain worsening due to knee OA, in a large cohort of North American people followed-up for 4 years.
Materials and Methods
Data source and subjects
Data were obtained from the Osteoarthritis Initiative (OAI) database (http://www.oai.ucsf.edu/). Within the OAI, participants were recruited across four clinical sites in the United States of America (Baltimore, MD; Pittsburgh, PA; Pawtucket, RI; and Columbus, OH) between February 2004 and May 2006. In this project, people were included if they: (1) had knee OA with knee pain for a 30-day period in the past 12 months or (2) were at high risk of developing knee OA (e.g. obese/overweight, familiarity for knee OA).(13) The data were collected during the baseline and in screening evaluations and in subsequent evaluations until four years of follow-up. All participants provided written informed consent. The OAI study was given full ethics approval by the institutional review board of the OAI Coordinating Center, at the University of California in San Francisco.
Use of statins (exposure)
Statins use was assessed at baseline using a specific questionnaire investigating the name of the prescription medicine, duration of use, and formulation code in the 30 days before the interview. Trained interviewers checked the medications used by each participant. The statins included in the interview were: rosuvastatin, atorvastatin, lovastatin, simvastatin, pravastatin, fluvastatin. The duration of use of these medications were recorded in the OAI at baseline evaluation and categorized as: < 1 month, between 1 month and < 1 year, between 1 and < 3 years, between 3 and < 5 years and more than 5 years. Statins use during follow-up was also recorded and used in the analysis.
Assessment of knee OA outcomes
At baseline and during follow-up examinations, individuals had full knee assessments which included both a clinical and radiographic examination. People with knee replacement at baseline were removed from all the analyses. A fixed flexion posterior–anterior radiograph, which was read centrally for Kellgren and Lawrence (KL) grade, was made for all the participants. In addition, participants were asked regarding knee pain, the following question: ‘During the past 30 days, have you had pain, aching, or stiffness in your right/left knee on most days?’. Knee pain was also assessed using the WOMAC (Western Ontario and McMaster Universities Osteoarthritis Index) pain subscale. This scale ranges from 0 (absence of pain) to 20 (highest pain) points.
The knee outcomes of interest for this study included: incident (1) ROA (radiographical osteoarthritis), if a knee developed a KL grade ≥2 at follow-up and was not present at baseline, (2) SxOA (symptomatic osteoarthritis), defined as new onset of a combination of painful knee plus the presence of ROA present at the same side and (3) knee pain worsening, i.e. WOMAC pain score difference of a knee between baseline and each annual exam ≥14% or the onset of pain during follow-up in people having zero at baseline in accordance with previous research.(14, 15) The assessment of these knee OA outcomes was made, other than at baseline, at V01 (12 months), V03 (24 months), V05 (36 months), and V06 (48 months).
Covariates
Ten covariates at baseline (other than age and sex) were identified as potential confounding factors based on previous literature.(16) These included: race (whites vs. others); educational attainment (college or higher vs. others); body mass index (BMI); yearly income (< vs ≥ $50,000 or missing data); depressive symptoms assessed using the Center for Epidemiologic Studies Depression Scale (CES-D)(17); smoking habits; physical activity evaluated using the total score for the Physical Activity Scale for the Elderly scale (PASE)(18); Charlson Comorbidity Index score(19), a validated general health measure of self-reported comorbidities; the number of medications used; the maximum knee extension strength (between left and right lower limb), after three trials for each side. Statins use during follow-up was also recorded and used as covariate.
Statistical analyses
Data on continuous variables were normally distributed according to the Kolmogorov-Smirnov test. Data were presented as means and standard deviation values (SD) for quantitative measures, and percentages for all categorical variables by the use or not of statins at baseline. P values were calculated using an independent T test for continuous variables and a chi-square test for categorical parameters.
To assess the relationship between statins use and the outcomes (ROA, SxOA, pain worsening), a multivariable Poisson regression analysis with robust variance estimators was applied, since a survival analysis was not possible due to lack of information on the precise date of event. The fully adjusted model included age; sex; race (whites vs. others); education (degree vs. others); body mass index (as continuous); yearly income (categorized as ≥ or < 50,000$ and missing data); CES-D: Center for Epidemiologic Studies Depression Scale; smoking habits (current and previous vs. others); Physical Activity Scale for Elderly score (as continuous); Charlson co-morbidity index; number of medications used; use of statins during follow-up period; maximum knee extension. Multi-collinearity among covariates was assessed through variance inflation factor (VIF)(20), taking a cut-off of 2 as the criterion for exclusion. No covariates were excluded using this criterion. Adjusted relative risks (RRs) and 95% confidence intervals (CI) were calculated to estimate the strength of the associations between statins use and incident knee OA outcomes.
We ran several sensitivity analyses assessing the association between statins use and incident knee OA outcomes. First, we used the propensity score that is a statistical matching technique that attempts to estimate the effect of a treatment by accounting for the covariates that predict receiving the treatment.(12) The propensity score, divided into quintiles, was estimated by using a logistic regression model regressing baseline statins use on the above-mentioned covariates. Second, we ran an analysis using the periods of use of statins from baseline evaluation (as defined before) as exposure. Finally, we used the type of statin (rosuvastatin, atorvastatin, lovastatin, simvastatin, pravastatin, fluvastatin) as the exposure. In all these elaborations, people not using statins were taken as the reference group.
A p<0.05 was deemed statistically significant. All analyses were performed using SPSS® software version 17.0 for Windows (SPSS Inc., Chicago, Illinois) and STATA® software version 14.1 (Stata Corp LP, College station, Texas).
Results
Sample selection
The OAI dataset initially included a total of 4,796 individuals. We excluded 63 participants with a total knee replacement at baseline (since they cannot develop any of the outcomes of interest) and a further 285 with no data regarding outcomes of interest during follow-up, obtaining a final sample of 4,448 people.
Descriptive characteristics
The cohort consisted of 2,584 females (58.1%) and 1,864 males (41.9%), with a mean age of 61.1 years (±9.2 years; range: 45-79 years). Of the entire cohort, 1,127 participants (=25.3% of population) used statins at baseline, mainly for a period between one month and one year (=10.4%) from baseline. The most frequent statin use reported was atorvastatin, used by 603 people (=13.6%). At baseline, 2,512 had knee ROA (=56.5% of baseline population) and, of them, 1,082 had knee SxOA (=24.3%).
Table 1 shows the baseline characteristics by statins use or not. Compared to the 3,321 participants not using statins, people using statins were older, and were more likely to be males, sedentary, whites, and smokers. People using statins were more obese and had a higher number of co-morbidities, using a higher number of medications. Finally, people using statins had a significant higher prevalence of knee ROA (59.4 vs. 55.5, p=0.02) and reported a higher level of WOMAC pain at both knees (p=0.001 for right knee and =0.002 at left knee). However, no difference emerged for the prevalence of knee SxOA (Table 1).
Table 1. Characteristics of the participants classified according to their baseline use of statins.
| Statins users (n=1127) |
No statins users (n=3321) |
p-value | |
|---|---|---|---|
| General characteristics | |||
| Age (years) | 64.3 (8.4) | 60.0 (9.2) | <0.0001 |
| Males (%) | 46.9 | 40.2 | <0.0001 |
| PASE (points) | 149 (75) | 167 (84) | <0.0001 |
| White race (%) | 82.1 | 79.5 | 0.05 |
| Smoking (previous/current) (%) | 51.3 | 45.3 | 0.001 |
| Graduate degree (%) | 30.3 | 31.3 | 0.55 |
| Yearly income (≥ $50,000) (%) | 57.8 | 60.1 | 0.34 |
| Knee extension (Nm) | 356 (129) | 356 (133) | 0.93 |
| Medical conditions | |||
| BMI (Kg/m2) | 29.5 (4.4) | 28.3 (4.9) | <0.0001 |
| CES-D (points) | 6.3 (6.3) | 6.6 (7.1) | 0.20 |
| Charlson co-morbidity index (points) | 0.6 (1.0) | 0.3 (0.8) | <0.0001 |
| Number of medications | 4.5 (2.6) | 2.4 (2.5) | <0.0001 |
| Osteoarthritis items (at baseline) | |||
| ROA (%) | 59.4 | 55.5 | 0.02 |
| SxOA (%) | 25.4 | 24.0 | 0.36 |
| WOMAC pain (right knee) | 0.5 (0.5) | 0.4 (0.5) | 0.001 |
| WOMAC pain (left knee) | 0.5 (0.5) | 0.4 (0.5) | 0.002 |
Notes: The data are presented as means (with standard deviations) for continuous variables and percentages for categorical outcomes.
Abbreviations: CES-D: Center for Epidemiologic Studies Depression Scale; PASE: Physical Activity Scale for the Elderly; BMI: body mass index; OA: osteoarthritis; WOMAC: Western Ontario and McMaster Universities Osteoarthritis Index.
Statins use and incident knee osteoarthritis outcomes
During the four years of follow-up, 431 people developed ROA. Of them, 201 had a SxOA. Pain worsening was observed in 3,678 subjects.
As shown in Table 2, during a mean follow-up period of 4 years, after adjusting for potential confounders at baseline and statins use during follow-up, participants using any statins did not report significant lower risk of pain worsening (RR=0.97; 95%CI: 0.93-1.02; p=0.23) and no differences emerged for incident knee ROA (RR=1.31; 95%CI: 0.83-2.09; p=0.25) or for knee SxOA (RR=0.97; 95%CI: 0.87-1.09; p=0.63) either. The adjustment for the propensity score substantially confirmed these findings.
Table 2. Association between baseline use of statins and incident knee osteoarthritis outcomes.
| Number of events/number of participants |
Full-adjusted model1 (RR, 95%CI) |
p-value | Propensity-score model2 (RR, 95%CI) |
p-value | |
|---|---|---|---|---|---|
| Pain worsening | 3,678/4,448 (=82.7%) | 0.97 (0.93-1.02) | 0.23 | 0.97 (0.93-1.02) | 0.24 |
| ROA | 431/1,936 (=22.2%) | 1.31 (0.83-2.09) | 0.25 | 1.41 (0.86-2.32) | 0.17 |
| SxOA | 201/3,364 (=5.9%) | 0.97 (0.87-1.09) | 0.63 | 0.98 (0.88-1.11) | 0.78 |
Notes:
All the data are presented as relative risk with their 95% confidence intervals.
Fully adjusted model included as covariates: age (as continuous); sex; race (whites vs. others); education (degree vs. others); body mass index (as continuous); yearly income (categorized as ≥ or < 50,000$ and missing data); CES-D: Center for Epidemiologic Studies Depression Scale; smoking habits (current and previous vs. others); Physical Activity Scale for Elderly score (as continuous); Charlson co-morbidity index; number of medications used; use of statins during follow-up period; maximum knee extension.
Propensity score model included as covariate the propensity score divided into quintiles.
Abbreviations: CI: confidence intervals; RR: relative risk.
In Table 3, we assessed the association between period of use of statins and incident knee OA outcomes. Only the use of a period of more than 5 years was associated with a decrease in pain during the follow-up period (RR=0.91; 95%CI: 0.83-0.997; p=0.04 in fully-adjusted model; RR=0.90; 95%CI: 0.82-0.993; p=0.03 after adjusting for the propensity-score). We did not observe any significant associations between statins use and radiographic or symptomatic knee OA for the other periods of use included (Table 2).
Table 3. Association between duration of use of statins and incident knee osteoarthritis outcomes.
| Full-adjusted model1 (RR, 95%CI) |
p-value | Propensity-score model2 (RR, 95%CI) |
p-value | |
|---|---|---|---|---|
| Pain worsening | ||||
| < 1 month | 0.95 (0.84-1.08) | 0.50 | 0.96 (0.85-1.09) | 0.56 |
| 1 month to 1 year | 0.96 (0.91-1.02) | 0.19 | 0.96 (0.91-1.02) | 0.18 |
| 1-3 years | 1.05 (0.995-1.12) | 0.07 | 1.06 (0.996-1.18) | 0.07 |
| 3-5 years | 0.96 (0.89-1.04) | 0.35 | 0.96 (0.89-1.05) | 0.40 |
| >5 years | 0.91 (0.83-0.997) | 0.04 | 0.90 (0.82-0.993) | 0.03 |
| Radiographic osteoarthritis | ||||
| < 1 month | 0.85 (0.19-3.76) | 0.83 | 0.92 (0.22-3.82) | 0.91 |
| 1 month to 1 year | 1.32 (0.76-2.31) | 0.32 | 1.45 (0.80-2.64) | 0.22 |
| 1-3 years | 1.26 (0.63-2.49) | 0.51 | 1.33 (0.68-2.66) | 0.42 |
| 3-5 years | 1.31 (0.59-2.88) | 0.51 | 1.32 (0.58-3.02) | 0.50 |
| >5 years | 1.49 (0.74-3.01) | 0.26 | 1.64 (0.80-3.37) | 0.18 |
| Symptomatic osteoarthritis | ||||
| < 1 month | 0.88 (0.66-1.16) | 0.35 | 1.10 (0.82-1.47) | 0.53 |
| 1 month to 1 year | 0.96 (0.84-1.11) | 0.61 | 0.97 (0.84-1.12) | 0.66 |
| 1-3 years | 1.01 (0.85-1.20) | 0.89 | 1.01 (0.85-1.21) | 0.87 |
| 3-5 years | 1.02 (0.84-1.25) | 0.85 | 1.03 (0.84-1.27) | 0.75 |
| >5 years | 0.93 (0.74-1.16) | 0.50 | 0.90 (0.72-1.12) | 0.35 |
Notes:
All the data are presented as relative risk with their 95% confidence intervals, taking those not using statins as reference.
Fully adjusted model included as covariates: age (as continuous); sex; race (whites vs. others); education (degree vs. others); body mass index (as continuous); yearly income (categorized as > or < 50,000$ and missing data); CES-D: Center for Epidemiologic Studies Depression Scale; smoking habits (current and previous vs. others); Physical Activity Scale for Elderly score (as continuous); Charlson co-morbidity index; number of medications used; use of statins during follow-up period; maximum knee extension.
Propensity score model included as covariate the propensity score divided into quintiles.
Abbreviations: CI: confidence intervals; RR: odds relative risk.
Regarding individual agents, atorvastatin was the only statin associated with a lower risk of pain worsening (RR=0.95; 95%CI: 0.91-0.996; p=0.03), whilst rosuvastatin was associated with a higher risk of pain worsening (RR=1.18; 9%%CI: 1.12-1.24; p<0.0001), as reported in Figure 1. No statins were associated with a significant effect on incident ROA or SxOA (details not shown, available on request from corresponding author).
Figure 1. Association between type of statins and pain worsening during follow-up, adjusted for the propensity score in quintiles.
Data are reported as odds ratios with 95% confidence intervals (CIs), adjusted for the propensity score, taking people not using statins as reference.
Discussion
In this large longitudinal study over a 4-year follow-up period, our results suggest that statins use is not associated with a lower risk of pain worsening, symptomatic and radiographic knee OA when the time of statins use and the type of statin was not taken into account. However, using statins for more than 5 years from baseline and atorvastatin use were associated with reduced pain worsening as well as rosuvastatin to a higher risk.
It was reported that statins may have several positive effects on knee OA outcomes due to several reasons. First, the anti-inflammatory effect can contribute to the reduction in pain worsening during follow-up that we observed. However, the effect of statins on musculoskeletal pain is probably contradictory and can overcome the anti-inflammatory properties of these medications. It is traditionally known that statins might lead to muscular pain as side effect(21), but a large randomized controlled trial (RCT) in people affected by rheumatoid arthritis reported a significant reduction of atorvastatin on pain, mainly due to a reduction in inflammatory parameters.(22) The association between statins and decrease in pain has been confirmed in some other observational studies.(23) There is however more limited data regarding OA. In a longitudinal study, among 16,609 participants with previous cardiovascular disease followed-up for 10 years, higher statin dose and larger statin dose increments were associated with a reduction in clinically defined OA outcome.(24) Unfortunately, the diagnosis of knee OA in this study was made through administrative data, limiting their reliability. (24) Therefore, future studies (particularly RCTs) are needed to understand if statins use can really decrease pain in people affected by knee OA. Second, statins may positively affect subchondral bone, another part usually damaged in knee OA.(25) Damaged subchondral bone in OA may result in vascular disease (particularly of small vessels), with localized vascular hypertension and ischemia that can further worsen progression.(26) Since statins cause vasodilatation and have anti-atherosclerotic effect, it is likely that these properties balance the negative effect on subchondral bone.(7) However, subchondral bone is better visualized through magnetic resonance imaging and therefore, we were unable to confirm the possible role of statins on this structure in our study.
Another interesting finding of our research is that statins did not decrease the incidence of symptomatic and radiographic knee OA, which is in contrast to earlier cohort studies.(9, 24) We can hypothesize that some methodological aspects can influence these results. For example, the OAI includes only people with knee OA or at high risk of this condition. Furthermore, the diagnostic criteria used for the definition of symptomatic and radiographic knee OA, and the covariates used for adjustment in the analyses differed between studies. Due to the importance of these outcomes, future studies are needed to better understand if statins are able to modify the natural history of knee OA.
Finally, we found that statins use for more than 5 years was associated with lower risk of pain worsening. Overall, our research confirmed previous findings coming from large RCTs on cardiovascular disease and hypercholesterolemia, indicating that a benefit of statins remains more than 5 years and linearly increases with the duration of use.(27) Similarly, we found that people taking atorvastatin at baseline had a significant decreased risk in pain worsening of about 5%. Atorvastatin is a lipophilic statin(28) and it is known that, in in vitro models, lipophilic statins can block cartilage collagen breakdown induced by proinflammatory cytokines and by downregulating key cartilage-degrading enzymes in bovine nasal cartilage.(29) These authors, however, found these interesting effects only on other two lipophilic statins (simvastatin and mevastatin) for which, on the contrary, we failed to find any significant association. Therefore, other research is needed to confirm/refute our findings and to understand if the effect of lovastatin on pain worsening is peculiar or not. At the same time, another potent statin (rosuvastatin) increased the risk of pain worsening due to knee OA suggesting that hydrophilic statins may lead to an increase in pain more frequently than lipophilic ones. However other studies are needed to confirm our findings.
The strengths of our study are the long duration of follow-up, the several knee OA outcomes assessed, and the large sample size included. However, our finding should be interpreted with some limitations. First, the participants of the OAI are at high risk or they already had knee OA. Thus, our results are not generalizable to the general population. Second, the observational nature of our findings can introduce another bias in our results, although we tried to correct this limitation using analyses adjusted for potential confounders and for the propensity-score. Third, most of the people taking statins, reported an use between 1 month and 1 year and, probably, this is a too short time for detecting a clinical effect. Fourth, given that the sample size for analyses with ROA as the outcome had a small sample size, we cannot discard the possibility that the statistical non-significance observed was due to lack of statistical power. Finally, the record of medications is self-reported (although confirmed by a trained interview) and the data regarding the duration of use can be subject to recall bias.
In conclusion, our data suggest that, overall, any statin use was not associated with a lower risk of pain worsening, radiographic and symptomatic knee OA due to knee OA in this large cohort of North American people. However, people using statins for more than 5 years and those using atorvastatin reported beneficial effects on pain worsening, whilst people taking rosuvastatin reported an increased risk for pain worsening. Therefore, future RCTs are needed to confirm/refute our observational findings.
Significance and Innovations.
The effect of statins on knee osteoarthritis outcomes are still limited.
In our study, we found that statins were not associated with a reduced risk of future pain in people with/at risk of knee osteoarthritis
People using statins for over five years and those using atorvastatin reported a significant lower risk of future pain due to knee osteoarthritis.
No effect was found for incident symptomatic knee osteoarthritis or for radiographic forms of knee osteoarthritis.
Acknowledgements
Sponsor’s Role: none.
Founding source: The OAI is a public-private partnership comprised of five contracts (N01-AR-2-2258; N01-AR-2-2259; N01-AR-2-2260; N01-AR-2-2261; N01-AR-2-2262) funded by the National Institutes of Health, a branch of the Department of Health and Human Services, and conducted by the OAI Study Investigators. Private funding partners include Merck Research Laboratories; Novartis Pharmaceuticals Corporation, GlaxoSmithKline; and Pfizer, Inc. Private sector funding for the OAI is managed by the Foundation for the National Institutes of Health. This manuscript was prepared using an OAI public use data set and does not necessarily reflect the opinions or views of the OAI investigators, the NIH, or the private funding partners.
Footnotes
Author Contributions: Study concept and design: Veronese, Reginster; analysis and interpretation of data: Koyanagi, Stubbs, Cooper; preparation of manuscript: Veronese, Guglielmi, Maggi; critical revision: Al-Daghri, Rizzoli, Reginster, Maggi. All the authors approved the final version.
Declarations of interest: Dr. Rizzoli reports personal fees from Radius Health, Sandoz, Labatec-Effryx, Mylan; Dr. Reginster reports grants and personal fees from IBSA-GENEVRIER, grants and personal fees from MYLAN, grants and personal fees from RADIUS HEALTH, personal fees from PIERRE FABRE, grants and personal fees from CNIEL, personal fees from DAIRY RESEARCH COUNCIL (DRC); prof. Punzi Punzi received consultancy and speaker fees from BMS, Fidia, Grunenthal, Menarini, MSD, Pfizer; Professor Cooper reports personal fees from Alliance for Better Bone Health, Amgen, Eli Lilly, GSK, Medtronic, Merck, Novartis, Pfizer, Roche, Servier, Takeda and UCB. These authors reported that these grants and personal fees are outside the submitted work. The other authors have nothing to disclose.
References
- 1.Davignon J. Beneficial Cardiovascular Pleiotropic Effects of Statins. Circulation. 2004;109(23 suppl 1):III–39. doi: 10.1161/01.CIR.0000131517.20177.5a. [DOI] [PubMed] [Google Scholar]
- 2.Afilalo J, Duque G, Steele R, Jukema JW, de Craen AJM, Eisenberg MJ. Statins for Secondary Prevention in Elderly Patients. Journal of the American College of Cardiology. 2008;51(1):37–45. doi: 10.1016/j.jacc.2007.06.063. [DOI] [PubMed] [Google Scholar]
- 3.Mills EJ, Rachlis B, Wu P, Devereaux PJ, Arora P, Perri D. Primary prevention of cardiovascular mortality and events with statin treatments: a network meta-analysis involving more than 65,000 patients. Journal of the American College of Cardiology. 2008;52(22):1769–81. doi: 10.1016/j.jacc.2008.08.039. [DOI] [PubMed] [Google Scholar]
- 4.Berenbaum F. Osteoarthritis as an inflammatory disease (osteoarthritis is not osteoarthrosis!) 2013:16–21. doi: 10.1016/j.joca.2012.11.012. [DOI] [PubMed] [Google Scholar]
- 5.Veronese N, Shivappa N, Stubbs B, Smith T, Hebert JR, Cooper C, et al. The relationship between the dietary inflammatory index and prevalence of radiographic symptomatic osteoarthritis: data from the Osteoarthritis Initiative. European journal of nutrition. 2017 doi: 10.1007/s00394-017-1589-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Johnson VL, Hunter DJ. The epidemiology of osteoarthritis. Best Practice and Research: Clinical Rheumatology. 2014;28(1):5–15. doi: 10.1016/j.berh.2014.01.004. [DOI] [PubMed] [Google Scholar]
- 7.Conaghan PG. The effects of statins on osteoarthritis structural progression: another glimpse of the Holy Grail? Annals of the rheumatic diseases. 2012;71(5):633. doi: 10.1136/annrheumdis-2011-201135. [DOI] [PubMed] [Google Scholar]
- 8.Scott D, Blizzard L, Fell J, Jones G. Statin therapy, muscle function and falls risk in community-dwelling older adults. QJM: An International Journal of Medicine. 2009;102(9):625–33. doi: 10.1093/qjmed/hcp093. [DOI] [PubMed] [Google Scholar]
- 9.Clockaerts S, Van Osch GJ, Bastiaansen-Jenniskens YM, Verhaar JA, Van Glabbeek F, Van Meurs JB, et al. Statin use is associated with reduced incidence and progression of knee osteoarthritis in the Rotterdam study. Annals of the rheumatic diseases. 2012;71(5):642–7. doi: 10.1136/annrheumdis-2011-200092. [DOI] [PubMed] [Google Scholar]
- 10.Beattie MS, Lane NE, Hung YY, Nevitt MC. Association of statin use and development and progression of hip osteoarthritis in elderly women. The Journal of rheumatology. 2005;32(1):106–10. [PubMed] [Google Scholar]
- 11.Neogi T. The Epidemiology and Impact of Pain in Osteoarthritis. Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society. 2013;21(9):1145–53. doi: 10.1016/j.joca.2013.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Haukoos JS, Lewis RJ. The Propensity Score. Jama. 2015;314(15):1637–8. doi: 10.1001/jama.2015.13480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eby GA, Eby KL. Rapid recovery from major depression using magnesium treatment. Medical Hypotheses. 2006;67(2):362–70. doi: 10.1016/j.mehy.2006.01.047. [DOI] [PubMed] [Google Scholar]
- 14.Angst F, Aeschlimann A, Michel BA, Stucki G. Minimal clinically important rehabilitation effects in patients with osteoarthritis of the lower extremities. The Journal of rheumatology. 2002;29(1):131–8. [PubMed] [Google Scholar]
- 15.Dai Z, Niu J, Zhang Y, Jacques P, Felson DT. Dietary intake of fibre and risk of knee osteoarthritis in two US prospective cohorts. Annals of the rheumatic diseases. 2017;76(8):1411–9. doi: 10.1136/annrheumdis-2016-210810. [DOI] [PubMed] [Google Scholar]
- 16.Allen KD, Golightly YM. Epidemiology of osteoarthritis: state of the evidence. Current opinion in rheumatology. 2015;27(3):276–83. doi: 10.1097/BOR.0000000000000161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lewinsohn PM, Seeley JR, Roberts RE, Allen NB. Center for Epidemiologic Studies Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychology and aging. 1997;12(2):277–87. doi: 10.1037//0882-7974.12.2.277. [DOI] [PubMed] [Google Scholar]
- 18.Washburn RA, McAuley E, Katula J, Mihalko SL, Boileau RA. The physical activity scale for the elderly (PASE): evidence for validity. Journal of clinical epidemiology. 1999;52(7):643–51. doi: 10.1016/s0895-4356(99)00049-9. [DOI] [PubMed] [Google Scholar]
- 19.Katz JN, Chang LC, Sangha O, Fossel AH, Bates DW. Can comorbidity be measured by questionnaire rather than medical record review? Medical care. 1996;34(1):73–84. doi: 10.1097/00005650-199601000-00006. [DOI] [PubMed] [Google Scholar]
- 20.Miles J. Tolerance and variance inflation factor. Wiley StatsRef: Statistics Reference Online. 2009 [Google Scholar]
- 21.Parker BA, Capizzi JA, Grimaldi AS, Clarkson PM, Cole SM, Keadle J, et al. The effect of statins on skeletal muscle function. Circulation. 2012 doi: 10.1161/CIRCULATIONAHA.112.136101. CIRCULATIONAHA-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McCarey DW, McInnes IB, Madhok R, Hampson R, Scherbakov O, Ford I, et al. Trial of Atorvastatin in Rheumatoid Arthritis (TARA): double-blind, randomised placebo-controlled trial. Lancet (London, England) 2004;363(9426):2015–21. doi: 10.1016/S0140-6736(04)16449-0. [DOI] [PubMed] [Google Scholar]
- 23.Okamoto H, Koizumi K, Kamitsuji S, Inoue E, Hara M, Tomatsu T, et al. Beneficial action of statins in patients with rheumatoid arthritis in a large observational cohort. The Journal of rheumatology. 2007;34(5):964–8. [PubMed] [Google Scholar]
- 24.Kadam UT, Blagojevic M, Belcher J. Statin Use and Clinical Osteoarthritis in the General Population: A Longitudinal Study. Journal of general internal medicine. 2013;28(7):943–9. doi: 10.1007/s11606-013-2382-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Martel-Pelletier J, Boileau C, Pelletier JP, Roughley PJ. Cartilage in normal and osteoarthritis conditions. 2008:351–84. doi: 10.1016/j.berh.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 26.Findlay DM. Vascular pathology and osteoarthritis. Rheumatology (Oxford, England) 2007;46(12):1763–8. doi: 10.1093/rheumatology/kem191. [DOI] [PubMed] [Google Scholar]
- 27.Bulbulia R, Armitage J. Does the benefit from statin therapy extend beyond 5 years? Current atherosclerosis reports. 2013;15(2):297. doi: 10.1007/s11883-012-0297-1. [DOI] [PubMed] [Google Scholar]
- 28.Chong PH, Seeger JD, Franklin C. Clinically relevant differences between the statins: implications for therapeutic selection. The American journal of medicine. 2001;111(5):390–400. doi: 10.1016/s0002-9343(01)00870-1. [DOI] [PubMed] [Google Scholar]
- 29.Barter MJ, Hui W, Lakey RL, Catterall JB, Cawston TE, Young DA. Lipophilic statins prevent matrix metalloproteinase-mediated cartilage collagen breakdown by inhibiting protein geranylgeranylation. Annals of the rheumatic diseases. 2010;69(12):2189–98. doi: 10.1136/ard.2010.129197. [DOI] [PubMed] [Google Scholar]