Figure 1.
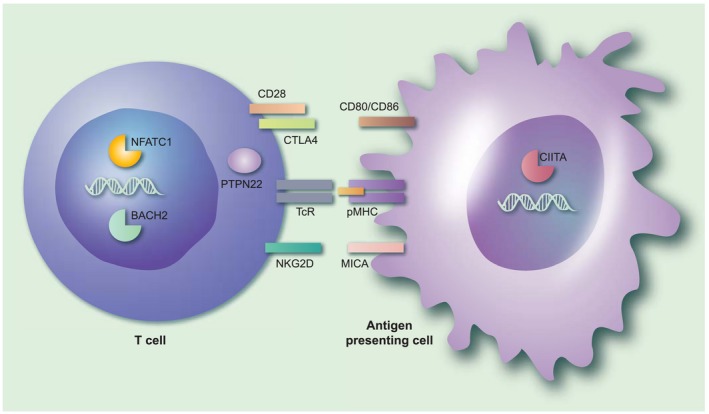
The immunological context of genetic susceptibility factors for autoimmune Addison’s disease that may interact with infectious agents. The figure gives an overview of the immunological processes implicated by the genetic susceptibility factors associated with autoimmune Addison’s disease (AAD). Note that both the products encoded by the risk genes themselves (denoted in bold type below) and their interaction partners are shown in the figure. Professional antigen‐presenting cells, such as dendritic cells or activated B cells, present antigenic peptides (from self or from microorganisms) on their major histocompatibility complex/human leucocyte antigen (MHC/HLA) molecules (pMHC in the figure) that may be recognized by T cells through their T cell receptor (TCR). An additional co‐stimulatory signal, usually mediated by CD80/CD86, is required for T cell activation. On the T cell, CD28 acts as a positive co‐stimulator, while cytotoxic T lymphocyte antigen‐4 (CTLA‐4) transmits inhibitory (negative) signals upon CD80/CD86 ligation. Polymorphisms in CTLA‐4 that may predispose to AAD may also lead to excessive immune responses in response to certain viruses. Protein tyrosine phosphatase, non‐receptor type 22 (PTPN22) serves critical roles in the regulation of T cell activation signalling events downstream of the TCR. A specific genetic variant of PTPN22 may predispose to the activation of self‐specific T cells, but also may lead to suboptimal immune responses against influenza. MHC class I polypeptide‐related sequence A (MICA), a ligand for the co‐stimulatory molecule natural killer group 2 member D (NKGD2) on CD8+ T cells, is up‐regulated by viral infection. Genetic variants in the transcription factors broad complex‐tramtrack‐bric a brac and cap’n’collar homology 2 (BACH2), nuclear factor of activated T cells (NFATC1) and class II major histocompatibility complex transactivator (CIITA) have all been associated with AAD. Mutations in BACH2 may give rise to an immunodeficiency syndrome with recurrent viral pulmonary infections; NFATC1 plays a role in the process of T cell exhaustion during viral infections, while CIITA is a well‐known target for immune evasive strategies for several viruses. [Colour figure can be viewed at wileyonlinelibrary.com]
