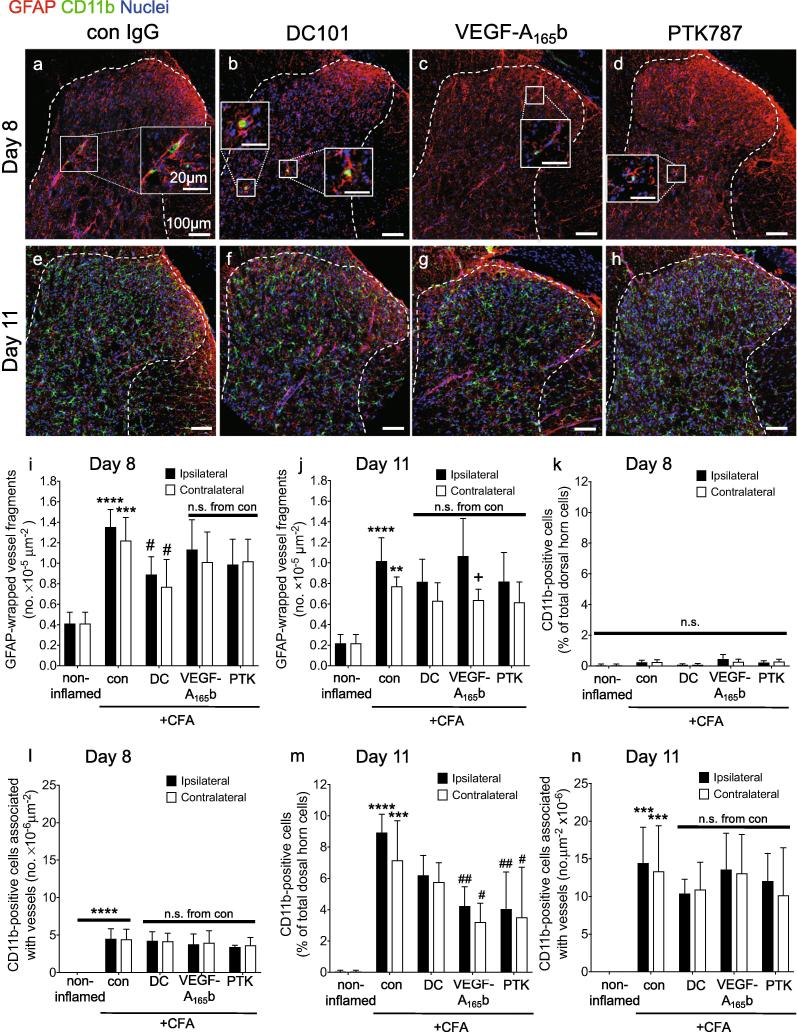
Fig. 4.
The effect of anti-VEGFR2 agents on astrocytic and microglial reactivity to articular inflammation. Intra-articular CFA caused a significant increase in the number of GFAP+ end-feet-wrapped vessel fragments in the ipsilateral dorsal horn on both (a) day eight and (e) day 11. Treatment with DC101 (b,f), but not VEGF-A165b (c,g) nor PTK787 (d,h) significantly reduced the number of ipsilateral and contralateral GFAP+ end-feet-wrapped vessel fragments on day eight (i), but not on day 11 (j). Intra-articular CFA caused a significant increase in microvessel-associated CD11b+ cells (ipsi- and contralateral) on day eight (k) and day 11 (l) with no difference observed between the CFA groups at both time points. On day eight there was no significant difference in the number of CD11b+ cells in the dorsal horn parenchyma compared to control (m), whereas on day 11 there was a significant increase in CD11b+ cells in the dorsal horn parenchyma compared to non-inflamed control animals. All three anti-VEGF treatments reduced this number although only VEGF-A165b (ipsi & contalateral) and PTK787 (ipsilateral) reached statistical significance (n). The only significant difference between respective ipsi- and contralateral effects was observed in VEGF-A165b group on the number of GFAP-wrapped vessels at day 11 (j). Three statistical analyses were performed: 2-way analysis of variance + Dunnett’s multiple comparisons test: control vs. non-inflamed *p < 0.5, **p < 0.01, ***p < 0.001, ****p < 0.0001; anti-VEGFR2 agent vs. control (ipsi or contra): #p < 0.5, ##p < 0.01, ###p < 0.001, ####p < 0.0001 and ipsi vs. contra of respective group +p < 0.5. Day eight: n = 4; day 11: n = 4–5. Data displayed as mean ± SD.