Abstract
Background:
Spinal cord decompression after cervical spinal cord injury (SCI) is the standard of care. However, there is a lack of consensus regarding the optimal management of these injuries, including the role of traction and timing of surgery. Here, we report the safety/efficacy of ventral surgery without preoperative traction for intraoperative fracture reduction following acute cervical SCI.
Methods:
We prospectively collected a series of patients who sustained acute traumatic subaxial cervical (C3–7) spine fractures between 2004 and 2016. Patients underwent anterior cervical decompression and fusion within 24 h of injury without the utilization of preoperative traction.
Results:
Thirty-six patients (27 male, 9 female), averaging 35 years of age, sustained 25 motor-vehicle accidents, 4 sports-related injuries, and 7 falls. Fracture dislocations were seen in 26 patients, whereas burst fractures were seen in 10. The majority of injuries occurred at the C4–5 (13 patients) and C5–6 (13 patients) levels. Complete SCI occurred in 10 patients, and incomplete SCI in 26 patients. All patients underwent anterior surgery only; 16 required vertebrectomy in addition to anterior cervical discectomy and fusion. Intraoperative reduction was achieved in all patients using a Cobb elevator or distraction pins without the use of preanesthesia traction. There were no intraoperative complications. Postoperatively, there were one postoperative hematoma, two wound/hardware revisions, one subsequent posterior fusion, and one reoperation anteriorly after screw pullout. The average hospital length of stay was 10.6 days (range 1–39).
Conclusion:
Early direct surgical stabilization/fusion for acute SCI because of subaxial cervical spine fractures is both safe and effective in selected cases when performed anteriorly without preoperative traction in select cases.
Keywords: Cervical, fracture, spinal cord injury, surgery, trauma
INTRODUCTION
There are approximately 200,000 people in America with spinal cord injuries (SCIs), and there are around 10,000 new cases each year.[22,26] One-third of SCIs involve the cervical vertebrae.[26] Spinal cord decompression with reduction of the fracture has become the standard of care, but a universally accepted protocol does not exist.[11] Debate still exists regarding use of preoperative traction, optimal surgical approach, and ideal timing for surgical reduction of subaxial cervical vertebral fractures for decompression of the spinal cord.[9,13,21]
Some studies have shown that surgery within 24 or 72 h results in better neurological outcomes than those treated after longer delays.[7,20] Here, we examined the outcomes of early (<24 h) anterior cervical discectomy and fusion (ACDF) for subaxial cervical spine fractures without preoperative traction.
MATERIALS AND METHODS
Study protocol
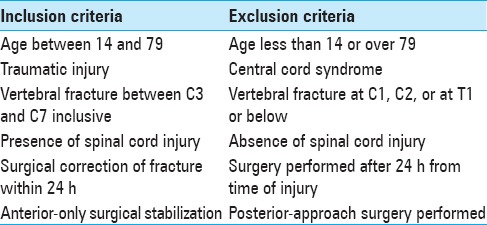
This study was a retrospective analysis of a prospectively collected database of patients with acute vertebral fractures resulting in cervical SCIs at our institution from 2004 and 2016. For a full list of inclusion and exclusion criteria, see Table 1. Ultimately, 36 patients qualified for inclusion in the study. Upon admission, all patients underwent a history and physical examination. Plain films or CT was used for the initial diagnosis, with MRI obtained as needed. The American Spinal Injury Association impairment scale was used to grade neurological status. Fracture patterns were described using the AO classification system. Surgical indications were determined based on individual patient factors, neurological status, and spinal instability.
Table 1.
Inclusion and exclusion criteria
Operative procedure
All 36 patients underwent surgery within 24 h of sustaining the injury, with 12 of those undergoing surgery within 8 h. Cervical traction using Gardner–Wells tongs was applied after the induction of general anesthesia and fluoroscopy was used to evaluate alignment following placement of traction. Metzenbaum scissor dissection was used through the prevertebral fascia. Intraoperative fluoroscopy was used to confirm the level of injury. Disk and ligament was removed. If the deformity was not reduced at this point (by traction, anesthesia, and discectomy), a Cobb elevator was placed in the disk space and maneuvered until the fracture reduced. Once decompression was obtained, the cartilaginous end plates were removed with a high-speed air drill and graft spacers were used. An anterior cervical plate was then locked into place and confirmed using intraoperative X-ray.
Postoperative care
Patients were mobilized as soon as possible after surgery, dependent upon their neurologic exam and concomitant injuries. Radiographs were obtained for each patient prior to discharge. Patients were enrolled with physical therapy and occupational therapy as needed. Follow-ups occurred in an outpatient spine clinic 4–6 weeks after surgery where initial follow-up X-rays were performed. Further outpatient imaging was obtained as needed. Patients filled out follow-up medical history intake forms ranking their symptoms, pain, and mood at each appointment.
RESULTS
Patient demographics
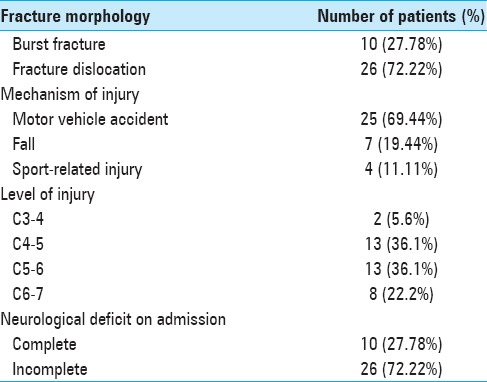
The hospital course of the 36 patients (27 male, 9 female), averaging 35 years of age, was reviewed. See Table 2 for information regarding fracture morphology, type and level of spinal cord injury, and mechanism of injury.
Table 2.
Patient population (n=36)
Surgical results and complications
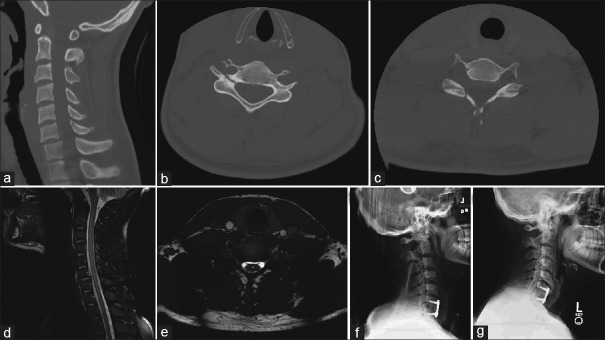
After physician evaluation, all 36 patients underwent surgery within 24 h of injury. Twelve patients had surgery within 8 h (eight motor-vehicle accidents, one sports-related injury, three falls). Of these 12 patients, 6 had complete and 6 had incomplete SCIs. Ten were male, two were female. All 36 patients underwent intraoperative reduction with subsequent ACDF. Figure 1 presents a patient case scenario.
Figure 1.
A 20-year-old male after motor vehicle accident with weakness of elbow and wrist flexion and extension along with reduced grip strength. (a–c) Preoperative CT scan demonstrating traumatic spondylolisthesis of C6–7 with associated fractures of C5 pedicle and C6 lamina. (d, e) MRI C-spine with no cord compression but an associated small syrinx. (f) Immediate postoperative X-ray demonstrating reduction of the anterolisthesis and appropriate placement of C6–7 hardware. (g) Lateral cervical X-ray demonstrated C6–7 fusion at 55 months following anterior cervical fusion
No patients suffered intraoperative neurological or vascular complications. Five patients had postoperative complications: two hardware failures (5.6%), two infections (5.6%), and one neck hematoma (2.8%). One patient required reoperation via anterior approach after kyphotic deformity 2 months after initial surgery because of noncompliance wearing their postoperative cervical collar. A second patient had reoperation 3 days after surgery to revise a C7 screw that pulled out. One patient developed a draining neck sinus infected with Methicillin-Susceptible Staphylococcus aureus (MSSA) 4 years after initial surgery. This patient underwent removal of anterior hardware and posterior fusion without further issue. Another patient had a wound revision 12 days after surgery for purulent drainage. One patient had a neck hematoma after a heparin drip was initiated for a postoperative Non-ST segment Elevation Myocardial Infarction (NSTEMI) requiring evacuation of clot at bedside. None of these complications affected the neurological status of the patients.
Length of stay and outcomes
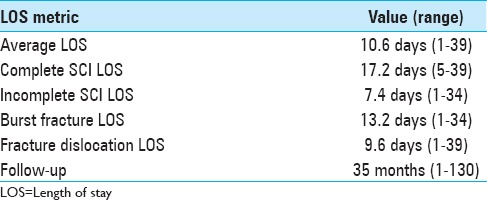
Follow-up data ranged from 1 to 130 (average 35) months. See Table 3 for data regarding hospital length of stay and follow-up. Twenty-five patients (69.4%) demonstrated improvement in their neurological function.
Table 3.
Hospital LOS and follow-up
DISCUSSION
In the current study, the average age and male predominance are similar to other published series.[3,10,14,19] It has been shown that early in a spinal cord injury, the duration of spinal cord compression is directly related to the propagation of secondary injuries.[1,7] Some surgeons still believe that there is equal or greater improvement in patients who undergo delayed surgery (>72 h after injury);[6,27] yet, despite this, Fehlings et al.[5] in a systematic review and prospective survey study found that depending on the clinical scenario, between 80.0% and 96.4% of spinal surgeons generally prefer decompression an acute cervical SCI within 24 h, with a majority wanting to decompress within 6 h. This is consistent with the idea that the benefits of decompression are greater when the duration of the spinal cord compression is short, decreasing secondary neurologic deterioration.[1,8] We believe that although preoperative traction is an option, it comes with the risk of delaying surgery and therefore potentially causing neurologic harm. To reduce duration between the trauma and ultimate surgical therapy, in this study, preoperative traction was not performed. In addition, some fractures will not reduce with traction alone, and traction in these cases may delay definitive reduction. The incidence of neurologic deterioration after SCI is 1.8–10%, which can be related to either halo vest or traction immobilization, and loss of neurologic function due to spinal cord distraction, ligamentous rupture, or disk protrusion may occur.[2,4,12,17,24,25] Conversely, once a patient presents to clinical attention and an unstable cervical fracture is identified with a neurological exam consistent with a spinal cord injury, they can immediately be taken to the operating room to undergo definitive treatment via anterior cervical approach.
Although several studies exist on cervical fractures, spinal cord injury, and early surgery,[15,16,18,23] our study focuses on patients who meet all four criteria: spinal cord injury, subaxial vertebral body fracture, anterior-only surgical approach, and no use of preoperative traction. Our study is novel in that it proposes rapid anterior surgical correction of spinal instability in the case of spinal cord injury. We believe the minimal dissection required for anterior approach surgery and proven ability to successfully and definitively reduce the deformity, remove the herniated disk, and decompress the neural elements allows for early mobilization and shorter hospitalizations in this subset of patients. In our study, no patients experienced deterioration in neurological status after ACDF. Patients with incomplete SCI recovered quicker than those with complete SCI, consistent with data from previous studies.[5] It was also noted in this study that patients who experienced a fracture dislocation had shorter hospital length of stay than patients who suffered a burst fracture.
CONCLUSIONS
Early surgical treatment of the subaxial cervical spine in cases of acute SCI through ACDF is both safe and technically feasible. Although traction may help reduce the fracture, emphasis should be placed on early surgical decompression for definitive treatment.
Prior presentation
Portions of this work were presented as a digital poster at the 2018 AANS Scientific Meeting in New Orleans, LA, and at the 2018 CNS Scientific Meeting in Houston, TX.
Financial support and sponsorship
This work received no source of funding and was not supported in any way by grants or industry-affiliated products/services.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Contributor Information
Domenico A. Gattozzi, Email: dgattozzi@kumc.edu.
Bailey R. Yekzaman, Email: byekzaman@kumc.edu.
Megan M. Jack, Email: mjack@kumc.edu.
Michael J. O'Bryan, Email: mjobryan@gmail.com.
Paul M. Arnold, Email: parnold@kumc.edu.
REFERENCES
- 1.Carlson GD, Gorden CD, Oliff HS, Pillai JJ, LaManna JC. Sustained spinal cord compression: Part I: Time-dependent effect on long-term pathophysiology. J Bone Joint Surg Am. 2003;85-A:86–94. [PubMed] [Google Scholar]
- 2.Colterjohn NR, Bednar DA. Identifiable risk factors for secondary neurologic deterioration in the cervical spine-injured patient. Spine (Phila Pa 1976) 1995;20:2293–7. doi: 10.1097/00007632-199511000-00006. [DOI] [PubMed] [Google Scholar]
- 3.DeVivo MJ, Rutt RD, Black KJ, Go BK, Stover SL. Trends in spinal cord injury demographics and treatment outcomes between 1973 and 1986. Arch Phys Med Rehabil. 1992;73:424–30. [PubMed] [Google Scholar]
- 4.Farmer J, Vaccaro A, Albert TJ, Malone S, Balderston RA, Cotler JM. Neurologic deterioration after cervical spinal cord injury. J Spinal Disord. 1998;11:192–6. [PubMed] [Google Scholar]
- 5.Fehlings MG, Rabin D, Sears W, Cadotte DW, Aarabi B. Current practice in the timing of surgical intervention in spinal cord injury. Spine (Phila Pa 1976) 2010;35(21 Suppl):S166–73. doi: 10.1097/BRS.0b013e3181f386f6. [DOI] [PubMed] [Google Scholar]
- 6.Fehlings MG, Tetreault LA, Wilson JR, Aarabi B, Anderson P, Arnold PM, et al. A clinical practice guideline for the management of patients with acute spinal cord injury and central cord syndrome: Recommendations on the timing (≤24 hours versus>24 hours) of decompressive surgery. Global Spine J. 2017;7(3 Suppl):195S–202S. doi: 10.1177/2192568217706367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fehlings MG, Vaccaro A, Wilson JR, Singh A, D WC, Harrop JS, et al. Early versus delayed decompression for traumatic cervical spinal cord injury: Results of the Surgical Timing in Acute Spinal Cord Injury Study (STASCIS) PLoS One. 2012;7:e32037. doi: 10.1371/journal.pone.0032037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fehlings MG, Wilson JR. Timing of surgical intervention in spinal trauma: What does the evidence indicate? Spine (Phila Pa 1976) 2010;35(21 Suppl):S159–60. doi: 10.1097/BRS.0b013e3181f330f4. [DOI] [PubMed] [Google Scholar]
- 9.Feuchtbaum E, Buchowski J, Zebala L. Subaxial cervical spine trauma. Curr Rev Musculoskelet Med. 2016;9:496–504. doi: 10.1007/s12178-016-9377-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Frankel HL, Coll JR, Charlifue SW, Whiteneck GG, Gardner BP, Jamous MA, et al. Long-term survival in spinal cord injury: A fifty year investigation. Spinal Cord. 1998;36:266–74. doi: 10.1038/sj.sc.3100638. [DOI] [PubMed] [Google Scholar]
- 11.Gelb DE, Aarabi B, Dhall SS, Hurlbert RJ, Rozzelle CJ, Ryken TC, et al. Treatment of subaxial cervical spinal injuries. Neurosurgery. 2013;72(Suppl 2):187–94. doi: 10.1227/NEU.0b013e318276f637. [DOI] [PubMed] [Google Scholar]
- 12.Harrop JS, Sharan AD, Vaccaro AR, Przybylski GJ. The cause of neurologic deterioration after acute cervical spinal cord injury. Spine (Phila Pa 1976) 2001;26:340–6. doi: 10.1097/00007632-200102150-00008. [DOI] [PubMed] [Google Scholar]
- 13.Koller H, Reynolds J, Zenner J, Forstner R, Hempfing A, Maislinger I, et al. Mid- to long-term outcome of instrumented anterior cervical fusion for subaxial injuries. Eur Spine J. 2009;18:630–53. doi: 10.1007/s00586-008-0879-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Levi L, Wolf A, Rigamonti D, Ragheb J, Mirvis S, Robinson WL. Anterior decompression in cervical spine trauma: Does the timing of surgery affect the outcome? Neurosurgery. 1991;29:216–22. [PubMed] [Google Scholar]
- 15.Li H, Huang Y, Cheng C, Lin Z, Wu D. Comparison of the technique of anterior cervical distraction and screw elevating-pulling reduction and conventional anterior cervical reduction technique for traumatic cervical spine fractures and dislocations. Int J Surg. 2017;40:45–51. doi: 10.1016/j.ijsu.2017.02.057. [DOI] [PubMed] [Google Scholar]
- 16.Li H, Yong Z, Chen Z, Huang Y, Lin Z, Wu D. Anterior cervical distraction and screw elevating-pulling reduction for traumatic cervical spine fractures and dislocations: A retrospective analysis of 86 cases. Medicine (Baltimore) 2017;96:e7287. doi: 10.1097/MD.0000000000007287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mahale YJ, Silver JR, Henderson NJ. Neurological complications of the reduction of cervical spine dislocations. J Bone Joint Surg Br. 1993;75:403–9. doi: 10.1302/0301-620X.75B3.8496208. [DOI] [PubMed] [Google Scholar]
- 18.Mattiassich G, Gollwitzer M, Gaderer F, Blocher M, Osti M, Lill M, et al. Functional outcomes in very early (<5 hours) and early (5-24 hours) surgical decompression in traumatic cervical spinal cord injury. Analysis of Neurological Improvement from the Austrian Spinal Cord Injury Study (ASCIS) J Neurotrauma. 2017;34:3362–71. doi: 10.1089/neu.2017.5132. [DOI] [PubMed] [Google Scholar]
- 19.McKinley WO, Huang ME, Tewksbury MA. Neoplastic vs.traumatic spinal cord injury: An inpatient rehabilitation comparison. Am J Phys Med Rehabil. 2000;79:138–44. doi: 10.1097/00002060-200003000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Mirza SK, Krengel WF, 3rd, Chapman JR, Anderson PA, Bailey JC, Grady MS, et al. Early versus delayed surgery for acute cervical spinal cord injury. Clin Orthop Relat Res. 1999:104–14. doi: 10.1097/00003086-199902000-00011. [DOI] [PubMed] [Google Scholar]
- 21.Park JH, Roh SW, Rhim SC. A single-stage posterior approach with open reduction and pedicle screw fixation in subaxial cervical facet dislocations. J Neurosurg Spine. 2015;23:35–41. doi: 10.3171/2014.11.SPINE14805. [DOI] [PubMed] [Google Scholar]
- 22.Passias PG, Poorman GW, Segreto FA, Jalai CM, Horn SR, Bortz CA, et al. Traumatic fractures of the cervical spine: Analysis of changes in incidence, cause, concurrent injuries, and complications among 488,262 patients from 2005 to 2013. World Neurosurg. 2018;110:e427–37. doi: 10.1016/j.wneu.2017.11.011. [DOI] [PubMed] [Google Scholar]
- 23.Reindl R, Ouellet J, Harvey EJ, Berry G, Arlet V. Anterior reduction for cervical spine dislocation. Spine (Phila Pa 1976) 2006;31:648–52. doi: 10.1097/01.brs.0000202811.03476.a0. [DOI] [PubMed] [Google Scholar]
- 24.Robertson PA, Ryan MD. Neurological deterioration after reduction of cervical subluxation. Mechanical compression by disc tissue. J Bone Joint Surg Br. 1992;74:224–7. doi: 10.1302/0301-620X.74B2.1544957. [DOI] [PubMed] [Google Scholar]
- 25.Vaccaro AR, Falatyn SP, Flanders AE, Balderston RA, Northrup BE, Cotler JM. Magnetic resonance evaluation of the intervertebral disc, spinal ligaments, and spinal cord before and after closed traction reduction of cervical spine dislocations. Spine (Phila Pa 1976) 1999;24:1210–7. doi: 10.1097/00007632-199906150-00007. [DOI] [PubMed] [Google Scholar]
- 26.Wilson JR, Grossman RG, Frankowski RF, Kiss A, Davis AM, Kulkarni AV, et al. A clinical prediction model for long-term functional outcome after traumatic spinal cord injury based on acute clinical and imaging factors. J Neurotrauma. 2012;29:2263–71. doi: 10.1089/neu.2012.2417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wilson JR, Tetreault LA, Kwon BK, Arnold PM, Mroz TE, Shaffrey C, et al. Timing of decompression in patients with acute spinal cord injury: A systematic review. Global Spine J. 2017;7(3 Suppl):95S–115S. doi: 10.1177/2192568217701716. [DOI] [PMC free article] [PubMed] [Google Scholar]