Abstract
Despite high rates of housing-cost burden in the United States, little is known regarding its impact on childhood obesity. In this article, we determine whether low-income 2–5-year-olds living in housing-cost burdened households are more likely to be obese and examine the potential moderators and behavioral and psychosocial mediators of this relationship. We used data from a triennial survey (2011, 2014) of a random sample of Los Angeles County participants of the Special Supplemental Nutrition Program for Women, Infants and Children (n = 2307). Logistic regression was used to examine the association between child's obesity status (Body Mass Index for age and sex ≥ 95th percentile) and severe housing-cost burden (finding it very difficult to pay for housing). Mother's depressive symptoms and child's diet and screen time were tested for mediation. We found that 16% of children lived in severe housing-cost burdened households. Severe housing-cost burden was associated with an increase in the odds of childhood obesity [aOR (95%CI) = 1.33 (1.00, 1.78)] and household size moderated this relationship. Child's diet and screen time and mother's depressive symptoms were not mediators. Given the high and vacillating rates of early childhood obesity and the increasing burden of housing costs in low-income populations, there is an urgency to better understand the role of housing-cost burden in epidemiologic investigations of early childhood obesity.
Abbreviations: SHCB, severe housing-cost burden; LAC, Los Angeles County; WIC, the Special Supplemental Nutrition Program for Women, Infants and Children
Keywords: Pediatric obesity, Housing, Poverty, WIC
Highlights
-
•
Children in severe housing-cost burdened households had more chronic stressors.
-
•
Severe housing-cost burden was associated with greater odds of childhood obesity.
-
•
Child's behavior and mother's mental well-being were not mediators of the relationship.
1. Introduction
The cost of housing has become increasingly expensive in the United States, particularly in metropolitan areas such as New York, San Francisco, and Los Angeles (Joint Center for Housing Studies of Harvard University, 2018). However, household incomes, especially among low-income households, have not kept apace (Joint Center for Housing Studies of Harvard University, 2018). The inability to keep up with rising housing costs has increased housing-cost burden in the United States (Joint Center for Housing Studies of Harvard University, 2018). This difficulty to pay for housing forces many households to make cost-cutting tradeoffs in order to have shelter (Joint Center for Housing Studies of Harvard University, 2018). Because housing is essential, housing-cost burden is also a risk factor for various health outcomes. While it has begun to be explored in regards to adult and child health (Harkness and Newman, 2005; Ma et al., 2008; Pollack et al., 2010; Nicholas, 2017; Bolívar Muñoz et al., 2016; Downing, 2016), little is known about the impact of housing-cost burden on obesity among children, especially among low-income preschool-aged children who are at high risk of obesity.
Given the dearth of research, we drew on the Family Stress Model of Economic Hardship, the Risky Families Model and biological theory describing the effects of chronic stress on energy metabolism, to inform how housing-cost burden might influence childhood obesity (Downing, 2016; Conger et al., 2000; Repetti et al., 2002; Miller et al., 2017). The two main mechanisms posited are through child's behaviors and parent's chronic psychosocial stress, both resulting from insufficient financial resources after housing costs have been paid (see Supplemental Fig. 1 for conceptual framework). Difficulty paying for housing may influence the proximal risk factors of obesity, namely diet and physical activity. Housing-cost burdened households are more likely to be in disadvantaged neighborhoods (Joint Center for Housing Studies of Harvard University, 2018) where fast food restaurants proliferate and access to affordable, healthy foods and facilities for exercise is limited (Schreier and Chen, 2013). In order to pay for housing, households are likely to cut their food-related expenses (Joint Center for Housing Studies of Harvard University, 2018; Harkness and Newman, 2005; Kirkpatrick and Tarasuk, 2007) relying more heavily on cheap, highly-caloric food (Rehm et al., 2011). While medical care and food are typically the first to be cut (Joint Center for Housing Studies of Harvard University, 2018; Kirkpatrick and Tarasuk, 2007; Feeding America et al., 2013; Williams et al., 2004), households may choose to cut other types of expenses such as utility bills, transportation, entertainment, and child care. Our tabulations from the 2013 Consumer Expenditure Survey found that while the lowest income households spend the greatest percentage on housing (40%) compared to higher-income households, the share spent on food (16%) is not affected given that they spend a smaller share on other expenses like transportation and entertainment.
Since housing is a basic need, the financial strain of not being able to meet housing costs every month can be a chronic stressor for parents, especially for low-income parents. This might cause conflict in the home and be detrimental to a parent's mental health, thereby creating a cold and neglectful home environment for the child (Davison et al., 2013) resulting in a child's insecure attachment with his/her primary caregiver (Gunnar and Quevedo, 2007). An insecure attachment can dysregulate the child's biological stress response system, thereby influencing the child's energy imbalance, and increasing the risk of developing obesity (Gunnar and Quevedo, 2007; Anderson and Whitaker, 2011; Garasky et al., 2009; Wilson and Sato, 2014). Studies have reported that young children whose mothers are chronically stressed or depressed are at greater risk of becoming obese (Lampard et al., 2014; Tate et al., 2015). Stressed parents might also be less inclined to cook for their children, relying instead on highly-caloric fast food (Parks et al., 2012), and to limit their children's screen time such as watching TV and playing computer games (Lampard et al., 2013).
Some features of the home environment may exacerbate the influence of housing-cost burden on childhood obesity while other features may buffer it. Housing-cost burdened households may cut their food expenditures so much that they become food insecure (Kirkpatrick and Tarasuk, 2011). While findings are mixed (Franklin et al., 2012) food insecurity has been found to be positively associated with early childhood obesity among WIC-participating children (Franklin et al., 2012; Metallinos-Katsaras et al., 2012) and it might be one additional financial stressor. Because homeowners have greater wealth than renters, homeownership may buffer the effect of housing-cost burden on health (Pollack et al., 2010). In order to reduce their housing costs, households may live with family members or roommates (Pilkauskas et al., 2014). The more people living together, the more likely a household is to be chaotic (Evans, 2004) and increase a child's stress (Lumeng et al., 2014). Due to rising rents and unexpected life events, families who already have a difficult time paying for housing can sometimes no longer afford their home and are forced to move. This residential instability can increase parents' stress (Theodos et al., 2018).
Based on these posited mechanisms, this study aims to 1) determine whether living in severe housing-cost burdened households is positively associated with obesity among low-income preschool-aged children living in Los Angeles County (LAC); 2) examine whether food insecurity, housing tenure, household size, and residential instability modify this relationship; and 3) evaluate the contributions of child's diet and sedentary behavior, and mother's mental well-being to this relationship.
2. Methods
2.1. Data source
Data for this study come from the 2011 and 2014 LAC WIC Survey (“WIC Survey”) (http://lawicdata.org/survey). The Special Supplemental Nutrition Program for Women, Infants and Children (WIC) is a federally-funded nutrition assistance program for low-income and nutritionally-at-risk pregnant and breastfeeding women, infants and children up to age 5. First conducted in 2005, this triennial WIC Survey was commissioned by the WIC Data Mining Project, a research partnership between the Public Health Foundation Enterprises WIC Program and First 5 LA. Each survey year, computer-assisted phone interviews are conducted on a random sample of approximately 6000 WIC participants in LAC in English and Spanish, and in Vietnamese and Cantonese in 2011.
Survey records were linked to WIC administrative data to obtain children's measured heights and weights, birthdates, household income and census tract of residence. Maintained by the WIC Data Mining Project, the administrative data are collected by the State of California WIC Program. Anthropometric measurements are obtained during clinic visits by trained WIC staff, and have high validity (Crespi et al., 2012). To characterize children's neighborhood socioeconomic conditions, survey records were linked to the 2010–2014 American Community Survey data through the child's census tract. The UCLA Institutional Review Board approved this study.
2.2. Variables
Obesity status, the outcome variable, was defined as having a BMI [weight (kg)/[height (m)]2] ≥ 95th percentile of CDC's gender- and age-specific growth reference values (Kuczmarski et al., 2002). It was calculated from height and weight measurements taken during a clinic visit that occurred after the survey but no >1.5 years from when the survey was conducted.
Change in adiposity, another outcome variable of interest, was defined as change in BMI z-score (ΔBMIz) between two time points: T1, which preceded the survey by ≤6 months, and T2 which was at least 6 months after the survey. This ensured that one time point (T1) was close enough to the survey to capture the effect of severe housing-cost burden (SHCB), while the other (T2) allowed sufficient time for a change in BMIz.
The independent variable of interest, SHCB, was determined by the response of “very difficult” to the question, “How easy or difficult is it for you to pay for housing—very difficult, somewhat difficult, somewhat easy or very easy?” Since the majority of families experienced some difficulty, a binary variable was created to measure those reporting extreme housing costs. “Very difficult” was coded as 1 and the other responses were coded as 0.
The mediating variables were child's diet, screen time and mother's depressive symptoms. Diet was assessed with two variables, one using fruit and vegetable consumption (number of daily servings of fruits and vegetables) as an indicator of healthy eating, and the other using a score derived from consumption of unhealthy foods, namely, fast food (number of times per week the child eats at a fast food restaurant), sugar-sweetened beverages (SSB; number of times per day the child drinks beverages such as sweetened milk, non-100% juice intake, and soda), and sweet foods (number of times per day the child eats foods such as sweetened cereals, fruit bars, and cookies). To create the unhealthy food score, the consumption frequencies of these three groups of unhealthy foods were dichotomized (1,0) according to recommendations for young children and the sample's distribution (Daniels and Hassink, 2015). A score of ‘1’ was assigned as follows: consumption of fast food at least once a week, of a SSB at least once a day, and of a sweet food at least once a day. Scores were summed to create an unhealthy food score with a maximum score of ‘3’ and a minimum score of ‘0’.
Screen time represents the number of hours that the child watches TV and plays video or computer games per day. Mother's depressive symptoms were determined by the two-item Patient Health Questionnaire (PHQ-2) (Kroenke et al., 2003). The responses were scored and summed. A score of 3 or higher has high sensitivity and specificity for major depression (Kroenke et al., 2003). The mediators were kept as continuous or treated as pseudo-continuous for the mediation analysis and categorized for descriptive purposes.
Analyses controlled for child's age (at T1 or time of the survey), gender, and race/ethnicity [Hispanic, Non-Hispanic (NH) white, NH black, NH Asian, and NH multiple race]. Dummy variables were created with Hispanic as the reference since the majority of children were Hispanic. Due to attrition the sample size for the mediation analysis was much smaller. We therefore used a binary ethnicity variable (Hispanic vs. not Hispanic) for the mediation analysis. We also adjusted for child's BMIz at T1 to account for child's initial weight. All of the analyses adjusted for the duration between the two time points in months. Mother's BMI was calculated from self-reported height and weight. Mother's education was the highest level of school completed or degree received. Household income was the household's percent of the federal poverty level (FPL) and was calculated by dividing household's total income by the poverty guideline for the number of people in the household. Since neighborhood socioeconomic characteristics may confound the relationship between SHCB and childhood obesity, a continuous neighborhood median household income measure was examined as a potential covariate. A binary survey year measure (2011 vs 2014) accounted for any temporal differences.
Food insecurity, housing tenure, household size, and number of moves were explored as potential moderators since they have been found to be associated with the variables of interest. A binary food insecurity measure was determined from responses to USDA's 6-item household food security scale. Responses were scored and summed. Food insecurity was determined by a score of 2 or more. Housing tenure refers to whether the household owns or rents their home, lives with relatives or lives in an ‘other’ situation. Household size is the number of people living in the household and was treated as a continuous variable and, for descriptive purposes, as a binary measure of 5 or more individuals. Similarly, number of moves was treated as both a continuous measure and binary measure of 2 or more moves during the past 3 years.
2.3. Statistical analyses
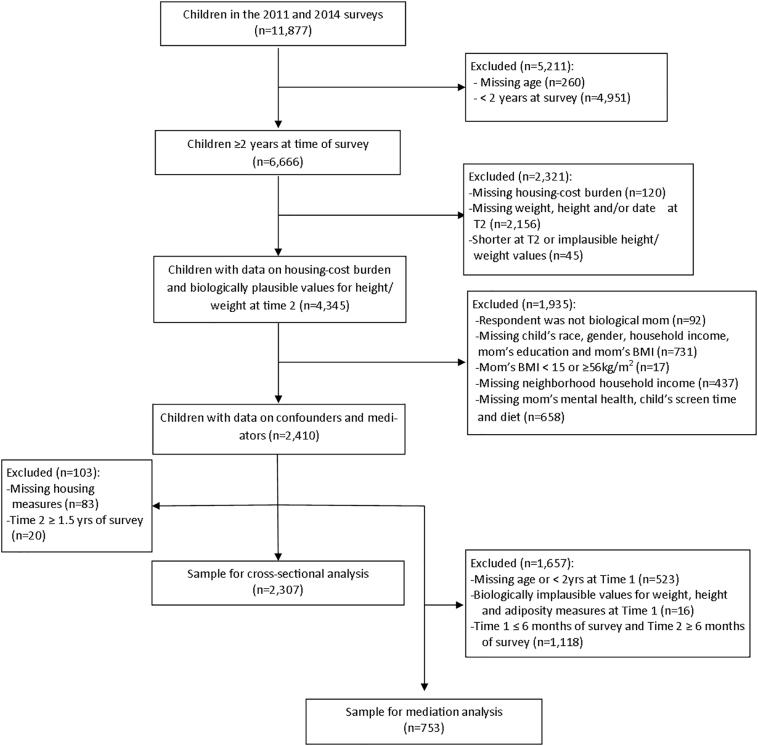
To examine the cross-sectional association of SHCB with obesity, children had to be at least 2 years at the time of the survey. For the mediation analysis, children had to be at least 2 years at T1. Children who had grown shorter between measurements or with biologically implausible values of BMIz (that is, <−4 or >8), or weight-for-age z-scores or height-for-age z-scores (<−3 or >5) were excluded. Children whose biological mothers did not respond to the survey, mothers with improbable BMIs (<15 or >56 kg/m2), or who were missing on any of the measures were also excluded. The final sample size was 2307 and 753 for the mediation analysis. See Fig. 1 for study exclusion criteria.
Fig. 1.
Flow chart of children excluded in each step to obtain final sample sizes for the cross-sectional and mediation analyses.
Univariate and bivariate analyses were conducted. Multiple logistic regression was used to examine the cross-sectional association of SHCB and obesity. The models adjusted for child's age, gender, race/ethnicity, household income, mother's BMI and education, neighborhood median household income, year of survey, and duration. All theorized household and individual level confounders were included in the final model since research has found that they are associated with both obesity and SHCB. To test for moderation, multiple logistic regression was used to examine the association of childhood obesity and the interaction term of SHCB with each potential moderator, adjusting for the previously mentioned covariates. For the mediation analysis, we first conducted multiple linear regression to examine the association of SHCB with ΔBMIz. We then used mediation methods outlined by MacKinnon to test each potential mediator (MacKinnon, 2008). The above-mentioned covariates were controlled for as well as BMIz at T1. The mediated effects were estimated by the PROCESS macro which uses a bootstrapping method (http://www.processmacro.org/). Tests for statistical significance were based on a P-value < .05. Analyses were conducted in SAS version 9.4 (SAS Institute, Cary, NC).
3. Results
Compared to children who were at least 2 years of age at the time of the survey (n = 6666), children in the cross-sectional sample of 2307 were slightly younger, more likely to be Hispanic and less likely to be Asian. They were also more likely to have mothers with higher education and better mental health. They were less likely to live in family-owned homes, and more likely to live with family and to experience residential mobility.
Nearly 16% of these children lived in SHCB households (Table 1). These children were significantly less likely to be Hispanic and to live in households that only had a high-school degree, and were more likely to live in extremely poor (≤50% FPL) households than children living in non-SHCB households (Table 1). Children living in SHCB households were also significantly more likely to be obese compared to children living in non-SHCB households (Table 1).
Table 1.
Sociodemographic characteristics and the home environment of the sample of 2–5-year-old children by severe housing-cost burden,a 2011 and 2014 Los Angeles County WIC Survey.
| Total (n = 2307) Mean (SD) or % |
Not severe housing-cost burden (n = 1940) Mean (SD) or % |
Severe housing-cost burden (n = 367) Mean (SD) or % |
Pb | |
|---|---|---|---|---|
| Sociodemographic characteristics | ||||
| Child's age at survey (yrs) | 3.1 (0.7) | 3.1 (0.7) | 3.2 (0.6) | .12 |
| Child's gender (female) | 47.7% | 47.8% | 47.1% | .82 |
| Child's race/ethnicity | .03 | |||
| NH white | 2.5 | 2.3 | 3.3 | |
| NH black | 6.8 | 6.6 | 7.6 | |
| NH Asian | 1.7 | 1.8 | 1.1 | |
| Hispanic | 87.5 | 88.0 | 84.7 | |
| NH multiple race | 1.6 | 1.3 | 3.3 | |
| Mother's education | .006 | |||
| < High school | 35.9% | 35.3% | 39.5% | |
| High school | 30.8% | 32.1% | 23.7% | |
| ≥ Some college | 33.3% | 32.6% | 36.8% | |
| Household income | <.001 | |||
| ≤50% FPL | 30.0 | 27.8 | 41.7 | |
| 50.1–100% FPL | 47.9 | 48.7 | 43.6 | |
| 100.1–133% FPL | 12.7 | 13.5 | 8.7 | |
| 133.1–185% FPL | 9.4 | 10.0 | 6.0 | |
| Neighborhood median household income ($) | $43,116 (15,372) | $43,116 (15,408) | $43,117 (15,200) | .99 |
| Months from survey to time of measurement | 5.9 (2.7) | 5.9 (2.7) | 5.9 (2.7) | .91 |
| Housing and home environment | ||||
| Housing tenure | ||||
| Renting | 76.4% | 77.7% | 69.5% | <.001 |
| Living with relatives | 16.2% | 14.6% | 24.8% | |
| Living in home they own | 6.8% | 7.2% | 4.6% | |
| Other | 0.7% | 0.6% | 1.1% | |
| At least 5 people in household | 53.0% | 52.8% | 53.7% | .77 |
| Very difficult to find housing | 24.7% | 17.0% | 65.4% | <.001 |
| At least 2 moves in 3 years | 12.1% | 11.0% | 18.3% | <.001 |
| Food insecurity | 33.2% | 29.2% | 54.5% | <.001 |
| Mother's and child's health | ||||
| % children who are obesec | 17.8% | 17.1% | 21.5% | .04 |
| Mother's BMI (kg/m2)d | 28.6 (6.1) | 28.6 (6.1) | 28.8 (6.2) | .55 |
| Mother with depressive symptoms | 13.1% | 11.6% | 20.7% | <.001 |
| Survey year (2011) | 35.1% | 34.1% | 40.1% | .03 |
Notes. NH = Non-Hispanic; FPL = Federal Poverty Level.
16% of children in the sample lived in households that perceived to be severe housing-cost burdened and 84% did not.
P-value of chi-square test or t-test of differences by severe housing-cost burden.
Obesity is a BMI z-score ≥ 95th percentile of CDC's gender- and age-specific growth reference values.
Mother's BMI based on self-report of height and weight.
SHCB households had greater difficulty finding housing and were more likely to live with relatives than non-SHCB households, although household size was similar (Table 1). Children living in SHCB households were significantly more likely than their non-SHCB counterparts to live in a stressful home environment, characterized by frequent residential mobility, having a mother with depressive symptoms, and living in a food-insecure household (Table 1).
No statistically significant differences existed by SHCB for child's health behaviors in either sample (Table 2). However, children's behaviors among the cross-sectional and mediation samples were slightly different. More children living in SHCB households in the mediation sample watched at least 2 h of screen time a day and drank less than one SSB a day compared to their counterparts in the cross-sectional sample (Table 2).
Table 2.
Health behaviors of 2–5-year-old children by severe housing-cost burden and analytic sample, 2011 and 2014 Los Angeles County WIC Survey.
| Cross-sectional analytic sample |
Mediation analytic sample |
|||
|---|---|---|---|---|
| Not severe housing-cost burden (n = 1940) Mean (SD) or % |
Severe housing-cost burden (n = 367) Mean (SD) or % |
Not severe housing-cost burden (n = 640) Mean (SD) or % |
Severe housing-cost burden (n = 113) Mean (SD) or % |
|
| Change in BMIz | – | – | 0.014 (0.762) | 0.004 (0.691) |
| Fruit and vegetable consumption | ||||
| ≤2 servings/day | 6.2% | 7.6% | 6.7% | 8.0% |
| 3–4 servings/day | 29.6% | 31.6% | 29.4% | 32.7% |
| ≥5 servings/day | 64.2% | 60.8% | 63.9% | 59.3% |
| Fast fooda | ||||
| <1 a month | 12.5% | 14.4% | 12.0% | 11.5% |
| <1 a week to l ≥ a month | 34.3% | 31.9% | 33.9% | 31.0% |
| ≥1 time per week | 53.2% | 53.7% | 54.1% | 57.5% |
| SSBb | ||||
| <1 (times/day) | 38.0% | 34.1% | 35.6% | 45.1% |
| ≥1 (times/day) | 62.0% | 65.9% | 64.4% | 54.5% |
| Sweet foodsc | ||||
| <1 (times/day) | 25.8% | 22.3% | 25.6% | 25.7% |
| ≥1 (times/day) | 74.2% | 77.7% | 74.4% | 74.3% |
| Unhealthy food scored | ||||
| 0 (not unhealthy) | 8.9% | 7.1% | 8.0% | 7.1% |
| 1 | 25.3% | 21.8% | 26.6% | 27.4% |
| 2 | 33.3% | 37.9% | 30.2% | 37.2% |
| 3 (very unhealthy) | 32.5% | 33.2% | 35.3% | 28.3% |
| Screen timee | ||||
| <2 h/day | 47.4% | 44.4% | 46.9% | 38.9% |
| ≥2 h/day | 52.6% | 55.6% | 53.1% | 61.1% |
P-value of chi-square test or t-test of differences by severe housing-cost burden within each analytic sample: * < .05; ** < .01; *** < .001.
Fast food is a restaurant like McDonald's, Taco Bell, Burger King, KFC or another similar place.
SSBs are sugar-sweetened beverages such as sweetened milk, non-100% juice, sweetened drinks and sodas.
Sweet foods include sweets or sweetened foods such as sweetened cereals, fruit bars, pop-tarts, donuts, cookies and candies.
Based on eating fast food at least once a week, drinking a SSB at least once a day, and eating a sweet food at least once a day.
Screen time includes television and video or computer games.
Living in SHCB households was associated with an increase in the odds of obesity [OR (95% CI): 1.33 (1.00, 1.78)] after adjusting for child's age, gender and race/ethnicity, mother's education and BMI, household income, duration between survey and outcome, and survey year. Household size was found to be a moderator of the relationship between SHCB and childhood obesity; the more people in the household the greater the strength of the association of SHCB with obesity (Table 3). Food insecurity, housing tenure, and number of moves were not found to be moderators (results not shown).
Table 3.
Association between severe housing-cost burden and obesity, 2011 and 2014 Los Angeles County WIC Survey.
| OR (95% CI) | |
|---|---|
| Household size × SHCB (not SHCB, ref) |
|
| 4 in household | 1.09 (0.79, 1.52) |
| 5 in household | 1.38 (1.04, 1.85) |
| 7 in household | 2.22 (1.38, 3.56) |
| 9 in household | 3.56 (1.61, 7.83) |
| Test of interaction P-value | .010 |
Notes. OR = odds ratio; CI = confidence interval; SHCB = severe housing-cost burden; NH = Non-Hispanic; FPL = Federal Poverty Level; ref = Reference.
The model included the main effects for SHCB (binary measure) and household size (continuous measure) and the interaction between the two. The model was adjusted for child's age at survey, gender, and race/ethnicity, household income, mother's education and BMI, time between survey and survey year. We present the ORs for the association between SHCB and obesity with household size set to different values. Values in bold are statistically significant.
Although SHCB was not significantly associated with ΔBMIz (Supplemental Table 1), we conducted the mediation analysis since it is possible to have inconsistent mediation (MacKinnon, 2008). Mother's depressive symptoms, and child's unhealthy diet, fruit and vegetable consumption, and screen time were not found to be mediators of the relationship between SHCB and ΔBMIz (Supplemental Table 2).
4. Discussion
Approximately 16% of low-income preschool-aged children participating in WIC in LAC lived in SHCB households. These children had greater odds of obesity and were exposed to more chronic stressors and housing instability than children living in non-SHCB households. Child's diet, sedentary behavior, and mother's mental well-being were not found to be pathways by which SHCB increased the odds of early childhood obesity.
To our knowledge, no study has examined the association between housing-cost burden and obesity among children. However, Garasky and colleagues examined an index of housing related stressors that included unaffordable housing (spending >30% of income on housing) with obesity among children aged 5–17 years and did not find an association (Garasky et al., 2009). Examining the measure as part of an index might have masked its effect. Furthermore, this measure may not get at actual burden since it does not account for the different amount of money households need to meet their basic necessities (HUD User PD&R Edge Home, n.d.). A low-income household with 4 children spending 30% of their income on housing may struggle to make ends meet while their counterpart with only 1 child may not be burdened. Garasky and colleagues examined children who were older and not specifically low-income. There are critical periods in development, and the effect of unaffordable housing may be more discernible in very young children. Additionally, housing-cost burden may influence obesity risk only among low-income families since they have fewer resources to devote to housing costs (Harkness and Newman, 2005) and they may face a real threat of becoming homeless if they are not able to pay rent due to their limited financial savings and social resources (Ma et al., 2008).
The few studies examining the association between housing-cost burden and obesity among adults have found mixed results (Pollack et al., 2010; Nicholas, 2017; Bolívar Muñoz et al., 2016). One study in LAC found that those who could not pay or delayed paying their rent or mortgage were more likely to be obese; however, this study did not control for socioeconomic factors (Nicholas, 2017). In another study, Bolivar Munoz et al. found that difficulty paying rent or undergoing eviction was associated with increased sedentary behavior and decreased fruit and vegetable consumption, but not obesity (Bolívar Muñoz et al., 2016). Using a measure that was similar to ours, Pollack and colleagues did not find an association between housing-cost burden and obesity; however, they examined any difficulty paying for housing and not just severe difficulty (Pollack et al., 2010).
The lack of association between SHCB and change in adiposity could be due to the sample size not being large enough to detect a statistically significant change. The sample for the mediation analyses was a third of that used for the cross-sectional analysis and only 16% of children lived in SHCB households. It could also be that the interval of time between T1 and T2 was not adequate for change to be detected. Half of the sample had time intervals of a year or less. Children grow steadily at that age and more time may be needed to see an increase in adiposity.
We did not find children's sedentary behavior or diet to mediate the relationship between SHCB and change in adiposity. While this might be due to insufficient power to detect an effect, children's physical activity might not be affected by the amount of screen time. Among older, low-income children, while financial strain was associated with children's sedentary behavior it was also positively associated with children's physical activity (Lundahl et al., 2013).
In the US, SHCB households with children in the lowest income quartile spend, on average, a little less than $300 a month on food while their non-SHCB counterparts spend approximately $500 a month (Joint Center for Housing Studies of Harvard University, 2018). The supplemental foods and fruit and vegetable voucher WIC provides might enable SHCB households to maintain a certain quality for their children's diet.
Although mothers living in SHCB households were at greater risk of depression, we did not find it to be a mediator. This could be due to the small sample size or to factors that buffer the effect of mother's depression. More than half of the children lived in households with 5 or more people. These individuals may help with child care or they may provide the mother social support which can buffer feelings of stress and depression (Campos et al., 2014; Ditzen and Heinrichs, 2014). Additionally, the majority of the study population was Hispanic. Familism, where “close, supportive family relationships” are emphasized, is greater among Hispanic families and it has been found to improve psychological health through increased social support (Campos et al., 2014).
Household size was found to moderate the relationship between SHCB and childhood obesity, with larger households increasing its effect. The crowding resulting from ‘doubling-up’ can add to the chaos and stress of the environment (Evans, 2004). Household chaos can dysregulate the biological stress-response system in low-income young children (Lumeng et al., 2014) and their mothers may not be as responsive (Evans et al., 2010).
While research has found home ownership to moderate the relationship between unaffordable housing and health (Pollack et al., 2010), our lack of findings could be because of the small percentage of homeowners. Although a greater share of households experiencing SHCB lived with relatives, these households may reap the previously-mentioned benefits of informal child care and social support that offset the chaos and stress of crowding. Contrary to other studies (Kimbro and Denney, 2013) we did not find neighborhood median household income to be associated with obesity. The lack of findings could be because of the lack of variation in this sample with many of the children living in similar low-income neighborhoods.
4.1. Strengths and limitations
To our knowledge, this is the first study to examine the effect of SHCB on obesity among preschool-aged children. This study also examined often-hypothesized mechanisms by which a chronic financial stressor can increase the risk of obesity among an age group that is infrequently studied (Miller et al., 2017). The effect size of SHCB on childhood obesity among low-income children might be underestimated since the study sample consists of WIC families who receive nutrition education and supplemental foods that include a fruit and vegetable voucher. These might buffer the negative impact of SHCB on risk of childhood obesity. While it is impossible to infer causality from this study, we ensured temporal precedence for both the cross-sectional and the mediation analyses by using measurements after the survey occurred for the former, and having the second measurement of adiposity occur after the survey for the latter.
This study's limitations include not knowing the duration of SHCB. Whether a stressor is acute or chronic is important to determine its potential impact. Is the experience of SHCB a one-time event and the household has the financial and/or social resources to get through the difficulty? Or is it a continuous experience and the household has exhausted the financial and social resources from which to draw?
We were not able to account for the receipt of housing assistance, such as public housing, housing choice voucher programs (Section 8), and subsidized rent (Aratani et al., 2011). If the situation of WIC-participating households in Los Angeles is similar to that of low-income families with children in the United States, we foresee approximately 13% of our sample to have been receiving housing assistance (Edelstein et al., 2014). Participation in these programs would underestimate the association between SHCB and early childhood obesity. While households who live in subsidized housing may still struggle to pay for housing, they might experience less stress and better dietary and physical activity outcomes because of greater residential stability and the ability to spend more money on healthy food (Aratani et al., 2011; Newman and Holupka, 2017).
The lack of significant findings for the mediators may be partially due to the measures' validity. Some of the diet measures had low to medium validity (Koleilat and Whaley, 2016) and the screen time questions have not been validated. The PHQ-2 has been validated for English-speakers but not Spanish-speakers (Kroenke et al., 2003; Reuland et al., 2009).
Findings may not be generalizable to older children since there are critical periods in a child's growth and development which might make them more vulnerable to chronic stressors. Furthermore, SHCB might not be a chronic stressor among older children. Stressors that induce feelings of instability might be more important in younger children while interpersonal and academic stressors might be more important in adolescence (Garasky et al., 2009).
5. Conclusion
Findings highlight the importance of considering housing-cost burden as a risk factor for childhood obesity and advance our understanding of the mechanisms by which financial chronic stress increases the risk of childhood obesity. While future research should explore the behavioral, biologic and psychosocial mechanisms by which housing-cost burden influences the risk of obesity, our findings have implications for obesity prevention programs and the importance of identifying children most in need.
Conflicts of interest
None.
Acknowledgements
We gratefully acknowledge Dr. Judith Siegel, Kiran Saluja, Judy Gomez, Mike Whaley, and Armando Jimenez for their contributions to this work. We also thank the Eunice Kennedy Shriver National Institute of Child Health and Human Development [grant number 1R01HD072296] and First 5 LA for their support.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2018.12.003.
Contributor Information
Tabashir Z. Nobari, Email: tabashir@ucla.edu.
Shannon E. Whaley, Email: shannon@phfewic.org.
Evelyn Blumenberg, Email: eblumenb@ucla.edu.
Michael L. Prelip, Email: mprelip@ucla.edu.
May C. Wang, Email: maywang@ucla.edu.
Appendix A. Supplementary data
Supplementary material
References
- Anderson S.E., Whitaker R.C. Attachment security and obesity in US preschool-aged children. Arch. Pediatr. Adolesc. Med. 2011;165(3):235–242. doi: 10.1001/archpediatrics.2010.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aratani Y., Chau M., Wight V.R., Addy S. New York, NY: National Center for Children in Poverty; 2011. Rent burden, housing subsidies and the well-being of children and youth. http://www.nccp.org/publications/pdf/text_1043.pdf Available from.
- Bolívar Muñoz J., Bernal Solano M., Mateo Rodríguez I. La salud de las personas adultas afectadas por un proceso de desahucio. Gac. Sanit. 2016;30(1):4–10. doi: 10.1016/j.gaceta.2015.10.002. [DOI] [PubMed] [Google Scholar]
- Campos B., Ullman J.B., Aguilera A., Dunkel Schetter C. Familism and psychological health: the intervening role of closeness and social support. Cult. Divers. Ethn. Minor. Psychol. 2014;20(2):191–201. doi: 10.1037/a0034094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conger K.J., Rueter M.A., Conger R.D. The role of economic pressure in the lives of parents and their adolescents: the Family Stress Model. In: Crockett L.J.E., Silbereisen R.K.E., editors. Negotiating Adolescence in Times of Social Change. Cambridge University Press; New York, NY: 2000. pp. 201–223. [Google Scholar]
- Crespi C.M., Alfonso V.H., Whaley S.E., Wang M.C. Validity of child anthropometric measurements in the Special Supplemental Nutrition Program for Women, Infants, and Children. Pediatr. Res. 2012;71(3):286–292. doi: 10.1038/pr.2011.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniels S.R., Hassink S.G. The role of the pediatrician in primary prevention of obesity. Pediatrics. 2015;136(1):e275–e292. doi: 10.1542/peds.2015-1558. [DOI] [PubMed] [Google Scholar]
- Davison K.K., Jurkowski J.M., Lawson H.A. Reframing family-centred obesity prevention using the Family Ecological Model. Public Health Nutr. 2013;16(10):1861–1869. doi: 10.1017/S1368980012004533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ditzen B., Heinrichs M. Psychobiology of social support: the social dimension of stress buffering. Restor. Neurol. Neurosci. 2014;32:149–162. doi: 10.3233/RNN-139008. [DOI] [PubMed] [Google Scholar]
- Downing J. The health effects of the foreclosure crisis and unaffordable housing: a systematic review and explanation of evidence. Soc. Sci. Med. 2016;162:88–96. doi: 10.1016/j.socscimed.2016.06.014. [DOI] [PubMed] [Google Scholar]
- Edelstein S., Pergamit M.R., Ratcliffe C. Washington, DC: Urban Institute; 2014. Characteristics of families receiving multiple public benefits. https://www.urban.org/sites/default/files/publication/22366/413044-Characteristics-of-Families-Receiving-Multiple-Public-Benefits.PDF Available from.
- Evans G.W. The environment of childhood poverty. Am. Psychol. 2004;59(2):77–92. doi: 10.1037/0003-066X.59.2.77. [DOI] [PubMed] [Google Scholar]
- Evans G.W., Ricciuti H.N., Hope S. Crowding and cognitive development: the mediating role of maternal responsiveness among 36-month-old children. Environ. Behav. 2010;42(1):135–148. [Google Scholar]
- Feeding America, Family Resiliency Center, Abt SRBI Short supply: American families struggle to secure everyday essentials. Chicago, IL. 2013. http://www.feedingamerica.org/research/in-short-supply/in-short-supply-executive.pdf Available at.
- Franklin B., Jones A., Love D., Puckett S., Macklin J., White-Means S. Exploring mediators of food insecurity and obesity: a review of recent literature. J. Community Health. 2012;37(1):253–264. doi: 10.1007/s10900-011-9420-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garasky S., Stewart S.D., Gundersen C., Lohman B.J., Eisenmann J.C. Family stressors and child obesity. Soc. Sci. Res. 2009;38(4):755–766. doi: 10.1016/j.ssresearch.2009.06.002. [DOI] [PubMed] [Google Scholar]
- Gunnar M., Quevedo K. The neurobiology of stress and development. Annu. Rev. Psychol. 2007;58(1):145–173. doi: 10.1146/annurev.psych.58.110405.085605. [DOI] [PubMed] [Google Scholar]
- Harkness J., Newman S.J. Housing affordability and children's well-being: evidence from the national survey of America's families. Hous. Policy Debate. 2005;16(2):223–255. [Google Scholar]
- HUD User PD&R Edge Home Rental burdens: rethinking affordability measures. Washington, DC. https://www.huduser.gov/portal/pdredge/pdr_edge_featd_article_092214.html Available from.
- Joint Center for Housing Studies of Harvard University The State of the Nation's Housing 2018. Cambridge, MA. 2018. http://www.jchs.harvard.edu/sites/default/files/Harvard_JCHS_State_of_the_Nations_Housing_2018.pdf Available at.
- Kimbro R.T., Denney J.T. Neighborhood context and racial/ethnic differences in young children's obesity: structural barriers to interventions. Soc. Sci. Med. 2013;95:97–105. doi: 10.1016/j.socscimed.2012.09.032. [DOI] [PubMed] [Google Scholar]
- Kirkpatrick S.I., Tarasuk V. Adequacy of food spending is related to housing expenditures among lower-income Canadian households. Public Health Nutr. 2007;10(12):1464–1473. doi: 10.1017/S136898000700081X. [DOI] [PubMed] [Google Scholar]
- Kirkpatrick S.I., Tarasuk V. Housing circumstances are associated with household food access among low-income urban families. J. Urban Health. 2011;88(2):284–296. doi: 10.1007/s11524-010-9535-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koleilat M., Whaley S.E. Reliability and validity of food frequency questions to assess beverage and food group intakes among low-income 2- to 4-year-old children. J. Acad. Nutr. Diet. 2016;116(6):931–939. doi: 10.1016/j.jand.2016.02.014. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med. Care. 2003;41(11):1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- Kuczmarski R.J., Ogden C.L., Guo S.S. 2000 CDC growth charts for the United States: methods and development. Vital Health Stat. 2002;11(246):1–190. [PubMed] [Google Scholar]
- Lampard A.M., Jurkowski J.M., Davison K.K. The family context of low-income parents who restrict child screen time. Child. Obes. 2013;9(5):386–392. doi: 10.1089/chi.2013.0043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lampard A.M., Franckle R.L., Davison K.K. Maternal depression and childhood obesity: a systematic review. Prev. Med. (Baltim.) 2014;59:60–67. doi: 10.1016/j.ypmed.2013.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lumeng J.C., Miller A., Peterson K.E. Diurnal cortisol pattern, eating behaviors and overweight in low-income preschool-aged children. Appetite. 2014;73:65–72. doi: 10.1016/j.appet.2013.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundahl A., Nelson T.D., Van Dyk T.R., West T. Psychosocial stressors and health behaviors: examining sleep, sedentary behaviors, and physical activity in a low-income pediatric sample. Clin. Pediatr. (Phila) 2013;52(8):721–729. doi: 10.1177/0009922813482179. [DOI] [PubMed] [Google Scholar]
- Ma C.T., Gee L., Kushel M.B. Associations between housing instability and food insecurity with health care access in low-income children. Ambul. Pediatr. 2008;8(1):50–57. doi: 10.1016/j.ambp.2007.08.004. [DOI] [PubMed] [Google Scholar]
- MacKinnon D.P. Lawrence Erlbaum Associates; 2008. Introduction to Statistical Mediation Analysis. [Google Scholar]
- Metallinos-Katsaras E., Must A., Gorman K. A longitudinal study of food insecurity on obesity in preschool children. J. Acad. Nutr. Diet. 2012;112(12):1949–1958. doi: 10.1016/j.jand.2012.08.031. [DOI] [PubMed] [Google Scholar]
- Miller A., Dawson L., Welker E. Stress in early life and childhood obesity risk. Durham, NC. 2017. http://healthyeatingresearch.org/wp-content/uploads/2017/06/her_stress_obesity_5-30.pdf Available at.
- Newman S., Holupka C.S. The effects of assisted housing on child well-being. Am. J. Community Psychol. 2017;60:66–78. doi: 10.1002/ajcp.12100. [DOI] [PubMed] [Google Scholar]
- Nicholas W. Measure H: preventing and reducing homelessness in Los Angeles County–a health impact assessment. 2017. http://www.pewtrusts.org/~/media/assets/external-sites/health-impact-project/measure-h.pdf?la=en Available at.
- Parks E.P., Kumanyika S., Moore R.H., Stettler N., Wrotniak B.H., Kazak A. Influence of stress in parents on child obesity and related behaviors. Pediatrics. 2012;130(5):e1096–e1104. doi: 10.1542/peds.2012-0895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilkauskas N.V., Garfinkel I., McLanahan S.S. The prevalence and economic value of doubling up. Demography. 2014;51(5):1667–1676. doi: 10.1007/s13524-014-0327-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollack C.E., Griffin B.A., Lynch J. Housing affordability and health among homeowners and renters. Am. J. Prev. Med. 2010;39(6):515–521. doi: 10.1016/j.amepre.2010.08.002. [DOI] [PubMed] [Google Scholar]
- Rehm C.D., Monsivais P., Drewnowski A. The quality and monetary value of diets consumed by adults in the United States. Am. J. Clin. Nutr. 2011;94(5):1333–1339. doi: 10.3945/ajcn.111.015560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Repetti R.L., Taylor S.E., Seeman T.E. Risky families: family social environments and the mental and physical health of offspring. Psychol. Bull. 2002;128(2):330–366. [PubMed] [Google Scholar]
- Reuland D.S., Cherrington A., Watkins G.S., Bradford D.W., Blanco R.A., Gaynes B.N. Diagnostic accuracy of Spanish language depression-screening instruments. Ann. Fam. Med. 2009;7(5):455–462. doi: 10.1370/afm.981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schreier H.M.C., Chen E. Socioeconomic status and the health of youth: a multilevel, multidomain approach to conceptualizing pathways. Psychol. Bull. 2013;139(3):606–654. doi: 10.1037/a0029416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tate E.B., Wood W., Liao Y., Dunton G.F. Do stressed mothers have heavier children? A meta-analysis on the relationship between maternal stress and child body mass index. Obes. Rev. 2015;16(5):351–361. doi: 10.1111/obr.12262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theodos B., McTarnaghan S., Coulton C. Washington, DC: Urban Institute; 2018. Family residential instability: what can states and localities do? https://www.urban.org/sites/default/files/publication/98286/family_residential_instability_what_can_states_and_localities_do_1.pdf Available at.
- Williams C., AZA Consulting, Rosen J., Hudman J., O'Malley M., Kaiser Commission on Medicaid and the Uninsured Challenges and tradeoffs in low-income family budgets: implications for health coverage. 2004. https://kaiserfamilyfoundation.files.wordpress.com/2013/01/challenges-and-tradeoffs-in-low-income-family-budgets-implications-for-health-coverage.pdf Available at.
- Wilson S.M., Sato A.F. Stress and paediatric obesity: what we know and where to go. Stress. Health. 2014;30(2):91–102. doi: 10.1002/smi.2501. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material