Abstract
Background
Coronary artery disease (CAD) is a leading cause of morbidity and death. Early diagnosis of patients with left main and/or three-vessel disease (LM/3VD) among acute coronary syndrome (ACS) patients is beneficial. The relation between erectile dysfunction (ED) and cardiovascular diseases was previously noticed. The aim of our work was to find out if the severity of ED could predict the presence of LM/3VD in ACS patients.
Patients and methods
Eighty-five male patients with ACS were included in the study. Clinical assessment, estimation of international index of erectile function (IIEF) score, and coronary angiography were performed in all patients. Gensini score was calculated to assess the severity of CAD. Based on IIEF score, the patients were divided into two groups: Group 1: patients with mild or no ED (IIEF score ≥17), Group 2: patients with moderate or severe ED (IIEF score <17).
Results
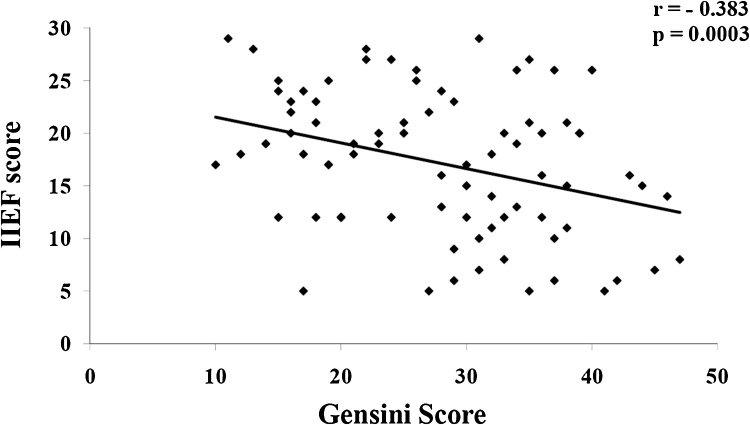
Patients with IIEF score <17 had significantly higher prevalence of LM CAD (4.3% versus 18.4%, p = 0.035), 3VD (17% versus 39.5%, p = 0.021) and LM/3VD (21.3% versus 55.3%, p = 0.0012), as well as higher mean Gensini score (23.5 ± 10.8 versus 34.1 ± 12.7, p = 0.0001). The independent predictors of LM/3VD in order of significance were: age, heart rate, IIEF <17, Killip class >1, and ST-depression or ST-elevation in lead aVR ≥1 mV. There was a significant negative correlation between IIEF score and Gensini score (r = −0.383, p = 0.0003).
Conclusion
The presence of moderate or severe ED in men with ACS is associated with higher Gensini score and more incidence of LM/3VD. IIEF score <17 was an independent predictor of LM/3VD.
Keywords: Erectile dysfunction, Left main disease, Three-vessel disease, Acute coronary syndrome
1. Introduction
Coronary artery disease (CAD) is a leading cause of morbidity and death all around the world.1 In patients with non-ST-segment elevation acute coronary syndrome (ACS), the presence of left main and/or three-vessel disease (LM/3VD) carries an outstanding higher risk of adverse cardiovascular events.2, 3
Early invasive strategy with revascularization is particularly indicated in ACS patients with LM/3VD to improve their outcome.4 Hence, early diagnosis of such patients upon presentation appears to be of an utmost benefit.
Erectile dysfunction (ED) is defined as the inability to achieve and/or to maintain erection that is necessary for satisfactory sexual intercourse.5 The pathophysiological mechanism and risk factors of developing ED are quite similar to those of CAD with endothelial dysfunction as the major component affecting different vascular beds of various diameters.6
The relation between ED and cardiovascular diseases was previously noticed. ED was found to be associated with subclinical left ventricular dysfunction,7 increased incidence of asymptomatic CAD,8 increased risk for CAD morbidity and mortality.9 The severity of ED was also found to be correlated with angiographic extent of CAD.10
The aim of this study was to find out if the severity of ED could predict the presence of LM/3VD in ACS patients.
2. Patients and methods
The study included 85 male patients with non-ST-segment elevation ACS who were admitted to the coronary care unit of the Cardiology Department, Zagazig University during the period from January 2015 till December 2016. The diagnosis of ACS was made according to the 2014 AHA/ACC guideline for the management of patients with non-ST-elevation ACS.11
Patients with history of previous myocardial infarction (MI), previous revascularization procedures, or those with any other contraindication for coronary angiography were excluded from the study.11 Also, patients with known neurologic, psychiatric or endocrine disease that may affect erectile function were excluded. Additionally, patients who had a history of pelvic, urethral, or prostatic surgery and those who were receiving treatment for ED were also excluded from the study. Single patients were also excluded from our study.
The Institutional Review Board had approved the study protocol. Written informed consent was obtained from every patient.
All the subjects underwent:
-
1)
Clinical assessment which included history and physical examination.
-
2)
International index of erectile function (IIEF) score estimation: After stabilization of the clinical condition, all patients were evaluated using the IIEF 15-item, self-administered questionnaire,12 which was translated into Arabic.
According to the results of IIEF questionnaire, patients were divided into two groups:
Group 1: patients with mild or no ED (IIEF score ≥ 17). This group included 47 patients.
Group 2: patients with moderate or severe ED (IIEF score <17).12 This group included 38 patients.
-
1)
Coronary Angiography: The coronary artery system was visually estimated by an expert angiographer who was unaware of patients’ clinical data. The coronary artery narrowing was expressed as percentage of luminal diameter stenosis. Lesions with ≥ 70% narrowing in major epicardial artery or ≥50% narrowing in the left main coronary artery were considered as having significant angiographic stenosis.13
Gensini score was calculated to assess the angiographic severity. Every lesion was assigned a score according to the percentage of stenosis- 1 for 25% stenosis, 2 for 50%, 4 for 75%, 8 for 90%, 16 for 99% and 32 for total occlusion. The score was then multiplied by a factor according to the site of the lesion.14
3VD was defined if there were significant obstructive CAD in all 3 major epicardial coronary arteries, namely left anterior descending, left circumflex and right coronary arteries.
2.1. Statistical analysis
All data were analyzed using the SPSS for Windows package program (Version 20.0; Armonk, NY, USA: IBM Corp.). Differences between patients' group and control group were analyzed using χ2 test and student’s t-test. Correlations between different variables were investigated by Pearson correlation analysis. A p value <0.05 was regarded as being statistically significant.
3. Results
As shown in Table 1, there was no significant difference between the two study groups regarding age, hypertension, diabetes mellitus (DM), smoking, or serum lipids. There was also no significant difference between the two groups regarding the chronic use of drugs (beta blockers, diuretics, angiotensin-converting-enzyme inhibitor, angiotensin receptor blockers, calcium channel blockers, nitrates, statins, aspirin, oral hypoglycemic, or Insulin) (Table 2).
Table 1.
Demographic data and risk factors in the two groups according to the severity of endothelial dysfunction.
| IIEF score ≥ 17 (n = 47) | IIEF score < 17 (n = 38) | p | |
|---|---|---|---|
| Age (years) | 47.5 ± 9.84 | 50.3 ± 10.21 | 0.205 |
| Hypertension | 18 (38.3%) | 16 (42.1%) | 0.722 |
| Diabetes | 13 (27.6%) | 14 (36.8%) | 0.366 |
| Smoking | 15 (34.1%) | 12 (31.6%) | 0.974 |
| Total Cholesterol (mg/dl) | 195.2 ± 41.5 | 198.4 ± 39.7 | 0.718 |
| LDL (mg/dl) | 112.4 ± 28.7 | 117.3 ± 26.2 | 0.414 |
| HDL (mg/dl) | 40.1 ± 9.41 | 38.7 ± 8.57 | 0.476 |
| Triglyceride (mg/dl) | 153.4 ± 37.5 | 161.2 ± 36.2 | 0.334 |
Data are expressed as mean ± SD or number (%). LDL = low density lipoprotein, HDL = high density lipoprotein.
Table 2.
Chronic drugs in the two groups according to the severity of endothelial dysfunction.
| IIEF score ≥ 17 (n = 47) | IIEF score < 17 (n = 38) | p | |
|---|---|---|---|
| Beta blockers | 6 (12.8%) | 5 (13.1%) | 0.957 |
| Diuretics | 3 (6.4%) | 3 (7.9%) | 0.787 |
| ACEIs | 8 (17%) | 7 (18.4%) | 0.866 |
| ARBs | 2 (4.2%) | 3 (7.9%) | 0.478 |
| Calcium channel blockers | 9 (19.1%) | 7 (18.4%) | 0.827 |
| Nitrates | 6 (12.8%) | 7 (18.4%) | 0.471 |
| Statins | 12 (25.5%) | 10 (26.3%) | 0.935 |
| Aspirin | 11 (23.4%) | 10 (26.3%) | 0.757 |
| Oral hypoglycemic | 8 (17%) | 8 (21%) | 0.636 |
| Insulin | 5 (10.6%) | 6 (15.8%) | 0.482 |
Data are expressed as number (%). ACEIs = Angiotensin converting enzyme inhibitors. ARBs = Angiotensin receptor blockers.
Regarding coronary angiography results, as shown in Table 3, the patients with IIEF score <17 had significantly higher prevalence of LM CAD (4.3% versus 18.4%, p = 0.035), 3VD (17% versus 39.5%, p = 0.021), and LM/3VD (21.3% versus 55.3%, p = 0.0012). Also, mean Gensini score was significantly higher in patients with IIEF score < 17 (23.5 ± 10.8 versus 34.1 ± 12.7, p = 0.0001). There was a significant negative correlation between IIEF score and Gensini score (r = −0.383, p = 0.0003) (Fig. 1).
Table 3.
Coronary angiography findings in the two groups according to the severity of endothelial dysfunction.
| IIEF score ≥ 17 (n = 47) | IIEF score < 17 (n = 38) | p | |
|---|---|---|---|
| Diseased vessel | |||
| - LMCA | 2 (4.3%) | 7 (18.4%) | 0.035 |
| - LAD | 35 (74.4%) | 31 (81.6%) | 0.434 |
| - LCX | 27 (57.4%) | 27 (71.1%) | 0.195 |
| - RCA | 20 (42.6%) | 22 (57.9%) | 0.159 |
| Number of diseased vessels | |||
| - Single vessel | 20 (42.6%) | 11 (28.9%) | 0.195 |
| - Two vessels | 19 (40.4%) | 12 (31.6%) | 0.399 |
| - Three vessels | 8 (17%) | 15 (39.5%) | 0.021 |
| LM/3VD | 10 (21.3%) | 21 (55.3%) | 0.0012 |
| Gensini score | 23.5 ± 10.8 | 34.1 ± 12.7 | 0.0001 |
Data are expressed as mean ± SD or number (%). LMCA = left main coronary artery, LAD = left anterior descending, LCX = left circumflex, RCA = right coronary artery. LM/3VD = Left main or three vessel disease.
Fig. 1.
Correlation between IIEF score and Gensini score.
Logistic regression analysis for independent predictors of LM/3VD is shown in Table 4. The independent predictors of LM/3VD in order of significance were: age (p = 0.00024), heart rate (p = 0.00013), IIEF <17 (p = 0.0057), Killip class >1 (p = 0.011), and ST-depression or ST-elevation in lead aVR ≥1 mV (p = 0.027).
Table 4.
Logistic regression analysis for predictors of LM/3VD.
| Variables | Odds ratio | 95% CI | p |
|---|---|---|---|
| Age | 4.15 | 3.61–4.69 | 0.00024 |
| Heart rate | 3.87 | 3.11–4.63 | 0.00013 |
| IIEF score <17 | 3.21 | 2.84–3.58 | 0.0057 |
| Killip class >1 | 2.87 | 2.03–3.71 | 0.011 |
| ST-depression, or ST-elevation in aVR ≥ 1 mV | 2.53 | 1.83–3.23 | 0.027 |
CI = Confidence Interval. IIEF: International index of erectile function.
4. Discussion
In our study, the angiographic severity of CAD was found to be more in patients with moderate or severe ED (IIEF score <17). These patients had a significantly higher mean Gensini score and a significantly higher incidence of LV/3VD than patients with mild or no ED (IIEF score ≥17).
ED could be considered as a part of the systemic manifestations of atherosclerosis. Both ED and CAD seem to share the same risk factors and to show similar characteristics such as endothelial dysfunction.15
The vast majority of the cases of organic ED seem to be due to vascular etiologies. Among the known organic factors for ED, 40.5% are shown to be of arterial origin, 10% of cavernosal origin, 12.5% were due to neurogenic causes, and 1.8% of the patients are found to be associated with endocrinologic causes.16
Hypertension, which is a known risk factor for CAD, has also been found to be a culprit in patients with ED. ED can be considered as an early marker of hypertension.17
DM is also an important risk factor for development of ED; DM patients were found to be at least three times more likely to develop ED than nondiabetic individuals.18
Possible mechanisms by which DM may cause ED include direct complications, endothelial dysfunction, oxidative stress, advanced glycation end products, and DM associated psychological disorders.19
The relation between ED and CAD has been previously studied by several investigators. In their meta-analysis, Dong and his colleagues20 concluded that ED significantly increases the risk of CAD, stroke and all-cause mortality. This increased risk was related to ED and was independent of other CAD risk factors.
The severity of ED was found to be correlated with the number of occluded vessels documented by coronary angiography, in male patients with acute MI.21 Also, the prevalence of ED was found to be higher in men with CAD. Patients with ED were found to have a more extensive CAD as documented by coronary angiography.22
The severity of ED was also found to be strongly correlated to the angiographic severity and complexity of CAD in patients with new onset angina undergoing coronary angiography. This correlation was not only strong but also independent. 10
In patients presented with acute MI, the presence of ED was found to be associated with and adverse outcome. ED was found to be a significant and an independent predictor of death and re-hospitalization in men presented with acute MI.23
Erectile dysfunction was found to be correlated with subclinical left ventricular (LV) deterioration as manifested by increased global longitudinal strain and global circumferential strain. Also, the degree of LV systolic dysfunction was found to be correlated with the degree of ED.24, 25
In our study, the presence of IIEF score <17 was a significant and an independent predictor for the presence of LM/3VD. The independent predictors of LM/3VD in order of significance were: age, heart rate, IIEF <17, Killip class >1, and ST-depression or ST-elevation in lead aVR ≥1 mV.
In the attempt to study if the neutrophil-to-lymphocyte ratio was an independent predictor of LM/3VD in patients with non-ST-segment elevation myocardial infarction, Misumida and colleagues25 found that the independent predictors for LM/3VD were age, male sex, hyperlipidemia, Killip class >1 on admission, neutrophil-to-lymphocyte ratio ≥2.8, ST‐depression ≥0.05 mV, and ST-elevation in lead aVR ≥0.05 mV.
In an earlier study by Kosuge and his colleagues,26 it was found that the independent predictors for LM/3VD in patients with non-ST-segment elevation ACS were age, heart rate, Killip class ≥ 2, prior MI, smoking, DM, positive-Troponin, CK-MB, maximal ST-segment depression, sum of ST-segment depression, number of leads with ST-segment depression, degree of ST-segment elevation in lead aVR, and maximal QRS duration.
In addition to the relatively small number of patients, the major limitation of our study is the subjective nature of IIEF score which was used to diagnose and to define the severity of ED. Also, we did not follow-up our patients to study the impact of moderate or severe ED on their prognosis.
5. Conclusion
The presence of moderate or severe ED in men with ACS is associated with more extensive CAD manifested by higher Gensini score and more incidence of LM/3VD. In men with ACS, IIEF score <17 was a significant and independent predictor for the presence of LM/3VD.
6. Disclosures
The authors declare that there is no conflict of interest.
References
- 1.Harriss L.R., Ajani A.E., Hunt D. Accuracy of national mortality codes in identifying adjudicated cardiovascular deaths. Aust N Z J Public Health. 2011;35:466–476. doi: 10.1111/j.1753-6405.2011.00739.x. [DOI] [PubMed] [Google Scholar]
- 2.Figueras J., Lidón R.M. Coronary reserve, extent of coronary disease, recurrent angina and ECG changes during pain in the in-hospital prognosis of acute coronary syndromes. Eur Heart J. 1993;14:185–194. doi: 10.1093/eurheartj/14.2.185. [DOI] [PubMed] [Google Scholar]
- 3.Kosuge M., Ebina T., Hibi K. An early and simple predictor of severe left main and/or three-vessel disease in patients with non-ST-segment elevation acute coronary syndrome. Am J Cardiol. 2011;107:495–500. doi: 10.1016/j.amjcard.2010.10.005. [DOI] [PubMed] [Google Scholar]
- 4.Amsterdam E.A., Wenger N.K., Brindis R.G. AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. J Am Coll Cardiol. 2014;2014(64):e139–e228. doi: 10.1016/j.jacc.2014.09.017. [DOI] [PubMed] [Google Scholar]
- 5.NIH consensus conference. Impotence. NIH consensus development panel on impotence. JAMA. 1993;270:83–90. [PubMed] [Google Scholar]
- 6.Reriani M., Flammer A.J., Li J. Microvascular endothelial dysfunction predicts the development of erectile dysfunction in men with coronary atherosclerosis without critical stenoses. Coron Artery Dis. 2014;25:552–557. doi: 10.1097/MCA.0000000000000145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Karagöz A., Günaydin Z.Y., Bektaş O., Benli E., Kaya A. Subclinical left ventricular deterioration in patients with erectile dysfunction. Acta Cardiol. 2016;71:557–563. doi: 10.2143/AC.71.5.3167499. [DOI] [PubMed] [Google Scholar]
- 8.Gazzaruso C., Coppola A., Pujia A. Erectile dysfunction as a predictor of asymptomatic coronary artery disease in elderly men with type 2 diabetes. J Geriatr Cardiol. 2016;13:552–556. doi: 10.11909/j.issn.1671-5411.2016.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Katsiki N., Wierzbicki A.S., Mikhailidis D.P. Erectile dysfunction and coronary heart disease. Curr Opin Cardiol. 2015;30:416–421. doi: 10.1097/HCO.0000000000000174. [DOI] [PubMed] [Google Scholar]
- 10.Andrade W.S., Oliveira P., Laydner H., Ferreira E.J., Barreto-Filho J.A. Severity of erectile dysfunction is highly correlated with the syntax score in patients undergoing coronariography. Int Braz J Urol. 2016;42:123–131. doi: 10.1590/S1677-5538.IBJU.2015.0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Amsterdam E.A., Wenger N.K., Brindis R.G. AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;130:e344–426. doi: 10.1161/CIR.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 12.Cappelleri J.C., Rosen R.C., Smith M.D., Mishra A., Osterloh I.H. Diagnostic evaluation of the erectile function domain of the International Index of Erectile Function. Urology. 1999;54:346–351. doi: 10.1016/s0090-4295(99)00099-0. [DOI] [PubMed] [Google Scholar]
- 13.Powell D., Moxey C.F. Diagnostic catheterization. In: Watson S., Gorski K.A., editors. Invasive Cardiology: A Manual for Cath Lab Personnel. 3rd ed. Jones & Bartlett Learning; Sudbury, MA, USA: 2011. pp. 143–162. [Google Scholar]
- 14.Gensini G.G. A more meaningful scoring system for determining the severity of coronary heart disease. Am J Cardiol. 1983;51:606. doi: 10.1016/s0002-9149(83)80105-2. [DOI] [PubMed] [Google Scholar]
- 15.Sullivan M.E., Thompson C.S., Dashwood M.R. Nitric oxide and penile erection: is erectile dysfunction another manifestation of vascular disease. Cardiovasc Res. 1999;43:658–665. doi: 10.1016/s0008-6363(99)00135-2. [DOI] [PubMed] [Google Scholar]
- 16.Caskurlu T., Tasci A.I., Resim S., Sahinkanat T., Ergenekon E. The etiology of erectile dysfunction and contributing factors in different age groups in Turkey. Int J Urol. 2004;11:525–529. doi: 10.1111/j.1442-2042.2004.00837.x. [DOI] [PubMed] [Google Scholar]
- 17.Nunes K.P., Labazi H., Webb R.C. New insights into hypertension-associated erectile dysfunction. Curr Opin Nephrol Hypertens. 2012;21:163–170. doi: 10.1097/MNH.0b013e32835021bd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Maiorino M.I., Bellastella G., Esposito K. Diabetes and sexual dysfunction: current perspectives. Diabetes Metab Syndr Obes. 2014;7:95–105. doi: 10.2147/DMSO.S36455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yamada T., Hara K., Umematsu H., Suzuki R., Kadowaki T. Erectile dysfunction and cardiovascular events in diabetic men: a meta-analysis of observational studies. PLoS One. 2012;7:e43673. doi: 10.1371/journal.pone.0043673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dong J.Y., Zhang Y.H., Qin L.Q. Erectile dysfunction and risk of cardiovascular disease: meta-analysis of prospective cohort studies. J Am Coll Cardiol. 2011;58:1378–1385. doi: 10.1016/j.jacc.2011.06.024. [DOI] [PubMed] [Google Scholar]
- 21.Canat L., Cicek G., Atis G., Gurbuz C., Caskurlu T. Is there a relationship between severity of coronary artery disease and severity of erectile dysfunction. Int Braz J Urol. 2013;39:465–473. doi: 10.1590/S1677-5538.IBJU.2013.04.03. [DOI] [PubMed] [Google Scholar]
- 22.Foroutan S.K., Rajabi M. Erectile dysfunction in men with angiographically documented coronary artery disease. Urol J. 2007;4:28–32. [PubMed] [Google Scholar]
- 23.Apostolovic S., Stanojevic D., Jankovic-Tomasevic R., Salinger-Martinovic S., Kostic T., Perisic Z. Erectile dysfunction as a predictor of 2-year prognosis in acute myocardial infarction. Cardiol J. 2017;(February (2)) doi: 10.5603/CJ.a2017.0006. [DOI] [PubMed] [Google Scholar]
- 24.Karagöz A., Günaydin Z.Y., Bektaş O., Benli E., Kaya A. Subclinical left ventricular deterioration in patients with erectile dysfunction. Acta Cardiol. 2016;71:557–563. doi: 10.2143/AC.71.5.3167499. [DOI] [PubMed] [Google Scholar]
- 25.Misumida N., Kobayashi A., Saeed M., Fox J.T., Kanei Y. Neutrophil-to-lymphocyte ratio as an independent predictor of left main and/or three-vessel disease in patients with non-ST-segment elevation myocardial infarction. Cardiovasc Revasc Med. 2015;16:331–335. doi: 10.1016/j.carrev.2015.05.006. [DOI] [PubMed] [Google Scholar]
- 26.Kosuge M., Ebina T., Hibi K. Early, accurate, non-invasive predictors of left main or 3-vessel disease in patients with non-ST-segment elevation acute coronary syndrome. Circ J. 2009;73:1105–1110. doi: 10.1253/circj.cj-08-1009. [DOI] [PubMed] [Google Scholar]