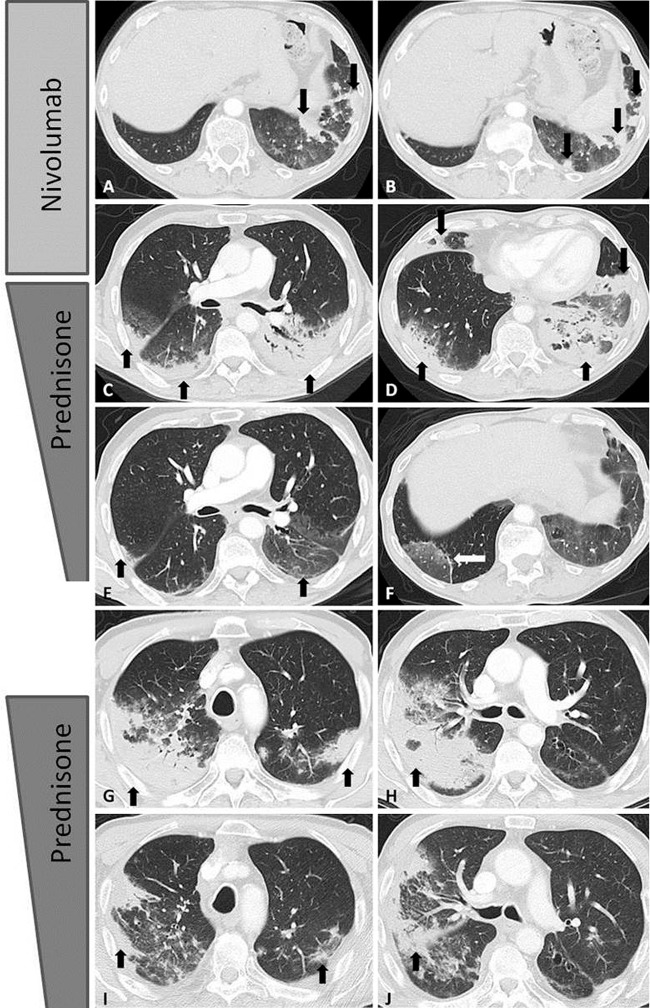
Figure 7:
Axial chest CT scans show programmed cell death protein 1 (PD-1) inhibitor–related pneumonitis in a patient with advanced non–small cell lung cancer treated with nivolumab. A, B, CT scans at 8 weeks of nivolumab therapy show new ground-glass opacities (GGOs), reticular opacities, and consolidation in the lower lobes predominantly on the left, with a peripheral and lower distribution, radiographically representing a cryptogenic organizing pneumonia (COP) pattern (arrows). C, D, On CT scans obtained at 15 weeks of therapy, the findings have substantially increased and involve all lobes, with multifocal areas of GGO, reticular opacities, and consolidation (arrows), as well as centrilobular nodularity and traction bronchiectasis in a predominantly peripheral distribution, demonstrating the overall features of a COP pattern. E, F, Further follow-up CT scans obtained after 4 weeks of prednisone treatment show a marked decrease in the CT findings with residual GGOs, demonstrating a “reversed halo” sign with central GGO surrounded by dense air-space consolidation of a crescentic shape (arrows in F). G, H, CT scans obtained 4 weeks after the completion of prednisone treatment show development of dense consolidations with GGOs and reticular opacities (arrows) in peripheral and multifocal distributions, involving both upper and lower lobes, again demonstrating the COP pattern noted during the first episode of PD-1 pneumonitis. Given the similarity of the radiographic and clinical manifestations to those of the first episode, the patient restarted prednisone for treatment of a “pneumonitis flare.” I, J, Follow-up CT scans obtained 2 weeks after starting the second course of prednisone therapy show decrease of consolidation and GGOs (arrows), indicating improving pneumonitis in response to corticosteroid therapy. (Reprinted, with permission, from reference 55.).