Abstract
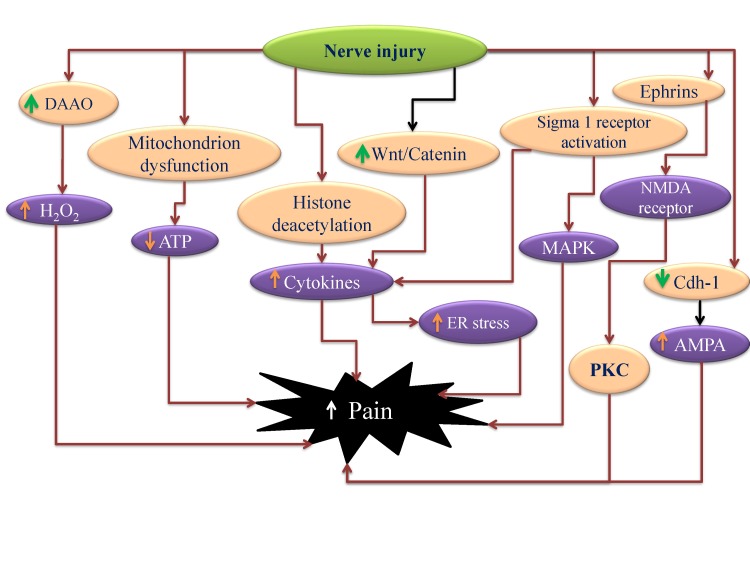
Neuropathic pain is a complex chronic pain state caused by the dysfunction of somatosensory nervous system, and it affects the millions of people worldwide. At present, there are very few medical treatments available for neuropathic pain management and the intolerable side effects of medications may further worsen the symptoms. Despite the presence of profound knowledge that delineates the pathophysiology and mechanisms leading to neuropathic pain, the unmet clinical needs demand more research in this field that would ultimately assist to ameliorate the pain conditions. Efforts are being made globally to explore and understand the basic molecular mechanisms responsible for somatosensory dysfunction in preclinical pain models. The present review highlights some of the novel molecular targets like D-amino acid oxidase, endoplasmic reticulum stress receptors, sigma receptors, hyperpolarization-activated cyclic nucleotide-gated cation channels, histone deacetylase, Wnt/β-catenin and Wnt/Ryk, ephrins and Eph receptor tyrosine kinase, Cdh-1 and mitochondrial ATPase that are implicated in the induction of neuropathic pain. Studies conducted on the different animal models and observed results have been summarized with an aim to facilitate the efforts made in the drug discovery. The diligent analysis and exploitation of these targets may help in the identification of some promising therapies that can better manage neuropathic pain and improve the health of patients.
Keywords: Endoplasmic reticulum stress receptors, Histone deacetylase, Neuropathic pain, Pain treatment
INTRODUCTION
Neuropathic pain is a chronic pain state that is caused by the dysfunction of the somatosensory nervous system. It is characterized by a series of neurobiological events such as unpleasant abnormal sensation (dysesthesia); an increased response to painful stimuli (hyperalgesia); and pain in response to stimuli that do not normally cause pain i.e., allodynia [1,2,3]. Peripheral neuropathic pain may result from damage to the peripheral nerves (sensory, motor or autonomic), which is generally observed in the patients with cancer, AIDS, long standing diabetes, lumbar disc syndrome, herpes infection, traumatic spinal cord injury, multiple sclerosis, stroke, thoractomy, herniorrhaphy, mastectomy and sternotomy [4]. Central neuropathic pain is a consequence of injury of the central nervous system (brain and spinal cord) that may result from spinal cord injury, stroke and multiple sclerosis [5]. Abnormal neuronal activity may develop at the site of injury, in dorsal horn of cell of the spinal cord or at various synaptic regions in the brain that participate in the processing of somatosensory information.
Opioids show limited clinically efficacy in neuropathic pain. Moreover, development of abuse potential and tolerance to pain also limit the common use of opioids in neuropathic pain. Tricyclic anti-depressants (TCAs) such as nortriptyline, desipramine (secondary amines) and amitriptyline, imipramine (tertiary amines) have been used in chronic neuropathic pain [6]. However, these have been largely replaced due to common side effects such as sedation, anti-cholinergic effects and orthostatic hypotension. Selective serotonin and norepinephrine reuptake inhibitors (SSNRIs) such as duloxetine and venlafaxine have also been used to provide pain relief [7]. Other antidepressants such as SSRIs (citalopram and paroxetine) have also shown efficacy in painful diabetic peripheral neuropathy [8]. However, anticonvulsants including gabapentin and pregabalin have largely replaced the other neuropathic pain attenuating drugs [9,10,11]. Carbamazepine has been used in the management of trigeminal neuralgia. Nevertheless, there is a need to identify more efficacious neuropathic pain attenuating drugs.
Many intensive studies have been conducted previously to explore the myriad targets that can be used to ameliorate the anomalies associated with neuropathic pain. Most of the studies have targeted to inhibit noradrenaline and 5-HT transporters [12], voltage-gated sodium channels (Na(v)1.3, 1.7, 1.8, 1.9) [13], voltage-gated calcium channels (Ca(v)1.2, 2.2, 2.3, 3.1, 3.2, 3.3 and alpha-2-delta-1 subunit) [14], purinergic receptors (P1, P2Y and P2X) [15,16], transient receptor potential (TRP) channels (TRPM8, TRPA1; TRPV1) [17], metabotropic (mGluR1- mGluR5) and ionotropic (NMDA and AMPA) glutamate receptors and glial glutamate transport [18,19]. Many studies have targeted the opening of voltage-gated potassium channels (KATP [Kir6.2/SUR1, Kir6.2/SUR2], KCNQ [K(v) 7.1-K(v) 7.5] and BKCa) [20], GABA receptors and transporters (GAT-1, GAT-3) [21]. Apart from these, many other targets like MAP kinase (ERK, p38 and JNK MAP kinases) [22,23], pro-inflammatory mediators (TNF-α, interleukin-1 and interleukin-6) [24], endocannabinoids (CB1 and CB2 receptors, fatty acid amide hydrolase and transporters) [25], PPAR-γ [26], Na+/Ca2+ exchanger [27], nitric oxide [15], calcitonin gene-related peptide [28] and neuronal nicotinic receptors [29]. The drawback have also been exploited of these targets and lack of effective treatment have forced the scientists to discover new targets that would yield desired results.
In recent years, more extensive research on neuropathic pain has projected new targets that may potentially attenuate neuropathic pain in diverse models. The targets include D-amino acid oxidase [30], endoplasmic reticulum stress receptors [31], sigma receptors [32], ephrins and Eph receptor tyrosine kinase [33], histone deacetylase [34], HCN channels [35], Cdh-1 [36], Wnt/β-catenin [37], Wnt/Ryk [38] and mitochondrial ATPase [39]. Studies conducted on several animal models of neuropathic pain like chronic constriction injury (CCI), spinal nerve ligation (SNL), partial sciatic nerve ligation (PSNL), spinal cord injury (SCI), spared nerve injury (SNI) have revealed a significant role of these targets in attenuation of neuropathic pain and indicate their effectiveness as therapeutic agents. In this review, these novel targets have been discussed, that can prove to be clinically salubrious and provide better pain management. Specific mechanisms and key roles of these new targets in induction of neuropathic pain have been explained. The exploitation of these targets may provide better understanding of mechanisms underlying neuropathic pain and outlines rationale for developing new strategies to improve pain management.
NEW TARGETS IN NEUROPATHIC PAIN TREATMENT
Sigma receptors
Sigma receptors (Sig-Rs) are unique proteins that were first discovered in 1976 [40] and were originally mischaracterized as a new class of opioid receptors. After sigma receptors were tested and cloned, they were found to have no structural or pharmacological similarity to opioid receptors. Biochemical analysis identified two sub-types of sigma receptors: Sig-1Rs (σ1) and Sig-2Rs (σ2) [41]. Sig-1Rs are located at mitochondria-associated endoplasmic reticulum membrane [42] and are widely distributed in heart, liver, immune cells as well as in the nervous system [43]. Numerous studies indicate the role of Sig-1Rs in pain sensitization [44], and hence, they may be beneficial in the pain management, especially neuropathic pain.
There have been studies showing alterations in the number of Sig-1Rs in the injured and neighbouring neurons in response to nerve injury [45]. The significant role of spinal Sig-1Rs in induction of mechanical allodynia has been demonstrated in CCI model in rats, mainly through the activation of spinal NMDA receptors. Intrathecal administration of Sig-1R antagonist, BD1047 (Fig. 1), twice daily from postoperative days 0 to 5 (induction phase of neuropathic pain) attenuated the mechanical allodynia. On the contrary, administration of BD1047 from days 15 to 20 (maintenance phase) did not modulate mechanical allodynia. These results imply that activation of Sig-1Rs on the dorsal horn neurons may trigger, but do not maintain CCI-induced mechanical allodynia and suggest that Sig-1R antagonists may be useful as a pre-emptive analgesic in chronic pain. The antiallodynic effects of Sig-1R antagonist during the induction phase was correlated with the blockade of expression and phosphorylation of NR1 subunit of NMDA receptor, the most essential component of receptor, in the spinal dorsal horn [46].
Fig. 1. Involvement of different targets in the development of neuropathic pain.
The observations from the Sig-1R knockout mice revealed the reduction in wind-up responses (amplification of the nociceptive signals in the spinal cord) in comparison to wild-type mice that had typical wind-up responses in response to sciatic nerve injury. Further, the sensitivity to mechanical and thermal stimuli was significantly attenuated in mice lacking Sig-1Rs. Further, the observations implied that ERK activation was increased in the spinal cords of wild type mice, but no significant changes were observed in Sig-1R knockout mice [47]. Earlier studies had shown that the activation of Sig-1Rs increases the intracellular Ca2+ concentration leading to central sensitization via NMDA receptors [48]. Furthermore, the Ca2+ entry into neurons through NMDA receptors may activate the intracellular ERK signaling [49]. Furthermore, it has been demonstrated that phosphorylation of ERK triggers the development of central sensitization in the spinal dorsal horn neurons to generate and maintain neuropathic pain [50,51]. Based on these results, it has been proposed that activation of Sig-1Rs in response to nerve injury may promote Ca2+ dependent ERK phosphorylation to promote pain sensitization.
It is also demonstrated that Sig-1R antagonist (E-52862) (Fig. 1), dose-dependently inhibits capsaicin-induced mechanical hypersensitivity, formalin-evoked nociceptive behaviours (phase I and phase II), and partial sciatic nerve ligation induced mechanical and thermal hypersensitivity. Furthermore, Sig-1R antagonists abolished wind-up phenomenon in isolated spinal cords of mice in response to electrical stimulation of lumbar dorsal horn. Thus, the electrophysiological as well as the pharmacological data support the involvement of these receptors in pain induction [52]. The role of Sig-1Rs in anti-neoplastic drug (paclitaxel)-induced neuropathy has also been explored in mice. Administration of paclitaxel led to development of cold and mechanical allodynia in wild type mice, without any significant effect in Sig-1R knockout mice. Moreover, s.c. administration of Sig-1R antagonist BD1063, before each paclitaxel dose, completely prevented paclitaxel-evoked cold and mechanical allodynia in Wild type mice. Furthermore, there was an increase in the level of pERK1/2 in the dorsal neurons of the spinal cord ten days after paclitaxel treatment in wild type neuropathic mice, whereas, no significant change in pERK1/2 was observed in Sig-1R knockout mice. Therefore, decreased phosphorylation of ERK after sciatic nerve injury or following paclitaxel administration in Sig-1R knockout mice may be responsible for the marked reduction of cold and mechanical allodynia [53].
Pharmacological blockade or genetic knockout of Sig-1Rs reduces the development of atypical axonal mitochondria in the saphenous nerve myelinated fibers and neuropathic pain after paclitaxel administration. Paclitaxel-induced mitochondrial abnormalities may occur via opening of mitochondrial permeability transition protein (mPTP), after its binding to β-tubulin [54], and/or to bcl-2, which could induce mitochondrial swelling and increase the release of mitochondrial Ca2+ to the cytoplasm [55]. Therefore, Sig-1Rs may possibly modulate bcl-2 proteins to indirectly regulate mPTP opening and mitochondrial swelling, thus, implying the potential role of Sig-1R antagonists in prevention of paclitaxel-induced neuropathic pain [32].
In a CCI model, activation of spinal Sig-1Rs is shown to activate p38 mitogen-activated protein kinase (p38MAPK), which plays a vital role in many chronic pain states including mechanical allodynia [56]. However, early i.t. treatment with the Sig-1R antagonist (BD1047) during the induction phase prevented the increase in p38 MAPK expression in spinal dorsal horn neurons, and attenuated mechanical allodynia [57]. Sig-1Rs have been reported to modulate intracellular Ca2+ signaling and activate Ca2+ dependent enzymes, leading to p38 MAPK activation in the dorsal horn neurons [58]. The facilitatory effects of Sig-1R agonists in pain perception are also mediated through nitric oxide (NO) signaling via neuronal nitric oxide (nNOS) activation [59], which is recognized to be closely associated to p38 MAPK signaling. These findings together indicate that Sig-1Rs can modulate the phosphorylation of p38 MAPK via Ca2+ dependent cascade and/or NO signaling pathway, which is vital for induction of mechanical allodynia.
Intra-hippocampal injections of Sig-1R antagonist, BD1063 (5–50 µg/rat), and Sig-2R antagonist, SM21 (1–5 g/rat) is shown to significantly attenuate agmatine-induced enhancement in thermal hyperalgesia, cold allodynia, mechanical allodynia and TNF-alpha levels. Since, the overproduction of TNF-alpha is associated with development of neuropathic pain [60,61], therefore, it was proposed that Sig-1R and Sig-2R antagonists may attenuate pain by reducing TNF-alpha levels in hippocampus in nerve ligated animals [62].
It has been shown that intrathecal administration of Sig-1R agonist (PRE084) in mice and CCI in rats increases the reactive oxygen species production through NADPH oxidase 2 (Nox2) in the lumbar spinal cord dorsal horn to produce mechanical allodynia and thermal hyperalgesia. Furthermore, intrathecal administration of Sig-1R antagonist (BD1047) (Fig. 1) reduced CCI-induced Nox2 activation (reactive oxygen species generation) and pain behaviour [63] suggesting that sigma receptors may activate free radical production to induce pain. This hypothesis was further supported by the finding showing that the Sig-1R agonists increase the p47 phox expression (the most critical component responsible for Nox2 activation) and Sig-1R antagonist (BD1047) suppresses the p47 phox expression in CCI rats.
The anti-nociceptive actions of selective Sig-1R antagonist has also been linked with the modulation of three key neurotransmitters i.e., glutamate, GABA and nor-adrenaline, in the spinal dorsal horn. Systemic administration of Sig-1R antagonist attenuated formalin-induced flinching and lifting/licking in phase I (initial acute pain phase) and phase II (prolonged tonic pain phase), indicating both spinal and supra-spinal actions. Furthermore, it also attenuated formalin-induced increase in glutamate and decrease in nor-adrenaline levels in the dorsal horns of spinal cord, without altering the GABA levels. Accordingly, it is proposed that Sig-1R antagonists may modulate intracellular Ca2+ ions to facilitate nor-adrenaline release, which may activate spinal alpha2 receptors to attenuate the release of glutamate, leading to their antinociception effects in formalin model [64].
The role of D-serine in the induction of neuropathic pain through activation of Sig-1R in CCI model of neuropathic pain has been explored in mice. After nerve injury, there was an increase in the levels of D-serine and serine-racemase (SR) in astrocytes of the superficial dorsal horn. It is found that SR coexists in the Sig-1Rs expressing astrocytes. Intrathecal administration of BD-1047 attenuated CCI-induced increase in D-serine and SR, and blocked the induction of mechanical allodynia. Moreover, selective blockade of SR by L-serine O-sulfate potassium salt (LSOS) inhibited the development of mechanical allodynia, but not thermal hyperalgesia in CCI mice. Therefore, it was proposed that Sig-1Rs activation was responsible for the increased expressions of D-serine and SR in the astrocytes, affecting dorsal horn neurons that are involved in induction of mechanical allodynia in neuropathic pain [65].
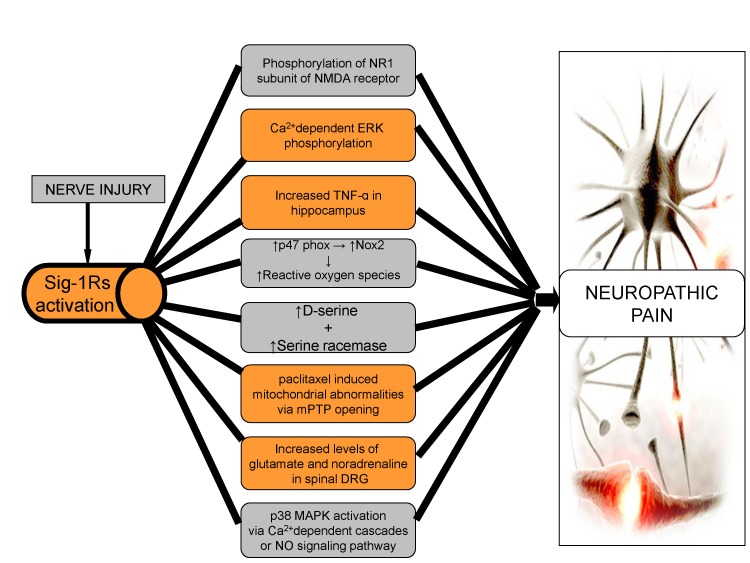
From these extensive sigma receptor-based studies, it may be concluded that Sig-1Rs play a significant role in the induction and maintenance of neuropathic pain through different mechanisms. Sig-1Rs modulate the intracellular Ca2+ entry that leads to the phosphorylation of ERK, NMDA, p38 MAPK and activation of NO signaling, all of which forms the basis for induction of neuropathic pain. Moreover, activation of Nox2 and TNF-alpha through Sig-1Rs, also play a major role in the induction of neuropathic pain by production of reactive oxygen species. Therefore, blocking of Sig-1Rs may result in attenuation of neuropathic pain (Fig. 2).
Fig. 2. Role of sigma receptors in neuropathic pain.
After nerve injury, there is activation of Sig-1Rs, with an increase the intracellular entry of Ca2+, resulting in increased phosphorylation of NMDA, ERK, p38 MAPK and activation of NO signaling leading to neuropathic pain. Increased levels of D-serine, glutamate and nor-adrenaline along with mitochondrial abnormalities via Sig-1Rs are major factors in the induction of neuropathic pain. Production of reactive oxygen species through Nox2 and TNF-alpha, via Sig-1Rs may also contribute to neuropathic pain.
Ephrins and Eph receptor tyrosine kinase
Eph receptor tyrosine kinases and their ligands, ephrins are involved in myriad of developmental aspects, including tissue patterning, angiogenesis, axon guidance and synapse formation [66]. Several Eph and ephrin receptor proteins are expressed in the laminae I-III of spinal dorsal horn and on small and medium sized DRG neurons [67]. EphB receptors and ephrins modulate synaptic activity in the spinal cord, contributing to sensory abnormalities in persistent pain states in NMDA dependent manner [68,69], therefore, suggesting a key role of ephrin and Eph system in physiologic and pathologic pain modulation in the spinal cord level.
L5 spinal nerve injury increases the expression of ephrin B2 (in the neurons of DRG and spinal cord) and Eph B1 isoforms in the neurons of spinal cord. Administration of ephrinB2 siRNA led to reduction in the expression of ephrinB2 and attenuated nerve injury-induced mechanical allodynia. Hence, it may be implied that activation of EphB1/ephrin B2 signaling pathway contribute in neuropathic pain [70]. There is a correlation between development of hyperalgesia and increase in the expression of ephrinB1 and EphB receptor proteins in DRG neurons, dorsal horn and IB4 positive nociceptive terminals in CCI and dorsal rhizotomoy (DR) model. After nerve injury the activation and redistribution of ephrinB-EphB in DRG and dorsal horn contribute to neuropathic pain. Intrathecal administration of EphB-receptor antagonists (EphB1-Fc and EphB2-Fc chimeras) was shown to suppress the induction and maintenance of nerve injury-induced mechanical allodynia and thermal hyperalgesia. Moreover, EphB antagonists also prevented nerve injury-induced hyper-excitability of nociceptive small DRG neurons, sensitization of dorsal horns neurons and LTP of synapses between C fibers and dorsal horn neurons. Furthermore, intrathecal injection of EphB-receptor activators (ephrinB1-Fc and ephrinB2-Fc), in uninjured animals, induced the thermal hypersensitivity and reduced the threshold for LTP. Accordingly, the up-regulation of ephrinB1 and EphB1 receptor proteins after nerve injury may increase the excitability of nociceptive related neurons and synaptic plasticity at spinal level, leading to induction of neuropathic pain [71].
The ephrin-B2 conditional knockout (CKO) mice, with deletion of ephrin-B2 from Nav 1.8-expressing nociceptors, demonstrated the reduction in pain behavior in different models of pain. Furthermore, there was significant decrease in tyrosine phosphorylation of NMDA receptor subunit NR2B in the dorsal horn suggesting that ephrin-B2 signaling plays a vital role in regulating pain thresholds, with its mechanisms associated with NMDA receptor phosphorylation [72]. It is demonstrated that the activation of MAPKs modulates the spinal nociceptive information through ephrinBs/EphBs signaling in CCI and formalin induced mice models of neuropathic pain. Intrathecal injection of ephrinB1-Fc produced a dose-dependent thermal hyperalgesia and mechanical allodynia, along with an increase in the expression of spinal c-Fos and p-MAPKs. The activated forms of p38 and JNK were localized in the spinal neurons and astrocytes, while p-ERK was localized in the spinal neurons. Inhibition of spinal MAPK was observed to reverse the pain behavior and prevent ephrinB1-Fc-induced hyperalgesia and spinal Fos protein expression. The blockade of EphB receptors alleviated formalin and CCI induced pain along with attenuation of spinal MAPKs and c-Fos protein activation Moreover, pre-treatment with NMDA receptor antagonist (MK-801), suppressed ephrinB1-Fc induced hyperalgesia and activation of spinal MAPKs. Therefore, it can be implied that ephrinsB1-Fc leads to activation of MAPK pathways through NMDA receptors to induce pain behavior [73].
The role of phosphatidylinositol 3-kinase (PI3K), as a downstream effector in the modulation of spinal nociceptive information, in relation to ephrinBs and EphBs in formalin and CCI-induced inflammation and neuropathic pain has been shown in mice. Intrathecal injection of ephrinB1-Fc is shown to induce mechanical allodynia and thermal hyperalgesia, increase spinal c-Fos and PI3Kp110γ expression and phosphorylate AKT (p-AKT), a downstream target of PI3K. Observations suggested that pre-treatment with wortmannin, a PI3K inhibitor, prevented ephrinB1-Fc induced activation of AKT, spinal c-Fos protein expression and reversed the pain behaviors. Similarly, blockade of spinal EphBs receptors suppressed formalin and CCI-induced inflammation and neuropathic pain behaviors by reducing the levels of spinal PI3K, c-Fos expression and reducing the phosphorylation of AKT. Therefore, it can be implied that PI3K has a significant role in modulation of nociceptive information related to ephrinsBs and EphBs via ERKs and EphBs via ERK activation [74].
The role of protein kinase C-γ (PKCγ) as a downstream effector in regulation of spinal pain processing via ephrinB-EphB signaling has been shown in various mice models of neuropathic pain. Observations indicated that intrathecal injection of EphB receptor activator (ephrinB2-Fc) induced mechanical allodynia and thermal hyperalgesia, along with the increase in the expression of spinal PKCγ. In spinal PKCγ knockout mice, there was no ephrinB2-Fc induced pain behavior. Moreover, intrathecal injection of EphB receptor blocker (EphB2-Fc) led to suppression of formalin-induced inflammatory, CCI induced neuropathic pain, tumor cell implantation (TCI)-induced bone cancer pain behaviours. Moreover it also decreased the activation of spinal PKCγ. Intrathecal injection of NMDA receptor blocker, (MK801), also suppressed ephrinB2-Fc-induced spinal PKCγ activation and pain behavior, confirming the key role of PKCγ in spinal pain processing through ephrinB-EphB signaling [75].
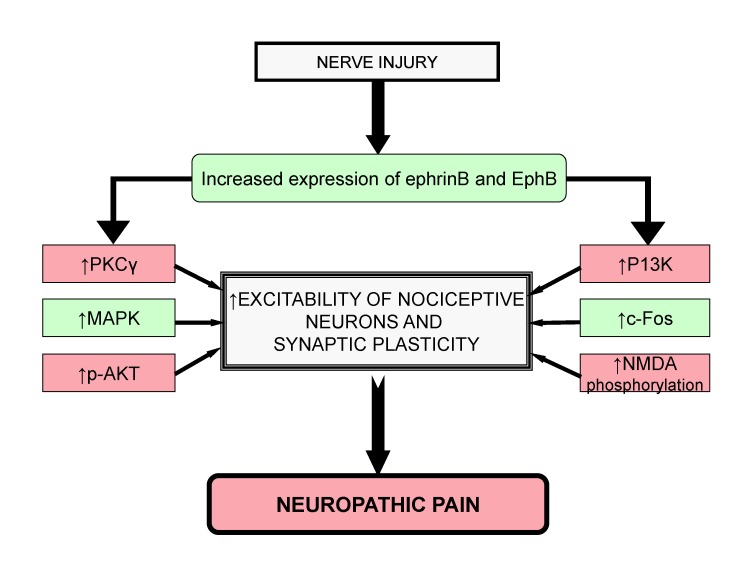
From above studies, it can be concluded that an increase in EphrinBs/EphBs signaling leads to increase in activation of PKCγ, MAPK, c-Fos, p-AKT, P13K and phosphorylation of NMDA. All these factors are responsible for increased excitability of nociceptive neurons and synaptic plasticity, which are fundamental mechanisms leading to induction of neuropathic pain (Fig. 3).
Fig. 3. Role of Ephrins and EphB receptor tyrosine kinase leads in neuropathic pain.
After nerve injury, the increased levels of PKCγ, MAPK, c-Fos, p-AKT, P13K and NMDA phosphorylation through ephrinB and EphB signaling lead to increased excitability of nociceptive neurons and synaptic plasticity that contributes to neuropathic pain.
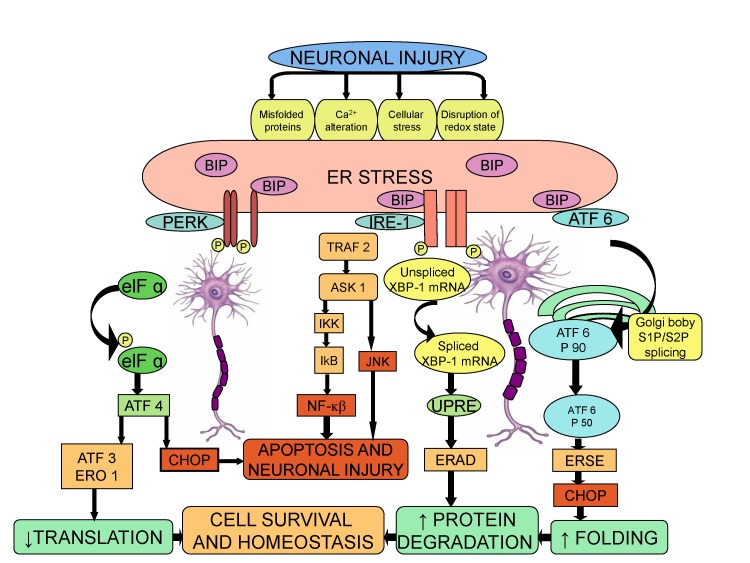
Endoplasmic reticulum stress (ERS) receptors
In a number of pathological conditions like glucose deprivation, depletion of calcium stores, exposure to free radicals and accumulation of unfolded proteins, there is disruption of the proper functioning of ER and thereby, causing ER stress, which severely impairs the protein folding [76,77]. The cells react to ER stress by increasing the expression of molecular chaperone such as Binding Immunoglobulin Proteins BIP (GRP 78), which initiates a defensive process called Unfold Protein Response (UPR) [78]. The transcriptional activation of BIP is used as a marker of UPR initiation [77]. The UPR is mediated by three ER stress receptors: PKR-like ER kinase (PERK), inositol-requiring enzyme 1 (IRE1), and the activating transcription factor-6 (ATF6) [79]. Studies suggest that ER stress response is a key reaction in inflammatory diseases, including neuroinflammation [80]. The signaling pathway between ER stress and neuroinflammatory response is connected through several mechanisms, including reactive oxygen species, calcium, nuclear factor-κB (NK-κB), and mitogen-activated protein kinase (MAPK) [81]. The pro-inflammatory substances trigger the ER stress response, which in turn may contribute in the development of neuropathic pain [82,83].
The role of ER stress response in neuropathic pain has been demonstrated in a Complete Freund's Adjuvant (CFA) injected rat model of orofacial inflammatory pain. The protein and mRNA levels of ER stress response genes, BIP (GRP78), p-eIF2α and ATF4 were significantly increased in the trigeminal ganglion (TG). The expression of BIP (GRP78) was increased in all sized TG neurons, while the p-eIF2α expression was increased in small and medium sized neurons. Administration of ER stress modulator, salubrinal, into TG for 5 days following CFA injection, attenuated heat hyperalgesia suggesting that induction of ER stress response in the primary sensory neurons is responsible for orofacial inflammation and pain [84]. The role of ER stress and UPR was examined in L5 spinal nerve ligation (SNL)-induced mirror-image neuropathic pain in rats. Nerve ligation led to activation of BIP (GRP 78) followed by activation of IRE-XBP1 and ATF6 pathways, but not PERK-e1F2 pathway. Accordingly, the increased levels of BIP in the dorsal horn indicate the induction of ER stress in response to neuronal injury. The increased level of spliced XBP-1 in the dorsal horn is a result of activation of IRE-1, as activation of IRE-1 induces the splicing of XBP-1 mRNA via cleavage of its intron [85]. Furthermore, it is also well documented that the spliced XBP-1 functions as a transcription factor for ER stress related genes and may be critical in initiating the ER stress response [86]. The activation of ATF6 pathway is mediated through BIP, which cleaves it from ER membrane and translocates it to the Golgi complex, followed by the transcription of UPR target genes by the cleaved 50-kDa product of ATF-6 fragment [87]. The intrathecal injection of siRNA for ATF-6 attenuated the neuropathic pain, again emphasizing the cardinal role of ER stress in the induction of neuropathic pain [83].
The role of epoxy fatty acids (EpFAs) and ER stress-regulated response in diabetes-induced neuropathic pain has been investigated. Since, soluble epoxide hydrolase (sEH) degrades EpFAs, the natural analgesic mediators; therefore, blocking of sEH produces analgesic actions. The precise mechanisms involved in analgesic effects of EpFAs are unknown; however, it has been postulated that naloxone antagonizes analgesic effects of these fatty acids suggesting the possible role of opioids in producing anti nociceptive effects. Inhibitors of sEH reduced ER stress markers and neuropathic pain and it also suggested that EpFAs are upstream modulators of ER stress pathways [88].
Taken together, the results imply a major role of ER stress pathways in regulating the excitability of nociceptive system and inflammatory pain in peripheral nervous system. Although, during cellular stress the main goal of UPR pathway is to promote cell survival, yet, the continuous and persistent activation of ER stress response may render the spinal neurons vulnerable to neuronal injury in response to neuropathic pain stimuli (Fig. 4).
Fig. 4. Role of ER stress in induction of neuropathic pain.
Activation of ER stress receptors including PERK, ATF-6 and IRE-1, tend to promote cell survival during nerve injury. However, persistent activation of ER stress response leads to neuronal injury and ultimately neuropathic pain.
β-Catenin, Wnt/Ryk and Wnt/β-catenin
β-catenin is a subunit of cadherin protein complex, localized to synaptic contacts, and is associated with synapse formation and neuronal circuit assembly during development [89]. Wnts belong to the family of glycoproteins and play a major role in many aspects of CNS development such as neural induction, cell proliferation, neuronal migration, axon guidance, dendritic arborization and synaptogenesis [90]. Ryk, a trans-membrane protein receptor of tyrosine kinase, is required for normal axon guidance and neuronal differentiation [91] and it binds with Wnt to modulate its activity [92]. Menin (MEN I), a transcription factor product of multiple endocrine neoplasia type I, is a tumor suppressor gene [93] that is localized to the nucleus and is also critical mediator of synapse formation between neurons. Moreover, menin has an essential role in Wnt/β-catenin signaling through histone methylation of downstream target gene promoters [94]. The Wnt/β-catenin pathway, a canonical Wnt signaling pathway, has a significant role in neural development, axonal guidance, neuropathic pain remission and neuronal survival [95]. β-catenin, Wnt/Ryk and Wnt/β-catenin pathways are explored as a therapeutic targets for treating neuropathic pain.
There is an increase in the expression of β-catenin and menin in the ipsilateral spinal dorsal horn of rats in response to spared nerve injury (SNI), which is associated with development of mechanical hypersensitivity. It is possible that menin may induce the formation of new synapses and sprout Aβ-fibers from lamina III to lamina II of dorsal horn and these changes may contribute in the induction of neuropathic pain [96]. An increase in expression of Wnt3a, a prototypic Wnt ligand of Wnt/β-catenin pathway, in the dorsal horn of spinal cord after partial sciatic nerve ligation (PSL) has also been reported. Intrathecal administration of XAV939, a Wnt/β-catenin signaling inhibitor, effectively attenuated the induction of neuropathic pain and microglial activation. Furthermore, intrathecal treatment with Wnt3a in the lumbar spinal regions of naive animals stimulated the development of allodynia and triggered the release of brain-derived neuropathic factor (BDNF) from microglial cells. Hence, it may be possible that up-regulation of Wnt3a in the dorsal horn activates the microglial cells to secrete BDNF, which is responsible for neuropathic pain induction [97].
An increase in the expression of Wnts in the DRG and spinal cord and activation of Wnt/Frizzled/β-catenin signaling in the spinal cord in CCI model and tumor cell implantation (TCI)-induced bone cancer in mice model has been reported. Wnt signaling enhanced the production of pro-inflammatory cytokines, which led to induction of neuropathic pain. It was found that Wnt inhibitors attenuate mechanical allodynia and thermal hyperalgesia in neuropathic pain models suggesting the critical role of Wnts in induction of neuropathic pain [88]. An increase in expression of Wnt3a, Wnt5b and Ryk receptors in the primary sensory neurons, dorsal horn neurons and astrocytes has been observed after sciatic nerve injury. Inhibition of Wnt/Ryk receptor signaling led to blockade of neuropathic pain without any significant effect on normal pain sensitivity and locomotor activity. In vivo and in vitro blockade of Ryk receptors with anti-Ryk antibody suppressed nerve injury-induced increase in intracellular Ca2+, sensory neuronal hyper-excitability, enhanced plasticity of synapses between afferent C-fibers and dorsal horn neurons, implying that Wnt/Ryk signaling may be a key mechanism underlying the pathogenesis of neuropathic pain [98].
The neuroprotective mechanism of rapamycin in spinal cord injury in rats has been correlated with an increase in expression levels of β-catenin and BDNF. Accordingly, it may be proposed that rapamycin reduces neuronal injury by inhibiting the apoptosis of neurons, and increasing the expression of BDNF, via activation of Wnt/β-catenin pathway [90]. It has been shown that nerve injury increases the levels of TCF4, β-catenin and GSK-3β within the neurons of DRG and spinal cord. Furthermore, intrathecal injection of Wnt/β-catenin inhibitor (IWR-1-endo) and TCF4 small interfering RNA (siRNA) attenuated CCI-induced mechanical allodynia and thermal hyperalgesia and reduced the expression of β-catenin and GSK-3β. Thus, it may be suggested that TCF4 in DRG and spinal cord may be involved in maintenance of CCI-induced neuropathic pain through Wnt/β-catenin signaling pathway [99].
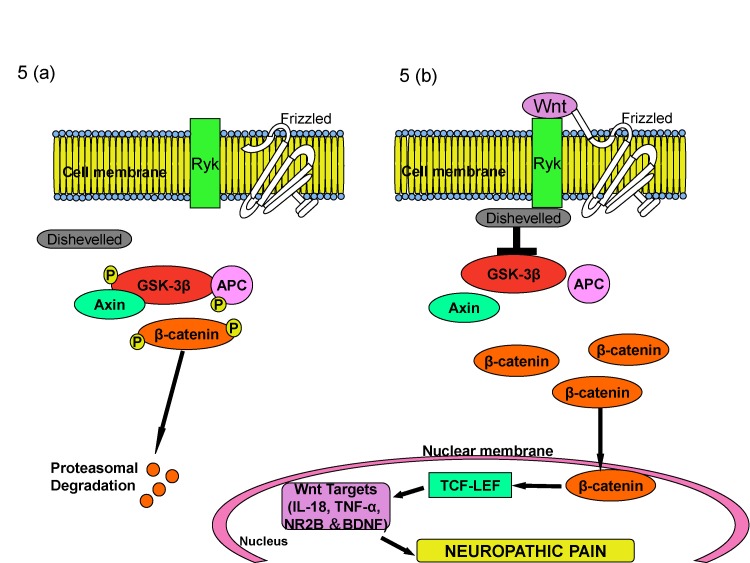
Based on these studies, it may be proposed that Wnt/β-catenin along with Wnt/ryk signaling plays a critical role in induction of neuropathic pain, either through production of pro-inflammatory cytokines or through secretion of BDNF from the microglial cells. The binding of Wnt to its receptor suppresses the GSK-3β phosphorylation of β-catenin, which on accumulation binds to TCF4 and leads to activation of Wnt target genes, causing neuropathic pain (Fig. 5).
Fig. 5. Role of β-catenin system in induction of neuropathic pain.
In the physiological state, absence of Wnt leads to decreased levels of β-catenin in the cytoplasm as GSK-3b phosphorylates b-catenin and leads to its proteosomal degradation (A). During the nerve injury, Wnt binds to its receptor frizzled and suppresses the GSK-3β phosphorylation of β-catenin. Increased β-catenin binds to TCF4 and activates Wnt target genes that are responsible for neuropathic pain (B).
Hyperpolarization-activated cyclic nucleotide-gated cation channels (HCN)
Hyperpolarization-activated and cyclic nucleotide-gated (HCN) channels are non-selective, ligand-gated cation channels [100] and are present in the cells of heart and central nervous system [101]. HCN channels are encoded by four genes (HCN1, HCN2, HCN3, HCN4), and the activation of these channels generates inward currents during hyperpolarization membrane potential. The physiological functions of these channels include normalization of synaptic inputs, regulation of resting membrane potential and modulation of intrinsic cellular frequency characteristics [102]. Various studies conducted on HCN channels imply their significant role in induction of neuropathic pain [103,104].
It is reported that the spinal HCN channels at the primary afferent terminals contribute to chronic pain in formalin and SNL-induced neuropathic pain models in mice. Intra-peritoneal and intrathecal administration of eugenol reversed peripheral nerve injury induced mechanical allodynia in trigeminal neurons by inhibition of HCN channels. Eugenol attenuates CCI of infraorbital nerve-induced mechanical allodynia and inhibits HCN current with IC50 of 157 µM in trigeminal ganglion neurons. Furthermore, eugenol induced inhibition of HCN current was diminished by increase in intracellular cAMP levels [104].
It has been reported that the genetic deletion of HCN2 diminishes cAMP sensitive component causing inward current and suppresses the action potential firing caused by elevation of cAMP levels in nociceptors. The deletion of HCN2 specifically in Nav 1.8 expressing nociceptors showed normal pain threshold in neuropathic pain mice, indicating a vital role of HCN2-driven action potential firing expressed in Nav 1.8 nociceptors [103]. The impact of changes to ventral-lateral periaqueductal gray (vIPAG) HCN channels on the neural activity in CCI model of neuropathic pain has also been reported. An increase in expression of HCN1 and HCN2 channels, augmentation of hyperpolarization-activated current amplitudes to more positive potentials and increase in action potential firing following CCI has been reported. Forskolin, which elevates intracellular cAMP, mimics CCI-induced changes in neuronal excitability in vIPAG. Furthermore, ZD7288, a HCN blocker, attenuated spontaneous EPSCs and reversed the effects of forskolin [105].
Ivabradine, an anti-anginal agent, attenuates pain in different models of inflammatory and neuropathic pain through HCN ion channels. Ivabradine blocks HCN channels, expressed on the small sensory neurons, and suppresses the action potential firing in nociceptive neurons by increasing the intracellular cAMP [106]. A significant increase in HCN2-immunoreactivity in small (<30 µm) DRG neurons (specifically in IB-4 negative neurons) has been observed in L5 spinal nerve axotomy model in rats. Furthermore, intra-plantar treatment with ZD7288 (100 µM) was shown to decrease mechanical pain behavior [107]. Pulsed Radio-Frequency treatment (PRF) is shown to decrease thermal hyperalgesia, mechanical allodynia and mechanical hyperalgesia along with an increase in the levels of HCN1 and HCN2 in DRG in CCI model [97].
The dysfunction of HCN channels in the pyramidal neurons of the medial Pre-frontal Cortex (mPFC) has also been reported in SNI model in rats. Hyper-polarizing shift in the SNI neurons was observed in the II/III pyramidal neurons of the contralateral mPFC. Furthermore, it was found that hyperpolarization shift was abolished by intracellular treatment with bromo-cAMP. Acute HCN blockade by local injection of ZD7288 in mPFC of SNI rats suppressed cold allodynia indicating that changes in the cAMP/Protein kinase A axis in mPFC neurons may be responsible for alterations in HCN channel function, which may further influence the descending inhibition of pain pathways in neuropathic pain [108].
Thus, it may be concluded that in response to nerve injury, an increase in intracellular cAMP level leads to action potential firing that increases the expression of HCN in DRG neurons and an increase in HCN expression is responsible for the induction of neuropathic pain.
D-Amino acid oxidase (DAAO)
Studies conducted in animal models of neuropathic pain have suggested that spinal DAAO, restricted within the astrocytes [109,110], plays a pronociceptive role and might be a potential target for treatment of neuropathic pain [72]. DAAO is a peroxisomal enzyme that catalyzes the oxidative deamination of polar and neutral D-amino acids to α-keto acids, ammonia and hydrogen peroxide [109]. In the CNS, D-amino acid oxidase is confined to the lower brain stem, cerebellum and spinal cord, with lower levels present in the mid brain, cortex and hippocampus [111].
The potential role of DAAO in neuropathic pain in a rat model of L5/L6 spinal nerve ligation has been investigated. Nerve ligation led to increase in mRNA expression and enzyme activity of DAAO in the lumbar spinal cord. The systemic injection of DAAO inhibitor, sodium benzoate, specifically blocked neuropathic pain by blocking the DAAO activity in the lumbar enlargement of spinal cord. Direct intrathecal injection of sodium benzoate (30 µg/rat) specifically reduced spinal nerve ligation-induced neuropathic pain. Furthermore, systemic and intrathecal administration of sodium benzoate blocked formalin-induced hyperalgesia and spinal nerve ligation induced neuropathic pain to an equal extent [72]. Study using small interference RNA (siRNA) has suggested that the down regulation of spinal DAAO expression and enzymatic activity leads to analgesia with its mechanism potentially related to inhibition of astrocytes in the spinal cord. Multiple daily intrathecal injections of siRNA for DAAO (30 µl/day) markedly inhibited spinal DAAO gene and protein expressions, DAAO enzymatic activity, expression of glial fibrillary acidic protein (GFAP), a biomarker of astrocytes activation and formalin-induced tonic phase pain in rats [30]. In another study, DAAO inhibitor, 5-chloro-benzo[d]isoxazol-3-ol (CBIO) was shown to block formalin-induced tonic phase pain and spinal hydrogen peroxide levels, suggesting that spinal DAAO produces algesia via production of hydrogen peroxide [112]. Hydrogen peroxide, most likely derived from the spinal astrocytes [113], is an active and stable reactive oxygen species that is produced form the oxidation of D-amino acids by DAAO [110,113], Hydrogen peroxide may be involved in induction of pain either directly or indirectly through N-methyl-D-aspartate (NMDA) receptor activation [98].
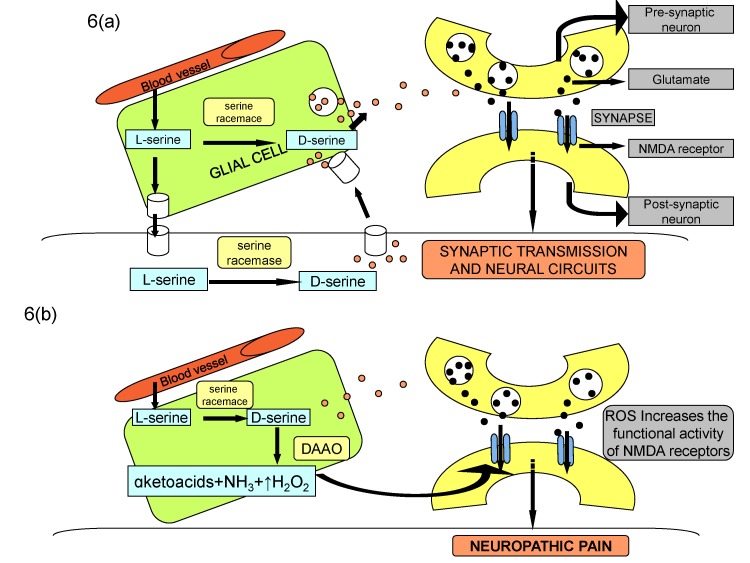
Therefore, it is plausible to suggest that nerve injury or toxic chemical may increase the expression as well as the activity of DAAO in the spinal cord to activate the central astrocytes, which may increase the production of reactive oxygen species. The latter in turn directly or indirectly through increase in phosphorylation of NMDA receptors may induce neuropathic pain (Fig. 6).
Fig. 6. NMDA-mediated synaptic transmission during physiological state (A) and nerve injury state (B).
Binding of glutamate and co-agonist D-serine to NMDA receptor subunit modulates synaptic transmission and plasticity in normal state. Increase in DAAO activity after nerve injury decreases the levels of D-serine, which may indirectly increase the synthesis of reactive oxygen species to induce neuropathic pain through increased NMDA phosphorylation and consequent enhanced synaptic plasticity.
Histone deacetylase
Histone deacetylase enzymes (HDAC) along with histone acetyl-transferases (HATs) control the process of acetylation of histone lysine residues, such as lysine residue9 (H3K9ac), which further modulates the expression of transcription factors [114] and also promotes transcriptional elongation. Histone acetylation is one of the epigenetic mechanisms that is hypothesized to be involved in induction of neuropathic pain, with its causes primarily rooted in altered transcriptional expression. There has been an increase the expression of histone deacetylase enzymes following nerve injury or inflammatory conditions that induce deacetylation of histone proteins and histone deacetylase inhibitors attenuate neuropathic pain in neuropathic and inflammatory pain [34].
There is an increase in expression of histone deacetylase 4 in response to spinal nerve ligation in rats and inhibition of histone deacetylase 4, using LMK 235, prevented development of allodynia [115]. In spinal nerve ligation model, an increase in histone deacetylase 1 and decrease in histone (H3) acetylation has been documented. Treatment with baicalin (an anti-inflammatory flavonoid) significantly attenuated deacetylase 1 expression and reversed pain sensitivity [116]. A study from our laboratory documented neuropathic pain attenuating potential of histone deacetylase inhibitor (sodium butyrate) in CCI model in rats [117]. Administration of another histone deacetylase inhibitor (trichostatin A) has been shown to suppress inflammatory pain symptoms [112]. There have been other studies showing that histone deacetylase inhibitors such as valproic acid [118], MS-275 and suberoylanilide hydroxamic acid reduce the nociceptive response [119]. Administration of curcumin has been shown to attenuate pain in formalin model along with hypo-acetylation of histones H3 and H4 in dorsal root ganglia. Furthermore, pretreatment with histone deacetylase inhibitor, suberoylanilide hydroxamic acid, enhanced the analgesic activity of glutamate agonist (LY379268) proposing the potential of histone acetylation to attenuate pain [120]. A recent study has also shown an increase in expression of histone deacetylase 1 in microglia and astrocytes in the dorsal horn neurons in response to nerve injury suggesting that increase in histone deacetylase in the astrocytes may be a key factor in inducing pain [121]. Another study has shown an increase in expression of histone deacetylase 2 specifically in astrocytes, with no significant change in neurons of dorsal horn in nerve injury model. The mechanisms responsible for histone hypoacetylation-induced pain include decrease in metabotropic glutamate receptors in the DRG and spinal cord [120]; increase in cytokines [117]; decrease in glutamate transporters [118]; down-regulation of mu-opioid receptors [122] and decrease in glutamic acid decarboxylase 65 expression, leading to decrease in synaptic GABAergic inhibition [123].
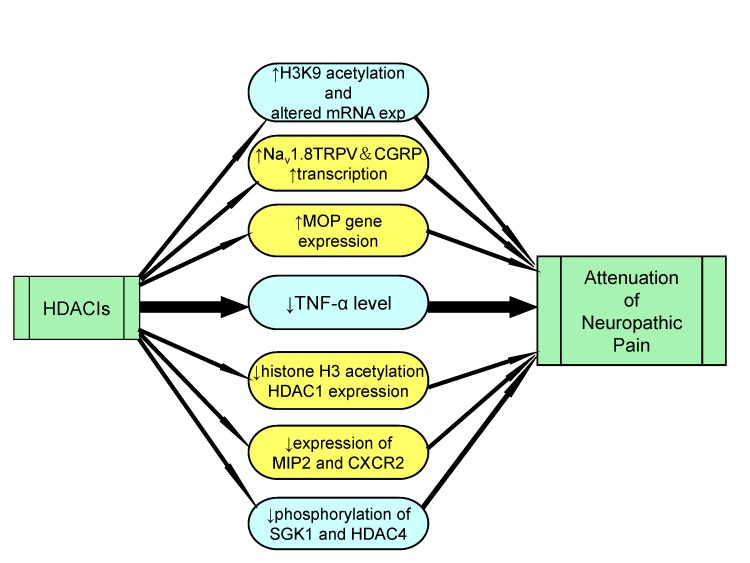
Therefore, it may be proposed that nerve injury produces epigenetic changes due to activation of histone deacetylase enzymes, which may decrease histone acetylation to induce pain and histone deacetylase inhibitors may be employed to inhibit neuropathic pain (Fig. 7).
Fig. 7. Role of HDAC inhibitors in attenuation of neuropathic pain.
Histone deacetylase inhibitors helps in management of neuropathic pain by increasing the acetylation of H3K9, transcription of Nav 1.8, TRPV and CGRP and increasing expression of MOP genes. HDACIs also result in decreased production of inflammatory mediators, reduction of histone H3 acetylation and reduced phosphorylation of SGK1 and HDAC4.
Mitochondrial ATPase
Mitochondria, a powerhouse of cell, play a major role in energy production, cellular signaling, apoptosis, ROS production, and calcium homeostasis [124]. Both mitochondrial and bioenergetic dysfunction is assumed to play a significant role in induction of neuropathic pain [39]. It has been shown that chemotherapeutic agents like paclitaxel and oxaliplatin lead to nitration of superoxide anion in the mitochondria to form peroxynitrite. It may be possible that during nerve injury, formation of peroxynitrite may damage the mitochondria and decrease the production of ATP, which may contribute in induction of neuropathic pain [125]. Another study demonstrates the role of mitochondrial ATP synthase in DRG after sciatic nerve injury in adult rats. Immunohistochemical and Western Blotting studies showed the decreased expression of mitochondrial ATP synthase in L4-L5 DRG neurons in the un-myelinated C-fibers and thinly myelinated Aδ fibers, suggesting the decreased ATP production. The most cardinal observation was that the intrathecal ATP injection reduced thermal and mechanical hyperalgesia after nerve injury [126]. It is important to understand that ATP is not an energy product; rather it may also act on specific membrane receptors to modulate pain transmission [127].
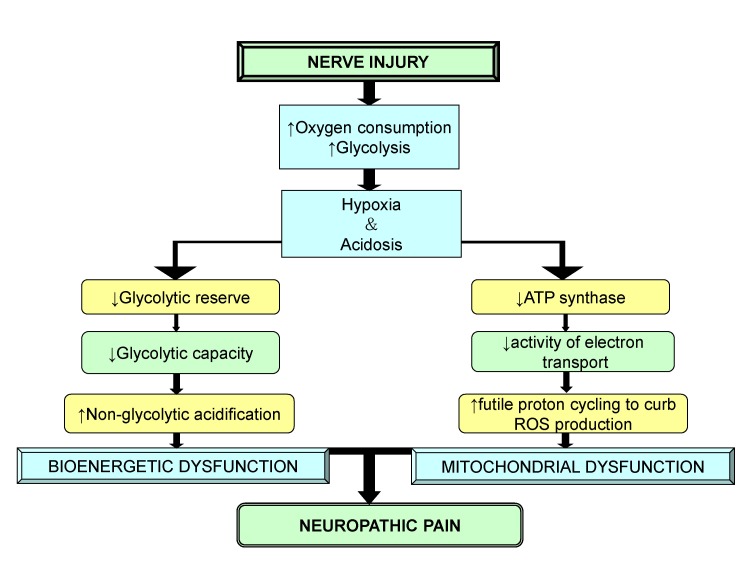
It has been shown that oxygen consumption, which is vital for ATP synthase activity is significantly reduced in injured nerves in response to partial sciatic nerve ligation (PSNL) in mice. Nerve injury led to increase in the number of immune cells that contributed to neuroinflammation and increased the oxygen demand. Therefore, the development of hypoxia (due to increased oxygen demand) further reduced the ability of mitochondria to carry out oxidative phosphorylation, which may be responsible for decrease in the maximal respiratory capacity of injured nerves. An increase in the number of immune cells was also responsible for increased glycolysis and lactic acidosis, which lead to development of tissue acidosis [39]. Tissue acidosis has been known to cause constant ongoing pain [128].
Therefore, it is concluded that after nerve injury, the increased oxygen consumption and glycolysis leads to hypoxia and acidosis, which trigger other anomalies responsible for mitochondrial and bioenergetic dysfunction. The decreased energy production associated with mitochondrial dysfunction reduces Na+/K+ATPase activity, which is responsible for membrane hyper-excitability. It is thus, vital to protect mitochondria to ameliorate the symptoms of neuropathic pain (Fig. 8).
Fig. 8. Role of mitochondrial and bioenergetic dysfunction in neuropathic pain.
After nerve injury, an increase in oxygen consumption result in hypoxia, acidosis, decreased glycolytic reserve and decrease in energy production that leads to mitochondrial and bioenergetic dysfunction causing neuropathic pain.
Cdh-1, a co-activator subunit of anaphase-promoting complex/cyclosome (APC/C)
Cdh-1 is a tumor suppressor gene that belongs to cadherin super family [129]. It leads to production of calcium-dependent cell-cell adhesion glycoprotein and several reports indicate the role of Cdh-1 in induction of neuropathic pain [130]. Anaphase-promoting complex/cyclosome (APC/C) and Cdh-1 are linked to various neurobiological functions, and the most vital is the regulation of synaptic differentiation and transmission [131]. It has been reported that APC/C-Cdh1 mediates synaptic plasticity through an EphA4-dependent signaling pathway in cortical neurons [132] and in anterior cingulate cortex (ACC), that is a major cortical area involved in processing pain related emotion and transmission of pain sensation [133]. In spared nerve injury (SNI) model, up-regulation of c-Fos in ACC was demonstrated suggesting the induction of central sensitization. A significant decrease in nuclear export of Cdh-1 after SNI was also observed, suggesting the decreased APC/C-Cdh1 activity in the ACC. The decreased APC/C-Cdh-1 activity in ACC contributed to increase in GluR1 subunits of α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptors leading to up-regulation of synaptic activity. Furthermore, swollen myelinated fiber and collapsed axons were detected in neuronal cells in ACC, probably due to AMPA receptor trafficking-induced excitotoxicity. Micro-injection of Cdh-1 expressing recombinant lentivirus in ACC alleviated SNI-induced mechanical allodynia, normalized redistribution of GluR1 subunits of AMPA receptors and synaptic ultra-structure in ACC [134].
Hence, it may be insinuated that nerve injury decreases the expression of Cdh-1 in ACC, which in turn may increase the expression of AMPA receptor to induce neuropathic pain.
DISCUSSION
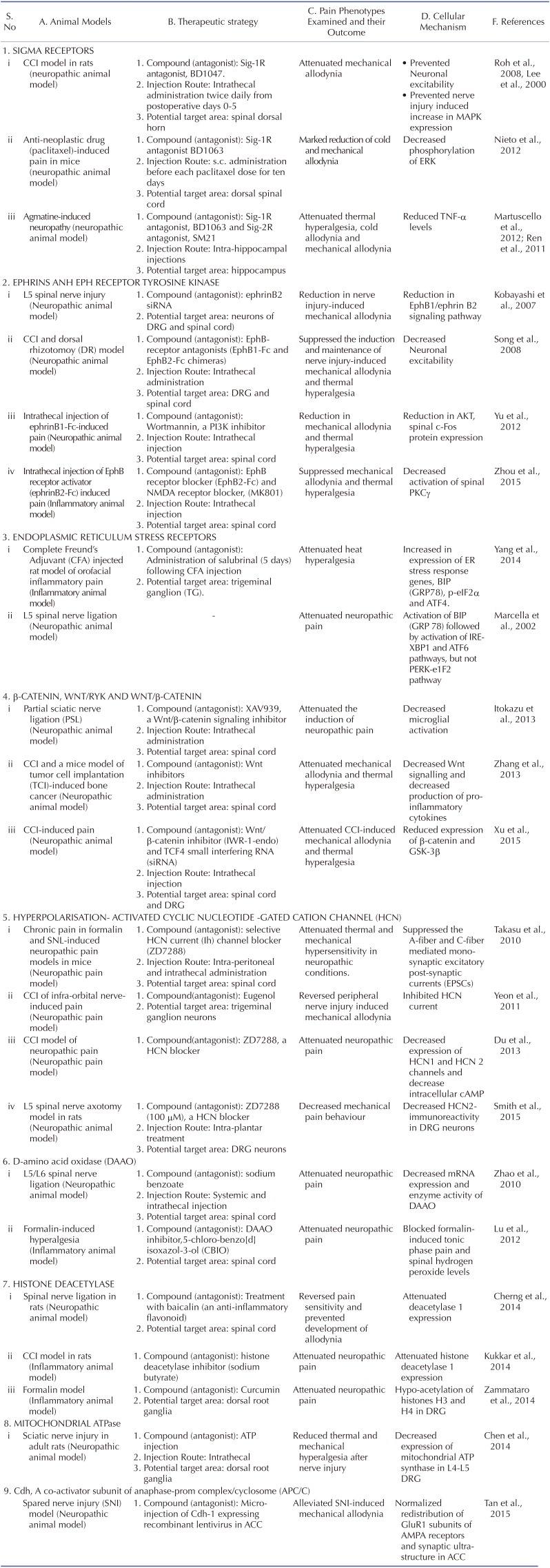
There have been extensive studies in recent years to explore the efficacy of new targets in management of neuropathic pain (Table 1). These studies have been largely done in well established animal models that share clinical features of nerve injury such as CCI (correlated to carpal tunnel syndrome), spinal nerve injury, CFA-induced orofacial inflammatory pain (trigeminal neuralgia) and anticancer drugs-induced neuropathic pain. These models possess face validity, constructive validity and predictive validity. Based on these studies, it is possible that there may be activation of myriad of reactions in response to nerve injury that may interconnect to induce central sensitization. Although, a number of different targets have been projected as clinically potentially targets, yet the studies describing the interrelation among these targets are lacking. Most of the studies have targeted the preventive treatment before the development of neuropathic pain (i.e induction phase) [52,63,71,74,84]. However, there have been very few studies documenting the influence of modulators of these targets in the maintenance phase of neuropathic pain i.e once the pain is already established. The study of Roh et al demonstrated the ineffectiveness of pharmacological modulator of sigma receptor antagonist in the maintenance phase of neuropathic pain [46]. Nevertheless, more elaborative studies are required to explore the role and understand mechanisms of these new targets in maintenance phase of neuropathic pain.
Table 1. Summarized findings related to new targets in neuropathic pain.
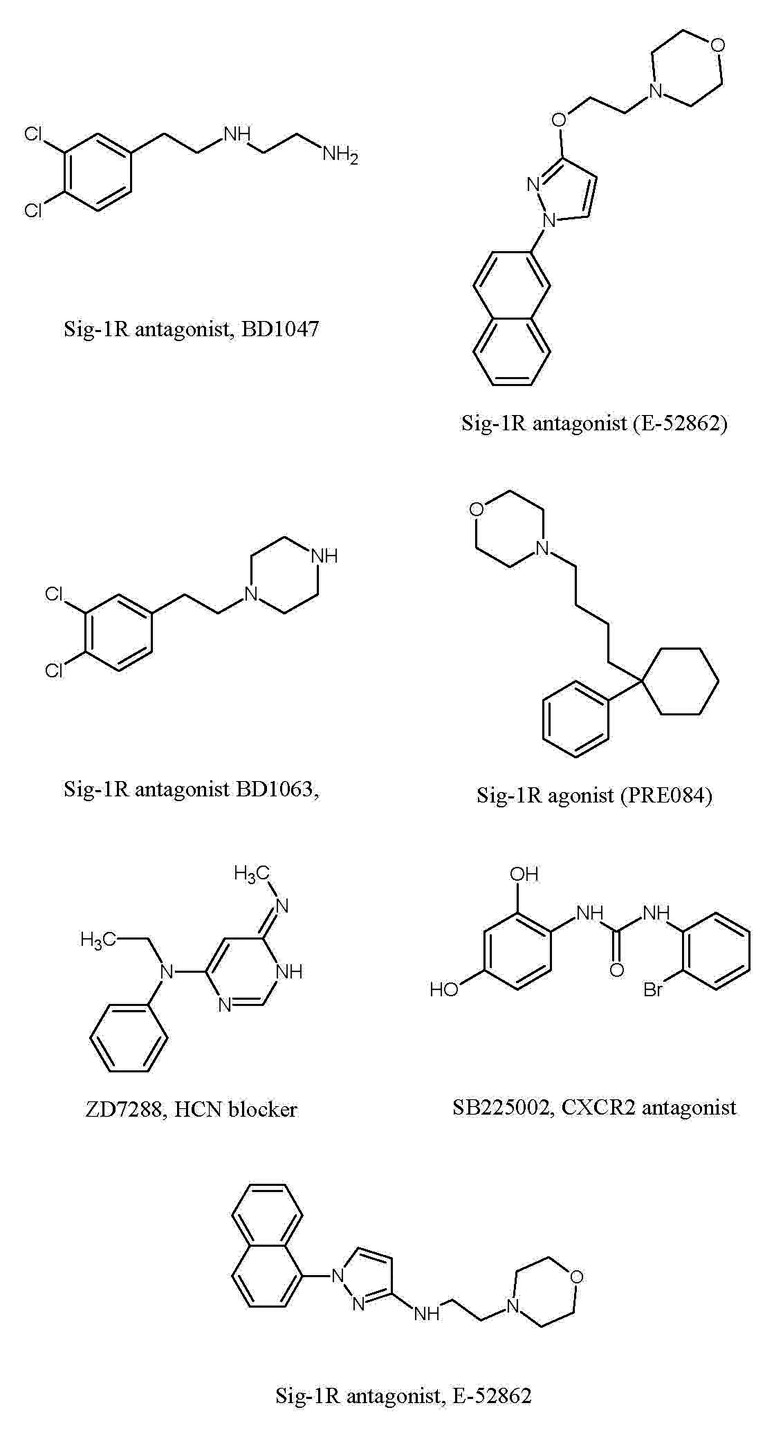
Research pertaining to these targets explores their individual roles in the disease, but close scrutiny of their mechanisms imply a significant correlation between these targets. It is possible that nerve injury may produce epigenetic changes such as histone deacetylation that may trigger the production of inflammatory mediators [34]. The activation of sigma receptors may also contribute in increasing cytokine production [62]. These increased levels of cytokines and free radicals, due to sigma receptor activation [63] and increased activity of DAAO [72,135], may induce ER stress [83] which in turn may induce central sensitization. The development of neuroinflammation may also increase oxygen consumption and produce local hypoxia. This condition gets worsened due to mitochondrial dysfunction and decrease in Na+/K+ATPase activity [39]. Nerve injury may also affect genes or proteins affecting synaptic plasticity including decreased APC/C-Cdh1 activity in the ACC, which in turn may activate AMPA channel activity to increase pain perception [36]. The increased expression of ephrin B2 [72] along with β-catenin and menin [37] in the neurons of DRG and spinal cord may also modulate synaptic activity leading to increase in pain perception (Fig. 9). Moreover, membrane hyper-excitability caused by mitochondrial and bioenergetic dysfunction after nerve injury is a significant factor that may results in neuropathic pain.
Fig. 9. Chemical structures of pharmacological agents employed to explore mechanism of neuropathic pain development.
Nevertheless, future studies are required to understand the precise interrelationship amongst these different targets. Furthermore, the comparative analysis of these targets may be done to understand the relative relevance of these targets in the pathophysiology of neuropathic pain. The pharmacological inhibitors of these therapeutic targets also exhibit adverse effects in patients such as histone deacetylase inhibitors produce nausea/vomiting, fatigue, and a transient decrease in platelet and white blood cell counts [136]; p38 inhibitors elevate liver enzymes, produce skin rashes and increase propensity to infections [137] and Wnt inhibitors possess teratogenic potential [138]. However, it is also worth mentioning that the most of inhibitors developed to inhibit these targets have been tested in preclinical studies and there is not enough studies delineating their possible side effects in clinical set up. Therefore, future studies may be designed to reveal the possible side effects of these pharmacological agents employed in neuropathic pain studies.
Footnotes
Author contributions: R.K.K. wrote the manuscript. J.S. did the revision. A.B. helped in writing manuscript. N.S. did the literature survey and helped in editing. A.S.J. conceived the idea and edited the manuscript.
CONFLICTS OF INTEREST: The authors declare no conflicts of interest.
References
- 1.Woolf CJ, Mannion RJ. Neuropathic pain: aetiology, symptoms, mechanisms, and management. Lancet. 1999;353:1959–1964. doi: 10.1016/S0140-6736(99)01307-0. [DOI] [PubMed] [Google Scholar]
- 2.Dworkin RH. An overview of neuropathic pain: syndromes, symptoms, signs, and several mechanisms. Clin J Pain. 2002;18:343–349. doi: 10.1097/00002508-200211000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Jaggi AS, Singh N. Therapeutic targets for the management of peripheral nerve injury-induced neuropathic pain. CNS Neurol Disord Drug Targets. 2011;10:589–609. doi: 10.2174/187152711796235041. [DOI] [PubMed] [Google Scholar]
- 4.Alston RP, Pechon P. Dysaesthesia associated with sternotomy for heart surgery. Br J Anaesth. 2005;95:153–158. doi: 10.1093/bja/aei152. [DOI] [PubMed] [Google Scholar]
- 5.Foley PL, Vesterinen HM, Laird BJ, Sena ES, Colvin LA, Chandran S, MacLeod MR, Fallon MT. Prevalence and natural history of pain in adults with multiple sclerosis: systematic review and meta-analysis. Pain. 2013;154:632–642. doi: 10.1016/j.pain.2012.12.002. [DOI] [PubMed] [Google Scholar]
- 6.Gilron I, Bailey JM, Tu D, Holden RR, Jackson AC, Houlden RL. Nortriptyline and gabapentin, alone and in combination for neuropathic pain: a double-blind, randomised controlled crossover trial. Lancet. 2009;374:1252–1261. doi: 10.1016/S0140-6736(09)61081-3. [DOI] [PubMed] [Google Scholar]
- 7.Dunner DL, Wohlreich MM, Mallinckrodt CH, Watkin JG, Fava M. Clinical consequences of initial duloxetine dosing strategies: comparison of 30 and 60 mg QD starting doses. Curr Ther Res Clin Exp. 2005;66:522–540. doi: 10.1016/j.curtheres.2005.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Finnerup NB, Otto M, McQuay HJ, Jensen TS, Sindrup SH. Algorithm for neuropathic pain treatment: an evidence based proposal. Pain. 2005;118:289–305. doi: 10.1016/j.pain.2005.08.013. [DOI] [PubMed] [Google Scholar]
- 9.Kukkar A, Bali A, Singh N, Jaggi AS. Implications and mechanism of action of gabapentin in neuropathic pain. Arch Pharm Res. 2013;36:237–251. doi: 10.1007/s12272-013-0057-y. [DOI] [PubMed] [Google Scholar]
- 10.Verma V, Singh N, Singh Jaggi A. Pregabalin in neuropathic pain: evidences and possible mechanisms. Curr Neuropharmacol. 2014;12:44–56. doi: 10.2174/1570159X1201140117162802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Muthuraman A, Singh N, Jaggi AS, Ramesh M. Drug therapy of neuropathic pain: current developments and future perspectives. Curr Drug Targets. 2014;15:210–253. [PubMed] [Google Scholar]
- 12.Yasuda T, Miki S, Yoshinaga N, Senba E. Effects of amitriptyline and gabapentin on bilateral hyperalgesia observed in an animal model of unilateral axotomy. Pain. 2005;115:161–170. doi: 10.1016/j.pain.2005.02.026. [DOI] [PubMed] [Google Scholar]
- 13.Zuliani V, Rivara M, Fantini M, Costantino G. Sodium channel blockers for neuropathic pain. Expert Opin Ther Pat. 2010;20:755–779. doi: 10.1517/13543771003774118. [DOI] [PubMed] [Google Scholar]
- 14.Jagodic MM, Pathirathna S, Joksovic PM, Lee W, Nelson MT, Naik AK, Su P, Jevtovic-Todorovic V, Todorovic SM. Upregulation of the T-type calcium current in small rat sensory neurons after chronic constrictive injury of the sciatic nerve. J Neurophysiol. 2008;99:3151–3156. doi: 10.1152/jn.01031.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Levy D, Tal M, Höke A, Zochodne DW. Transient action of the endothelial constitutive nitric oxide synthase (ecNOS) mediates the development of thermal hypersensitivity following peripheral nerve injury. Eur J Neurosci. 2000;12:2323–2332. doi: 10.1046/j.1460-9568.2000.00129.x. [DOI] [PubMed] [Google Scholar]
- 16.Burnstock G. Physiology and pathophysiology of purinergic neurotransmission. Physiol Rev. 2007;87:659–797. doi: 10.1152/physrev.00043.2006. [DOI] [PubMed] [Google Scholar]
- 17.Staaf S, Oerther S, Lucas G, Mattsson JP, Ernfors P. Differential regulation of TRP channels in a rat model of neuropathic pain. Pain. 2009;144:187–199. doi: 10.1016/j.pain.2009.04.013. [DOI] [PubMed] [Google Scholar]
- 18.Osikowicz M, Mika J, Makuch W, Przewlocka B. Glutamate receptor ligands attenuate allodynia and hyperalgesia and potentiate morphine effects in a mouse model of neuropathic pain. Pain. 2008;139:117–126. doi: 10.1016/j.pain.2008.03.017. [DOI] [PubMed] [Google Scholar]
- 19.Nie H, Weng HR. Impaired glial glutamate uptake induces extrasynaptic glutamate spillover in the spinal sensory synapses of neuropathic rats. J Neurophysiol. 2010;103:2570–2580. doi: 10.1152/jn.00013.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roza C, Lopez-Garcia JA. Retigabine, the specific KCNQ channel opener, blocks ectopic discharges in axotomized sensory fibres. Pain. 2008;138:537–545. doi: 10.1016/j.pain.2008.01.031. [DOI] [PubMed] [Google Scholar]
- 21.Lee J, Back SK, Lim EJ, Cho GC, Kim MA, Kim HJ, Lee MH, Na HS. Are spinal GABAergic elements related to the manifestation of neuropathic pain in rat? Korean J Physiol Pharmacol. 2010;14:59–69. doi: 10.4196/kjpp.2010.14.2.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wen YR, Suter MR, Ji RR, Yeh GC, Wu YS, Wang KC, Kohno T, Sun WZ, Wang CC. Activation of p38 mitogen-activated protein kinase in spinal microglia contributes to incision-induced mechanical allodynia. Anesthesiology. 2009;110:155–165. doi: 10.1097/ALN.0b013e318190bc16. [DOI] [PubMed] [Google Scholar]
- 23.Tsuda M, Mizokoshi A, Shigemoto-Mogami Y, Koizumi S, Inoue K. Activation of p38 mitogen-activated protein kinase in spinal hyperactive microglia contributes to pain hypersensitivity following peripheral nerve injury. Glia. 2004;45:89–95. doi: 10.1002/glia.10308. [DOI] [PubMed] [Google Scholar]
- 24.Sommer C, Lindenlaub T, Teuteberg P, Schäfers M, Hartung T, Toyka KV. Anti-TNF-neutralizing antibodies reduce pain-related behavior in two different mouse models of painful mononeuropathy. Brain Res. 2001;913:86–89. doi: 10.1016/s0006-8993(01)02743-3. [DOI] [PubMed] [Google Scholar]
- 25.Scott DA, Wright CE, Angus JA. Evidence that CB-1 and CB-2 cannabinoid receptors mediate antinociception in neuropathic pain in the rat. Pain. 2004;109:124–131. doi: 10.1016/j.pain.2004.01.020. [DOI] [PubMed] [Google Scholar]
- 26.Nabekura J, Ueno T, Okabe A, Furuta A, Iwaki T, Shimizu-Okabe C, Fukuda A, Akaike N. Reduction of KCC2 expression and GABAA receptor-mediated excitation after in vivo axonal injury. J Neurosci. 2002;22:4412–4417. doi: 10.1523/JNEUROSCI.22-11-04412.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Scheff NN, Gold MS. Trafficking of Na+/Ca2+ exchanger to the site of persistent inflammation in nociceptive afferents. J Neurosci. 2015;35:8423–8432. doi: 10.1523/JNEUROSCI.3597-14.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee SE, Kim JH. Involvement of substance P and calcitonin gene-related peptide in development and maintenance of neuropathic pain from spinal nerve injury model of rat. Neurosci Res. 2007;58:245–249. doi: 10.1016/j.neures.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 29.Bannon AW, Decker MW, Kim DJ, Campbell JE, Arneric SP. ABT-594, a novel cholinergic channel modulator, is efficacious in nerve ligation and diabetic neuropathy models of neuropathic pain. Brain Res. 1998;801:158–163. doi: 10.1016/s0006-8993(98)00596-4. [DOI] [PubMed] [Google Scholar]
- 30.Chen XL, Li XY, Qian SB, Wang YC, Zhang PZ, Zhou XJ, Wang YX. Down-regulation of spinal D-amino acid oxidase expression blocks formalin-induced tonic pain. Biochem Biophys Res Commun. 2012;421:501–507. doi: 10.1016/j.bbrc.2012.04.030. [DOI] [PubMed] [Google Scholar]
- 31.Ge Y, Jiao Y, Li P, Xiang Z, Li Z, Wang L, Li W, Gao H, Shao J, Wen D, Yu W. Coregulation of endoplasmic reticulum stress and oxidative stress in neuropathic pain and disinhibition of the spinal nociceptive circuitry. Pain. 2018;159:894–906. doi: 10.1097/j.pain.0000000000001161. [DOI] [PubMed] [Google Scholar]
- 32.Nieto FR, Cendán CM, Cañizares FJ, Cubero MA, Vela JM, Fernández-Segura E, Baeyens JM. Genetic inactivation and pharmacological blockade of sigma-1 receptors prevent paclitaxel-induced sensory-nerve mitochondrial abnormalities and neuropathic pain in mice. Mol Pain. 2014;10:11. doi: 10.1186/1744-8069-10-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ruan JP, Zhang HX, Lu XF, Liu YP, Cao JL. EphrinBs/EphBs signaling is involved in modulation of spinal nociceptive processing through a mitogen-activated protein kinases-dependent mechanism. Anesthesiology. 2010;112:1234–1249. doi: 10.1097/ALN.0b013e3181d3e0df. [DOI] [PubMed] [Google Scholar]
- 34.Khangura RK, Bali A, Jaggi AS, Singh N. Histone acetylation and histone deacetylation in neuropathic pain: an unresolved puzzle? Eur J Pharmacol. 2017;795:36–42. doi: 10.1016/j.ejphar.2016.12.001. [DOI] [PubMed] [Google Scholar]
- 35.Emery EC, Young GT, Berrocoso EM, Chen L, McNaughton PA. HCN2 ion channels play a central role in inflammatory and neuropathic pain. Science. 2011;333:1462–1466. doi: 10.1126/science.1206243. [DOI] [PubMed] [Google Scholar]
- 36.Tan W, Yao WL, Hu R, Lv YY, Wan L, Zhang CH, Zhu C. Alleviating neuropathic pain mechanical allodynia by increasing Cdh1 in the anterior cingulate cortex. Mol Pain. 2015;11:56. doi: 10.1186/s12990-015-0058-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang X, Chen G, Xue Q, Yu B. Early changes of beta-Catenins and Menins in spinal cord dorsal horn after peripheral nerve injury. Cell Mol Neurobiol. 2010;30:885–890. doi: 10.1007/s10571-010-9517-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liu S, Liu YP, Huang ZJ, Zhang YK, Song AA, Ma PC, Song XJ. Wnt/Ryk signaling contributes to neuropathic pain by regulating sensory neuron excitability and spinal synaptic plasticity in rats. Pain. 2015;156:2572–2584. doi: 10.1097/j.pain.0000000000000366. [DOI] [PubMed] [Google Scholar]
- 39.Lim TK, Rone MB, Lee S, Antel JP, Zhang J. Mitochondrial and bioenergetic dysfunction in trauma-induced painful peripheral neuropathy. Mol Pain. 2015;11:58. doi: 10.1186/s12990-015-0057-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Martin WR, Eades CG, Thompson JA, Huppler RE, Gilbert PE. The effects of morphine- and nalorphine- like drugs in the nondependent and morphine-dependent chronic spinal dog. J Pharmacol Exp Ther. 1976;197:517–532. [PubMed] [Google Scholar]
- 41.Quirion R, Bowen WD, Itzhak Y, Junien JL, Musacchio JM, Rothman RB, Su TP, Tam SW, Taylor DP. A proposal for the classification of sigma binding sites. Trends Pharmacol Sci. 1992;13:85–86. doi: 10.1016/0165-6147(92)90030-a. [DOI] [PubMed] [Google Scholar]
- 42.Hayashi T, Su TP. Sigma-1 receptor chaperones at the ER-mitochondrion interface regulate Ca2+ signaling and cell survival. Cell. 2007;131:596–610. doi: 10.1016/j.cell.2007.08.036. [DOI] [PubMed] [Google Scholar]
- 43.Tchedre KT, Huang RQ, Dibas A, Krishnamoorthy RR, Dillon GH, Yorio T. Sigma-1 receptor regulation of voltage-gated calcium channels involves a direct interaction. Invest Ophthalmol Vis Sci. 2008;49:4993–5002. doi: 10.1167/iovs.08-1867. [DOI] [PubMed] [Google Scholar]
- 44.Zamanillo D, Romero L, Merlos M, Vela JM. Sigma 1 receptor: a new therapeutic target for pain. Eur J Pharmacol. 2013;716:78–93. doi: 10.1016/j.ejphar.2013.01.068. [DOI] [PubMed] [Google Scholar]
- 45.Bangaru ML, Weihrauch D, Tang QB, Zoga V, Hogan Q, Wu HE. Sigma-1 receptor expression in sensory neurons and the effect of painful peripheral nerve injury. Mol Pain. 2013;9:47. doi: 10.1186/1744-8069-9-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Roh DH, Kim HW, Yoon SY, Seo HS, Kwon YB, Kim KW, Han HJ, Beitz AJ, Na HS, Lee JH. Intrathecal injection of the sigma(1) receptor antagonist BD1047 blocks both mechanical allodynia and increases in spinal NR1 expression during the induction phase of rodent neuropathic pain. Anesthesiology. 2008;109:879–889. doi: 10.1097/ALN.0b013e3181895a83. [DOI] [PubMed] [Google Scholar]
- 47.de la Puente B, Nadal X, Portillo-Salido E, Sánchez-Arroyos R, Ovalle S, Palacios G, Muro A, Romero L, Entrena JM, Baeyens JM, López-García JA, Maldonado R, Zamanillo D, Vela JM. Sigma-1 receptors regulate activity-induced spinal sensitization and neuropathic pain after peripheral nerve injury. Pain. 2009;145:294–303. doi: 10.1016/j.pain.2009.05.013. [DOI] [PubMed] [Google Scholar]
- 48.Kawasaki Y, Kohno T, Zhuang ZY, Brenner GJ, Wang H, Van Der Meer C, Befort K, Woolf CJ, Ji RR. Ionotropic and metabotropic receptors, protein kinase A, protein kinase C, and Src contribute to C-fiber-induced ERK activation and cAMP response element-binding protein phosphorylation in dorsal horn neurons, leading to central sensitization. J Neurosci. 2004;24:8310–8321. doi: 10.1523/JNEUROSCI.2396-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Xin WJ, Gong QJ, Xu JT, Yang HW, Zang Y, Zhang T, Li YY, Liu XG. Role of phosphorylation of ERK in induction and maintenance of LTP of the C-fiber evoked field potentials in spinal dorsal horn. J Neurosci Res. 2006;84:934–943. doi: 10.1002/jnr.21013. [DOI] [PubMed] [Google Scholar]
- 50.Chen Z, Muscoli C, Doyle T, Bryant L, Cuzzocrea S, Mollace V, Mastroianni R, Masini E, Salvemini D. NMDA-receptor activation and nitroxidative regulation of the glutamatergic pathway during nociceptive processing. Pain. 2010;149:100–106. doi: 10.1016/j.pain.2010.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ji RR, Gereau RW, 4th, Malcangio M, Strichartz GR. MAP kinase and pain. Brain Res Rev. 2009;60:135–148. doi: 10.1016/j.brainresrev.2008.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Romero L, Zamanillo D, Nadal X, Sánchez-Arroyos R, Rivera-Arconada I, Dordal A, Montero A, Muro A, Bura A, Segalés C, Laloya M, Hernández E, Portillo-Salido E, Escriche M, Codony X, Encina G, Burgueño J, Merlos M, Baeyens JM, Giraldo J, et al. Pharmacological properties of S1RA, a new sigma-1 receptor antagonist that inhibits neuropathic pain and activity-induced spinal sensitization. Br J Pharmacol. 2012;166:2289–2306. doi: 10.1111/j.1476-5381.2012.01942.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Nieto FR, Cendán CM, Sánchez-Fernández C, Cobos EJ, Entrena JM, Tejada MA, Zamanillo D, Vela JM, Baeyens JM. Role of sigma-1 receptors in paclitaxel-induced neuropathic pain in mice. J Pain. 2012;13:1107–1121. doi: 10.1016/j.jpain.2012.08.006. [DOI] [PubMed] [Google Scholar]
- 54.Zheng H, Xiao WH, Bennett GJ. Functional deficits in peripheral nerve mitochondria in rats with paclitaxel- and oxaliplatin-evoked painful peripheral neuropathy. Exp Neurol. 2011;232:154–161. doi: 10.1016/j.expneurol.2011.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Halestrap AP. What is the mitochondrial permeability transition pore? J Mol Cell Cardiol. 2009;46:821–831. doi: 10.1016/j.yjmcc.2009.02.021. [DOI] [PubMed] [Google Scholar]
- 56.Huang Q, Mao XF, Wu HY, Liu H, Sun ML, Wang X, Wang YX. Cynandione A attenuates neuropathic pain through p38β MAPK-mediated spinal microglial expression of β-endorphin. Brain Behav Immun. 2017;62:64–77. doi: 10.1016/j.bbi.2017.02.005. [DOI] [PubMed] [Google Scholar]
- 57.Moon JY, Roh DH, Yoon SY, Kang SY, Choi SR, Kwon SG, Choi HS, Han HJ, Beitz AJ, Lee JH. Sigma-1 receptor-mediated increase in spinal p38 MAPK phosphorylation leads to the induction of mechanical allodynia in mice and neuropathic rats. Exp Neurol. 2013;247:383–391. doi: 10.1016/j.expneurol.2013.01.004. [DOI] [PubMed] [Google Scholar]
- 58.Lee SA, Park JK, Kang EK, Bae HR, Bae KW, Park HT. Calmodul-independent activation of p38 and p42/44 mitogen-activated protein kinases contributes to c-fos expression by calcium in PC12 cells: modulation by nitric oxide. Brain Res Mol Brain Res. 2000;75:16–24. doi: 10.1016/s0169-328x(99)00280-6. [DOI] [PubMed] [Google Scholar]
- 59.Roh DH, Choi SR, Yoon SY, Kang SY, Moon JY, Kwon SG, Han HJ, Beitz AJ, Lee JH. Spinal neuronal NOS activation mediates sigma-1 receptor-induced mechanical and thermal hypersensitivity in mice: involvement of PKC-dependent GluN1 phosphorylation. Br J Pharmacol. 2011;163:1707–1720. doi: 10.1111/j.1476-5381.2011.01316.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Martuscello RT, Spengler RN, Bonoiu AC, Davidson BA, Helinski J, Ding H, Mahajan S, Kumar R, Bergey EJ, Knight PR, Prasad PN, Ignatowski TA. Increasing TNF levels solely in the rat hippocampus produces persistent pain-like symptoms. Pain. 2012;153:1871–1882. doi: 10.1016/j.pain.2012.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ren WJ, Liu Y, Zhou LJ, Li W, Zhong Y, Pang RP, Xin WJ, Wei XH, Wang J, Zhu HQ, Wu CY, Qin ZH, Liu G, Liu XG. Peripheral nerve injury leads to working memory deficits and dysfunction of the hippocampus by upregulation of TNF-α in rodents. Neuropsychopharmacology. 2011;36:979–992. doi: 10.1038/npp.2010.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kotagale NR, Shirbhate SH, Shukla P, Ugale RR. Agmatine attenuates neuropathic pain in sciatic nerve ligated rats: modulation by hippocampal sigma receptors. Eur J Pharmacol. 2013;714:424–431. doi: 10.1016/j.ejphar.2013.07.005. [DOI] [PubMed] [Google Scholar]
- 63.Choi SR, Roh DH, Yoon SY, Kang SY, Moon JY, Kwon SG, Choi HS, Han HJ, Beitz AJ, Oh SB, Lee JH. Spinal sigma-1 receptors activate NADPH oxidase 2 leading to the induction of pain hypersensitivity in mice and mechanical allodynia in neuropathic rats. Pharmacol Res. 2013;74:56–67. doi: 10.1016/j.phrs.2013.05.004. [DOI] [PubMed] [Google Scholar]
- 64.Torres LM, Revnic J, Knight AD, Perelman M. Relationship between onset of pain relief and patient satisfaction with fentanyl pectin nasal spray for breakthrough pain in cancer. J Palliat Med. 2014;17:1150–1157. doi: 10.1089/jpm.2014.0089. [DOI] [PubMed] [Google Scholar]
- 65.Moon JY, Choi SR, Roh DH, Yoon SY, Kwon SG, Choi HS, Kang SY, Han HJ, Kim HW, Beitz AJ, Oh SB, Lee JH. Spinal sigma-1 receptor activation increases the production of D-serine in astrocytes which contributes to the development of mechanical allodynia in a mouse model of neuropathic pain. Pharmacol Res. 2015;100:353–364. doi: 10.1016/j.phrs.2015.08.019. [DOI] [PubMed] [Google Scholar]
- 66.Klein R. Eph/ephrin signaling in morphogenesis, neural development and plasticity. Curr Opin Cell Biol. 2004;16:580–589. doi: 10.1016/j.ceb.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 67.Bundesen LQ, Scheel TA, Bregman BS, Kromer LF. Ephrin-B2 and EphB2 regulation of astrocyte-meningeal fibroblast interactions in response to spinal cord lesions in adult rats. J Neurosci. 2003;23:7789–7800. doi: 10.1523/JNEUROSCI.23-21-07789.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Battaglia AA, Sehayek K, Grist J, McMahon SB, Gavazzi I. EphB receptors and ephrin-B ligands regulate spinal sensory connectivity and modulate pain processing. Nat Neurosci. 2003;6:339–340. doi: 10.1038/nn1034. [DOI] [PubMed] [Google Scholar]
- 69.Slack S, Battaglia A, Cibert-Goton V, Gavazzi I. EphrinB2 induces tyrosine phosphorylation of NR2B via Src-family kinases during inflammatory hyperalgesia. Neuroscience. 2008;156:175–183. doi: 10.1016/j.neuroscience.2008.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kobayashi H, Kitamura T, Sekiguchi M, Homma MK, Kabuyama Y, Konno S, Kikuchi S, Homma Y. Involvement of EphB1 receptor/EphrinB2 ligand in neuropathic pain. Spine (Phila Pa 1976) 2007;32:1592–1598. doi: 10.1097/BRS.0b013e318074d46a. [DOI] [PubMed] [Google Scholar]
- 71.Song XJ, Cao JL, Li HC, Zheng JH, Song XS, Xiong LZ. Upregulation and redistribution of ephrinB and EphB receptor in dorsal root ganglion and spinal dorsal horn neurons after peripheral nerve injury and dorsal rhizotomy. Eur J Pain. 2008;12:1031–1039. doi: 10.1016/j.ejpain.2008.01.011. [DOI] [PubMed] [Google Scholar]
- 72.Zhao J, Yuan G, Cendan CM, Nassar MA, Lagerström MC, Kullander K, Gavazzi I, Wood JN. Nociceptor-expressed ephrin-B2 regulates inflammatory and neuropathic pain. Mol Pain. 2010;6:77. doi: 10.1186/1744-8069-6-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Yu LN, Sun LH, Wang M, Wang LJ, Wu Y, Yu J, Wang WN, Zhang FJ, Li X, Yan M. EphrinB-EphB signaling induces hyperalgesia through ERK5/CREB pathway in rats. Pain Physician. 2017;20:E563–E574. [PubMed] [Google Scholar]
- 74.Yu LN, Zhou XL, Yu J, Huang H, Jiang LS, Zhang FJ, Cao JL, Yan M. PI3K contributed to modulation of spinal nociceptive information related to ephrinBs/EphBs. PLoS One. 2012;7:e40930. doi: 10.1371/journal.pone.0040930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Zhou XL, Zhang CJ, Wang Y, Wang M, Sun LH, Yu LN, Cao JL, Yan M. EphrinB-EphB signaling regulates spinal pain processing via PKCγ. Neuroscience. 2015;307:64–72. doi: 10.1016/j.neuroscience.2015.08.048. [DOI] [PubMed] [Google Scholar]
- 76.Xu C, Bailly-Maitre B, Reed JC. Endoplasmic reticulum stress: cell life and death decisions. J Clin Invest. 2005;115:2656–2664. doi: 10.1172/JCI26373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kaufman RJ. Orchestrating the unfolded protein response in health and disease. J Clin Invest. 2002;110:1389–1398. doi: 10.1172/JCI16886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Beggs S, Salter MW. Microglia-neuronal signalling in neuropathic pain hypersensitivity 2.0. Curr Opin Neurobiol. 2010;20:474–480. doi: 10.1016/j.conb.2010.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ron D, Walter P. Signal integration in the endoplasmic reticulum unfolded protein response. Nat Rev Mol Cell Biol. 2007;8:519–529. doi: 10.1038/nrm2199. [DOI] [PubMed] [Google Scholar]
- 80.Gotoh T, Endo M, Oike Y. Endoplasmic reticulum stress-related inflammation and cardiovascular diseases. Int J Inflam. 2011;2011:259462. doi: 10.4061/2011/259462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hu P, Han Z, Couvillon AD, Kaufman RJ, Exton JH. Autocrine tumor necrosis factor alpha links endoplasmic reticulum stress to the membrane death receptor pathway through IRE1alpha-mediated NF-kappaB activation and down-regulation of TRAF2 expression. Mol Cell Biol. 2006;26:3071–3084. doi: 10.1128/MCB.26.8.3071-3084.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Sommer C, Kress M. Recent findings on how proinflammatory cytokines cause pain: peripheral mechanisms in inflammatory and neuropathic hyperalgesia. Neurosci Lett. 2004;361:184–187. doi: 10.1016/j.neulet.2003.12.007. [DOI] [PubMed] [Google Scholar]
- 83.Zhan X, Qian B, Cao F, Wu W, Yang L, Guan Q, Gu X2, Okusolubo TA, Dunn SL, Zhu JK, Zhu J. An Arabidopsis PWI and RRM motif-containing protein is critical for pre-mRNA splicing and ABA responses. Nat Commun. 2015;6:8139. doi: 10.1038/ncomms9139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Yang F, Whang J, Derry WT, Vardeh D, Scholz J. Analgesic treatment with pregabalin does not prevent persistent pain after peripheral nerve injury in the rat. Pain. 2014;155:356–366. doi: 10.1016/j.pain.2013.10.024. [DOI] [PubMed] [Google Scholar]
- 85.Calfon M, Zeng H, Urano F, Till JH, Hubbard SR, Harding HP, Clark SG, Ron D. IRE1 couples endoplasmic reticulum load to secretory capacity by processing the XBP-1 mRNA. Nature. 2002;415:92–96. doi: 10.1038/415092a. [DOI] [PubMed] [Google Scholar]
- 86.Iwakoshi NN, Lee AH, Vallabhajosyula P, Otipoby KL, Rajewsky K, Glimcher LH. Plasma cell differentiation and the unfolded protein response intersect at the transcription factor XBP-1. Nat Immunol. 2003;4:321–329. doi: 10.1038/ni907. [DOI] [PubMed] [Google Scholar]
- 87.Molinari M, Galli C, Piccaluga V, Pieren M, Paganetti P. Sequential assistance of molecular chaperones and transient formation of covalent complexes during protein degradation from the ER. J Cell Biol. 2002;158:247–257. doi: 10.1083/jcb.200204122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Inceoglu B, Bettaieb A, Trindade da Silva CA, Lee KS, Haj FG, Hammock BD. Endoplasmic reticulum stress in the peripheral nervous system is a significant driver of neuropathic pain. Proc Natl Acad Sci USA. 2015;112:9082–9087. doi: 10.1073/pnas.1510137112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kwiatkowski AV, Weis WI, Nelson WJ. Catenins: playing both sides of the synapse. Curr Opin Cell Biol. 2007;19:551–556. doi: 10.1016/j.ceb.2007.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Salinas PC. Wnt signaling in the vertebrate central nervous system: from axon guidance to synaptic function. Cold Spring Harb Perspect Biol. 2012;4:a008003. doi: 10.1101/cshperspect.a008003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.He X. Wnt signaling went derailed again: a new track via the LIN-18 receptor? Cell. 2004;118:668–670. doi: 10.1016/j.cell.2004.09.009. [DOI] [PubMed] [Google Scholar]
- 92.Hsieh JC, Kodjabachian L, Rebbert ML, Rattner A, Smallwood PM, Samos CH, Nusse R, Dawid IB, Nathans J. A new secreted protein that binds to Wnt proteins and inhibits their activities. Nature. 1999;398:431–436. doi: 10.1038/18899. [DOI] [PubMed] [Google Scholar]
- 93.Chandrasekharappa SC, Guru SC, Manickam P, Olufemi SE, Collins FS, Emmert-Buck MR, Debelenko LV, Zhuang Z, Lubensky IA, Liotta LA, Crabtree JS, Wang Y, Roe BA, Weisemann J, Boguski MS, Agarwal SK, Kester MB, Kim YS, Heppner C, Dong Q, et al. Positional cloning of the gene for multiple endocrine neoplasia-type 1. Science. 1997;276:404–407. doi: 10.1126/science.276.5311.404. [DOI] [PubMed] [Google Scholar]
- 94.Sawicki M, Chen G, Farley S. Menin Is a beta-catenin associated agonist of the wnt signaling pathway in pancreatic endocrine cells. J Surg Res. 2008;144:196. doi: 10.1158/1541-7786.MCR-07-2206. [DOI] [PubMed] [Google Scholar]
- 95.Zhang YK, Huang ZJ, Liu S, Liu YP, Song AA, Song XJ. WNT signaling underlies the pathogenesis of neuropathic pain in rodents. J Clin Invest. 2013;123:2268–2286. doi: 10.1172/JCI65364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Itokazu T, Hayano Y, Takahashi R, Yamashita T. Involvement of Wnt/β-catenin signaling in the development of neuropathic pain. Neurosci Res. 2014;79:34–40. doi: 10.1016/j.neures.2013.12.002. [DOI] [PubMed] [Google Scholar]
- 97.Yang QO, Yang WJ, Li J, Liu FT, Yuan H, Ou Yang YP. Ryk receptors on unmyelinated nerve fibers mediate excitatory synaptic transmission and CCL2 release during neuropathic pain induced by peripheral nerve injury. Mol Pain. 2017;13:1744806917709372. doi: 10.1177/1744806917709372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Gao K, Wang YS, Yuan YJ, Wan ZH, Yao TC, Li HH, Tang PF, Mei XF. Neuroprotective effect of rapamycin on spinal cord injury via activation of the Wnt/β-catenin signaling pathway. Neural Regen Res. 2015;10:951–957. doi: 10.4103/1673-5374.158360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Xu Z, Chen Y, Yu J, Yin D, Liu C, Chen X, Zhang D. TCF4 mediates the maintenance of neuropathic pain through Wnt/β-catenin signaling following peripheral nerve injury in rats. J Mol Neurosci. 2015;56:397–408. doi: 10.1007/s12031-015-0565-y. [DOI] [PubMed] [Google Scholar]
- 100.Lüthi A, McCormick DA. H-current: properties of a neuronal and network pacemaker. Neuron. 1998;21:9–12. doi: 10.1016/s0896-6273(00)80509-7. [DOI] [PubMed] [Google Scholar]
- 101.Notomi T, Shigemoto R. Immunohistochemical localization of Ih channel subunits, HCN1-4, in the rat brain. J Comp Neurol. 2004;471:241–276. doi: 10.1002/cne.11039. [DOI] [PubMed] [Google Scholar]
- 102.George MS, Abbott LF, Siegelbaum SA. HCN hyperpolarization-activated cation channels inhibit EPSPs by interactions with M-type K+ channels. Nat Neurosci. 2009;12:577–584. doi: 10.1038/nn.2307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Liu X, Zhang L, Jin L, Tan Y, Li W, Tang J. HCN2 contributes to oxaliplatin-induced neuropathic pain through activation of the CaMKII/CREB cascade in spinal neurons. Mol Pain. 2018;14:1744806918778490. doi: 10.1177/1744806918778490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Yeon KY, Chung G, Kim YH, Hwang JH, Davies AJ, Park MK, Ahn DK, Kim JS, Jung SJ, Oh SB. Eugenol reverses mechanical allodynia after peripheral nerve injury by inhibiting hyperpolarization-activated cyclic nucleotide-gated (HCN) channels. Pain. 2011;152:2108–2116. doi: 10.1016/j.pain.2011.05.018. [DOI] [PubMed] [Google Scholar]
- 105.Du L, Wang SJ, Cui J, He WJ, Ruan HZ. Inhibition of HCN channels within the periaqueductal gray attenuates neuropathic pain in rats. Behav Neurosci. 2013;127:325–329. doi: 10.1037/a0031893. [DOI] [PubMed] [Google Scholar]
- 106.Young GT, Emery EC, Mooney ER, Tsantoulas C, McNaughton PA. Inflammatory and neuropathic pain are rapidly suppressed by peripheral block of hyperpolarisation-activated cyclic nucleotide-gated ion channels. Pain. 2014;155:1708–1719. doi: 10.1016/j.pain.2014.05.021. [DOI] [PubMed] [Google Scholar]
- 107.Smith T, Al Otaibi M, Sathish J, Djouhri L. Increased expression of HCN2 channel protein in L4 dorsal root ganglion neurons following axotomy of L5- and inflammation of L4-spinal nerves in rats. Neuroscience. 2015;295:90–102. doi: 10.1016/j.neuroscience.2015.03.041. [DOI] [PubMed] [Google Scholar]
- 108.Cordeiro Matos S, Zhang Z, Séguéla P. Peripheral neuropathy induces HCN channel dysfunction in pyramidal neurons of the medial prefrontal cortex. J Neurosci. 2015;35:13244–13256. doi: 10.1523/JNEUROSCI.0799-15.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Angermüller S, Islinger M, Völkl A. Peroxisomes and reactive oxygen species, a lasting challenge. Histochem Cell Biol. 2009;131:459–463. doi: 10.1007/s00418-009-0563-7. [DOI] [PubMed] [Google Scholar]
- 110.Wang YX, Gong N, Xin YF, Hao B, Zhou XJ, Pang CC. Biological implications of oxidation and unidirectional chiral inversion of D-amino acids. Curr Drug Metab. 2012;13:321–331. doi: 10.2174/138920012799320392. [DOI] [PubMed] [Google Scholar]
- 111.Yoshikawa M, Oka T, Kawaguchi M, Hashimoto A. MK-801 up-regulates the expression of d-amino acid oxidase mRNA in rat brain. Brain Res Mol Brain Res. 2004;131:141–144. doi: 10.1016/j.molbrainres.2004.08.017. [DOI] [PubMed] [Google Scholar]
- 112.Lu JM, Gong N, Wang YC, Wang YX. D-Amino acid oxidase-mediated increase in spinal hydrogen peroxide is mainly responsible for formalin-induced tonic pain. Br J Pharmacol. 2012;165:1941–1955. doi: 10.1111/j.1476-5381.2011.01680.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Williams M. Commentary: genome-based CNS drug discovery: D-amino acid oxidase (DAAO) as a novel target for antipsychotic medications: progress and challenges. Biochem Pharmacol. 2009;78:1360–1365. doi: 10.1016/j.bcp.2009.06.108. [DOI] [PubMed] [Google Scholar]
- 114.Shahbazian MD, Grunstein M. Functions of site-specific histone acetylation and deacetylation. Annu Rev Biochem. 2007;76:75–100. doi: 10.1146/annurev.biochem.76.052705.162114. [DOI] [PubMed] [Google Scholar]
- 115.Lin TB, Hsieh MC, Lai CY, Cheng JK, Chau YP, Ruan T, Chen GD, Peng HY. Modulation of nerve injury-induced HDAC4 cytoplasmic retention contributes to neuropathic pain in rats. Anesthesiology. 2015;123:199–212. doi: 10.1097/ALN.0000000000000663. [DOI] [PubMed] [Google Scholar]
- 116.Cherng CH, Lee KC, Chien CC, Chou KY, Cheng YC, Hsin ST, Lee SO, Shen CH, Tsai RY, Wong CS. Baicalin ameliorates neuropathic pain by suppressing HDAC1 expression in the spinal cord of spinal nerve ligation rats. J Formos Med Assoc. 2014;113:513–520. doi: 10.1016/j.jfma.2013.04.007. [DOI] [PubMed] [Google Scholar]
- 117.Kukkar A, Singh N, Jaggi AS. Attenuation of neuropathic pain by sodium butyrate in an experimental model of chronic constriction injury in rats. J Formos Med Assoc. 2014;113:921–928. doi: 10.1016/j.jfma.2013.05.013. [DOI] [PubMed] [Google Scholar]
- 118.Hobo S, Eisenach JC, Hayashida K. Up-regulation of spinal glutamate transporters contributes to anti-hypersensitive effects of valproate in rats after peripheral nerve injury. Neurosci Lett. 2011;502:52–55. doi: 10.1016/j.neulet.2011.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Chiechio S, Zammataro M, Morales ME, Busceti CL, Drago F, Gereau RW, 4th, Copani A, Nicoletti F. Epigenetic modulation of mGlu2 receptors by histone deacetylase inhibitors in the treatment of inflammatory pain. Mol Pharmacol. 2009;75:1014–1020. doi: 10.1124/mol.108.054346. [DOI] [PubMed] [Google Scholar]
- 120.Zammataro M, Sortino MA, Parenti C, Gereau RW, 4th, Chiechio S. HDAC and HAT inhibitors differently affect analgesia mediated by group II metabotropic glutamate receptors. Mol Pain. 2014;10:68. doi: 10.1186/1744-8069-10-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Kami K, Taguchi S, Tajima F, Senba E. Histone acetylation in microglia contributes to exercise-induced hypoalgesia in neuropathic pain model mice. J Pain. 2016;17:588–599. doi: 10.1016/j.jpain.2016.01.471. [DOI] [PubMed] [Google Scholar]
- 122.Uchida H, Matsushita Y, Araki K, Mukae T, Ueda H. Histone deacetylase inhibitors relieve morphine resistance in neuropathic pain after peripheral nerve injury. J Pharmacol Sci. 2015;128:208–211. doi: 10.1016/j.jphs.2015.07.040. [DOI] [PubMed] [Google Scholar]
- 123.Zhang Y, Gong K, Zhou W, Shao G, Li S, Lin Q, Li J. Involvement of subtypesγ and ε of protein kinase C in colon pain induced by formalin injection. Neurosignals. 2011;19:142–150. doi: 10.1159/000328311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Sas K, Robotka H, Toldi J, Vécsei L. Mitochondria, metabolic disturbances, oxidative stress and the kynurenine system, with focus on neurodegenerative disorders. J Neurol Sci. 2007;257:221–239. doi: 10.1016/j.jns.2007.01.033. [DOI] [PubMed] [Google Scholar]
- 125.Janes K, Doyle T, Bryant L, Esposito E, Cuzzocrea S, Ryerse J, Bennett GJ, Salvemini D. Bioenergetic deficits in peripheral nerve sensory axons during chemotherapy-induced neuropathic pain resulting from peroxynitrite-mediated post-translational nitration of mitochondrial superoxide dismutase. Pain. 2013;154:2432–2440. doi: 10.1016/j.pain.2013.07.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Chen KH, Lin CR, Cheng JT, Cheng JK, Liao WT, Yang CH. Altered mitochondrial ATP synthase expression in the rat dorsal root ganglion after sciatic nerve injury and analgesic effects of intrathecal ATP. Cell Mol Neurobiol. 2014;34:51–59. doi: 10.1007/s10571-013-9986-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Inoue K. Neuropharmacological study of ATP receptors, especially in the relationship between glia and pain. Yakugaku Zasshi. 2017;137:563–569. doi: 10.1248/yakushi.16-00262. [DOI] [PubMed] [Google Scholar]
- 128.Steen KH, Steen AE, Kreysel HW, Reeh PW. Inflammatory mediators potentiate pain induced by experimental tissue acidosis. Pain. 1996;66:163–170. doi: 10.1016/0304-3959(96)03034-5. [DOI] [PubMed] [Google Scholar]
- 129.Wong AS, Gumbiner BM. Adhesion-independent mechanism for suppression of tumor cell invasion by E-cadherin. J Cell Biol. 2003;161:1191–1203. doi: 10.1083/jcb.200212033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Husseman JW, Nochlin D, Vincent I. Mitotic activation: a convergent mechanism for a cohort of neurodegenerative diseases. Neurobiol Aging. 2000;21:815–828. doi: 10.1016/s0197-4580(00)00221-9. [DOI] [PubMed] [Google Scholar]
- 131.Puram SV, Bonni A. Novel functions for the anaphase-promoting complex in neurobiology. Semin Cell Dev Biol. 2011;22:586–594. doi: 10.1016/j.semcdb.2011.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Fu AK, Hung KW, Fu WY, Shen C, Chen Y, Xia J, Lai KO, Ip NY. APC(Cdh1) mediates EphA4-dependent downregulation of AMPA receptors in homeostatic plasticity. Nat Neurosci. 2011;14:181–189. doi: 10.1038/nn.2715. [DOI] [PubMed] [Google Scholar]
- 133.Qu C, King T, Okun A, Lai J, Fields HL, Porreca F. Lesion of the rostral anterior cingulate cortex eliminates the aversiveness of spontaneous neuropathic pain following partial or complete axotomy. Pain. 2011;152:1641–1648. doi: 10.1016/j.pain.2011.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Tan Y, Wang J, Su S, Wang Q, Jiang S, Lu L, Chen YH. Enhancement of endocytic uptake of HIV-1 virions into CD4-negative epithelial cells by HIV-1 gp41 via its interaction with POB1. Cell Mol Immunol. 2017;14:568–571. doi: 10.1038/cmi.2015.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Zhao WJ, Gao ZY, Wei H, Nie HZ, Zhao Q, Zhou XJ, Wang YX. Spinal D-amino acid oxidase contributes to neuropathic pain in rats. J Pharmacol Exp Ther. 2010;332:248–254. doi: 10.1124/jpet.109.158816. [DOI] [PubMed] [Google Scholar]
- 136.Subramanian S, Bates SE, Wright JJ, Espinoza-Delgado I, Piekarz RL. Clinical toxicities of histone deacetylase inhibitors. Pharmaceuticals (Basel) 2010;3:2751–2767. doi: 10.3390/ph3092751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Fisk M, Gajendragadkar PR, Mäki-Petäjä KM, Wilkinson IB, Cheriyan J. Therapeutic potential of p38 MAP kinase inhibition in the management of cardiovascular disease. Am J Cardiovasc Drugs. 2014;14:155–165. doi: 10.1007/s40256-014-0063-6. [DOI] [PubMed] [Google Scholar]
- 138.Kahn M. Can we safely target the WNT pathway? Nat Rev Drug Discov. 2014;13:513–532. doi: 10.1038/nrd4233. [DOI] [PMC free article] [PubMed] [Google Scholar]