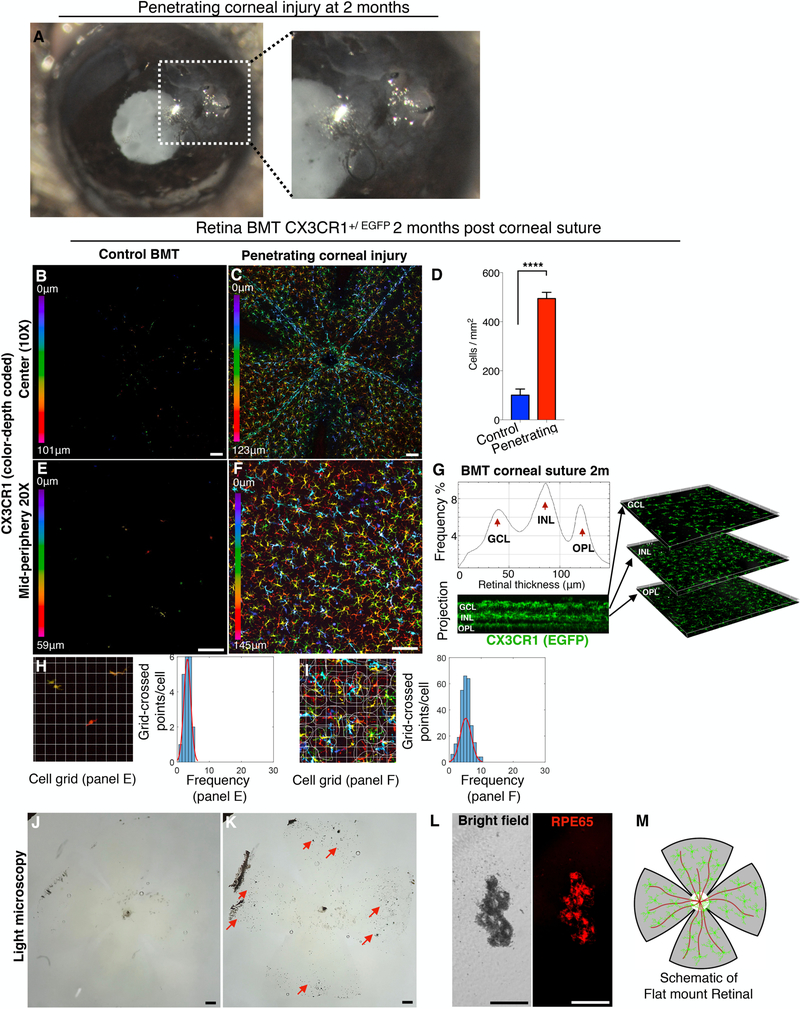
Figure 4. Penetrating corneal injury leads to peripheral CX3CR1+ infiltration and engraftment into the retina.
(A) Penetrating cornea injury performed by full-thickness placement of 11–0 vycril suture in the cornea. (B, E) CX3CR1+/EGFP bone marrow chimera model shows no peripheral monocyte infiltration in the absence of a suture. (C, D, F) Penetrating corneal injury causes engraftment of peripheral CX3CR1+ monocytes into the retina with a ramified appearance at 2 months. (G) Engrafted peripheral CX3CR1+ monocytes migrate into the three distinct microglia strata (ganglion cell, inner nuclear cell, and outer plexiform cell layers) 2 months after the injury. (H, I) Peripheral monocytes that infiltrate the retina after penetrating ocular injury have more ramified morphology compared to control BMT mice (P<0.0001) but appear less ramified compared to resident (native) microglia (P<0.0001). (J-L) Penetrating corneal injury causes pigmentation of the inner retina (red arrows) by RPE65+ cells. (M) Schematic representation of flat mount retina used for confocal microscopy. BMT: bone marrow transfer, OHT: ocular hypertension. Three independent experiments with 1 mouse per group per experiment. (B, C, E, F, J, K) Scale bar: 100μm. (L) Scale bar: 50μm. Student t-test ****P<0.0001.