Abstract
Chronic cocaine and alcohol use impart significant stress on biological and cognitive systems, resulting in changes consistent with an allostatic load model of neurocognitive impairment.
The present study measured potential markers of allostatic load in individuals with comorbid cocaine/alcohol use disorders (CUD/AUD) and control subjects. Measures of brain white matter (WM), telomere length, and impulsivity/attentional bias were obtained. WM (CUD/AUD only) was indexed by diffusion tensor imaging metrics, including radial diffusivity (RD) and fractional anisotropy (FA). Telomere length was indexed by the telomere to single copy gene (T/S) ratio. Impulsivity and attentional bias to drug cues were measured via eye-tracking, and were also modeled using the Hierarchical Diffusion Drift Model (HDDM). Average whole-brain RD and FA were associated with years of cocaine use (R2 = 0.56 and 0.51, both p < .005) but not years of alcohol use. CUD/AUD subjects showed more anti-saccade errors (p < .01), greater attentional bias scores (p < .001), and higher HDDM drift rates on cocaine-cue trials (Bayesian probability CUD/AUD > control = p > 0.99). Telomere length was shorter in CUD/AUD, but the difference was not statistically significant. Within the CUD/AUD group, exploratory regression using an elastic-net model determined that more years of cocaine use, older age, larger HDDM drift rate differences and shorter telomere length were all predictive of WM as measured by RD (model R2 = 0.79). Collectively, the results provide modest support linking CUD/AUD to putative markers of allostatic load.
Introduction
Allostasis implies a shift in homeostatic systems in response to acute or chronic stressors (e.g., allostatic load), described by McEwen as “the price the body pays for being forced to adapt to adverse psychosocial or physical situations” [1]. Exposure to extreme or pervasive stressors can result in pathophysiological change. Examination of allostatic load has commonly focused on changes in the regulation of stress hormones and the sequelae of such changes [2,3], but the concept can apply broadly to effects on many homeostatic systems. Nearly two decades ago, Koob and colleagues proposed allostatic models of chronic cocaine and alcohol intake based on preclinical work [4–6], but only modest attention has focused on the allostasic framework in studying human substance use disorders (SUD). Here, we focus on the effects of chronic SUD in adults with co-morbid cocaine and alcohol use disorders [7–9].
Among those with cocaine use disorder (CUD), co-occurring substance abuse, e.g., marijuana and/or alcohol use disorder (AUD), is the norm rather than the exception [10]. Individuals who use only cocaine are of putative scientific importance with regard to isolating individual drug effects. However, such investigations are more precisely understood using preclinical models that can isolate dose-response relationships. In reality, because cocaine-only users are rare, they may represent a phenotype of lesser clinical or applied interest. From the standpoint of measuring indicators of CUD that translate to real world effects, alterations in biological and neurocognitive function are probably best understood as the result of the synergistic impact of CUD plus abuse of other substances.
The present study focused on brain white matter integrity, telomere length, and eye movement indices of impulse/attentional control. While not a comprehensive set of biological or cognitive markers of CUD/AUD-related impairment, these domains are indicators of health and cognitive functioning. Importantly, varying degrees of evidence exist to suggest that each domain is adversely modified by chronic cocaine and alcohol use [11–18]. Each marker–white matter integrity, telomere length, and anti-saccade performance–is broadly associated with neurological and psychiatric disease processes, independent of substance use disorders [19–30], and thus collectively provides an indicator of possible allostatic load extrapolated from a broader evidence base applied to CUD/AUD. We expected to observe evidence of impairment for each marker related to CUD/AUD and the cumulative effects of abusing these substances.
Methods
Subjects
Participants for this project were recruited from the Greater Houston Metropolitan Area using local newspaper and radio advertisements. The data reported here constitute part of a larger clinical trial examining the effects 12-weeks of treatment with pioglitazone in participants with a primary cocaine use disorder (CUD) and a secondary alcohol use disorder (AUD), described in [31] (NCT02774343). For the present report, data were obtained from measures taken at baseline (Day 0), prior to initiation of the clinical trial. The dataset included 22 CUD/AUD subjects who provided complete neuroimaging, eye tracking, and telomere data. Two additional CUD/AUD subjects provided eye tracking and telomere data without DTI. In addition, data from two independent samples of 35 (eye tracking) and 25 (telomere) healthy control subjects were obtained for purposes of comparison with the CUD/AUD subjects. DTI was not obtained from control participants, who were not part of the clinical trial, as neuroimaging of control subjects was beyond both the scope and budget of the project. Additionally, numerous studies have previously characterized white matter integrity in CUD and AUD [11–13,32–35]. The study was carried out in accordance with the recommendations of the Belmont Report and the approval of the UTHSC-Houston IRB. All subjects gave written informed consent obtained in person in accordance with the Declaration of Helsinki. Subject characteristics are provided in Table 1.
Table 1. Demographic characteristics for CUD/AUD subjects (N = 22 completed DTI) and control groups for the anti-saccade (eye) and telomere length (telo) data.
Values represent mean (SD) or Number # (%). P-values represent outcomes from two-sample t-tests (age education, Shipley-2) or Fisher’s Exact Test (sex, race).
| Variable | Group | p-values | ||
|---|---|---|---|---|
| CUD/AUD | control (eye) | control (telo) | ||
| N | 24 | 35 | 25 | — |
| Age | 46.96 (7.66) | 42.49 (10.17) | 43.76 (6.62) | a. < 0.07 b. < 0.12 |
| Sex, # M (%) | 18 (75.00) | 17 (48.57) | 17 (68.00) | a. < 0.06 b. < 0.75 |
| Education | 12.69 (1.52) | 14.06 (2.39) | 14.00 (2.55) | a. < 0.02 b. < 0.03 |
| Race | a. < 0.58 b. < 0.34 |
|||
| AA | 14 (58.33) | 25 (71.43) | 18 (72.00) | |
| C | 6 (25.00) | 5 (14.29) | 2 (8.00) | |
| H | 4 (16.67) | 5 (14.29) | 5 (20.00) | |
| Shipley-2 | 87.67 (13.10) | 94.63 (14.15) | 99.60 (10.87) | a. < 0.07 b. < 0.16 |
| Cocaine (yrs) | 17.96 (8.34) | — | — | — |
| Alcohol (yrs) | 21.62 (12.27) | — | — | — |
a. CUD vs. control (eye-tracking)
b. CUD vs. control (telomere length)
Measures
Demographic and clinical
The following measures were obtained for all subjects: age, sex, education, race, cognitive aptitude (Shipley-2, [36]), and mental health functioning via Structured Clinical Interview for DSM-IV (SCID-IV, [37]). For CUD/AUD subjects, lifetime and recent substance use were determined via the SCID-IV, the Addiction Severity Index [38], and the Kreek-McHugh-Schluger-Kellogg scale (KMSK, [39]).
Diffusion Tensor Imaging (DTI)
DTI is a magnetic resonance imaging technique that is used to map brain white matter (WM) fibers by quantifying the tissue diffusion properties of water. DTI-derived metrics examined here included axial, radial, and mean diffusivity (AD, RD, and MD, respectively), as well as fractional anisotropy (FA). These metrics have been used to infer CNS white matter pathology in a number of neurological and psychiatric diseases [40–44]. DTI methods, scanning parameters, and data processing details are provided in Supporting Information (S1 File). In summary, for each subject (N = 22) whole brain voxel-wise FA, MD, RD, and AD maps were generated with toolboxes provided by FSL [45] using the Tract-Based Spatial Statistics (TBSS) method [46,47]. DTI-derived maps were transformed into MNI152 standard space by nonlinearly registering each map to a standard template provided with FSL using a non-linear registration method (FNIRT, [47]). Each subject’s FA map was projected onto the corresponding FA skeleton, allowing for voxelwise analysis across subjects using a permutation-based non-parametric statistical method (RANDOMISE, [48]) with 5000 permutations. T1-based analyses with SPM and Freesurfer examining grey matter volume, white matter volume, and cortical thickness and their relationships to cocaine use did not reveal any significant patterns. Additionally, all scans were reviewed by a radiologist to ensure that there were no gross anatomical abnormalities. Consequently, the present DTI-based results may represent a unique white-matter marker that are not captured by volumetrics or gross brain pathology.
Anti-saccade task
The details of the eye-tracking task are provided in Dias et al [15]. Briefly, participants were tested using an infrared binocular eye-tracker to measure performance on blocks of pro-saccade and anti-saccade trials (36 trials per block). Following training to minimize blinking and optimize task understanding, four counterbalanced blocks were administered (2 pro-saccade, 2 anti-saccade, 144 trials total). Stimuli included cocaine-related images, neutral images matched as closely as possible to the cocaine images (e.g., color, background, complexity), and size-matched solid gray shapes. The eye-tracking data were analyzed as (1) overall error rates on all anti-saccade trials (global inhibitory control), (2) the ratio of anti-saccade errors on cocaine-stimulus trials to total anti-saccade errors over all trials (cocaine/total: attentional bias towards cocaine cues). Anti-saccade errors provide an index of inhibitory control circuitry, both with regard to neural pathways subserving the control of eye movements and to markers of pathology in psychiatric and neurological disease [49,50]. Attentional bias provides an index of asymmetrical attentional control by the salience of specific stimuli (in this case cocaine cues) relative to neutral stimuli, with clinical relevance to SUD [15,51,52].
Hierarchical drift diffusion model (HDDM)
Error rates and attentional bias are robust but coarse and descriptive measures of anti-saccade performance. Accordingly, eye-tracking performance was also examined with a conceptually-informed approach from cognitive neuroscience, the HDDM [53]. The HDDM is a drift diffusion / sequential sampling model of decision making that incorporates both accuracy and reaction time, based on a threshold model in which evidence for a decision (here, execution of an anti-saccade) accumulates in the context of imperfect information (noise). The HDDM capitalizes on both the theoretical utility of the drift diffusion framework and the use of Bayesian data analytic methods, which have substantial utility in modeling neural and cognitive phenomena [54]. The analysis focused on the HDDM parameter v (drift rate). Herein, we interpret differences in v as evidence of differential salience of the cocaine (vs. non-drug) stimuli, such that for the CUD/AUD group the cocaine stimuli increase decision conflict reflected in both accuracy and reaction time. Details of this model, including conceptual foundations and neural correlates can be found in [55,56]. Additionally, details of the HDDM outcomes, including model output (group and individual subject), and metrics of model convergence and fit are provided in the Supporting Information (S2 File).
Telomere length
Genomic DNA was extracted from leukocytes by standard procedures. DNA concentration was assessed by Nanodrop and telomere length was measured quantitatively by PCR, as previously described [56]. Briefly, primers for the telomere sequence (T) are tel1b: 5’-CGGTTT(GTTTGG)5GTT-3’ and tel2b: 5’-GGCTTG(CCTTAC)5CCT-3’. The single-copy gene human beta-globin was used as the reference gene (S), with the following primers: hbg1 5’-GCTTCTGACACAACTGTGTTCACTAGC-3’ and hbg2 5’ CCAACTTCATCCACGTTCACC-3’. T and S values were quantified relative to a reference DNA sample by the standard curve method. Since the number of S copies are the same in all individuals, relative T/S ratio (the primary dependent variable) reflects relative length differences in telomeric DNA. All PCRs were carried out using the thermal cycling profiles previously described in [57], with DNA samples run in duplicate on separate plates but in the same well positions.
Data analytic strategy
DTI: Confirmatory analyses
We examined the relationship between FA, RD, MD and AD values and years of cocaine use while controlling for alcohol use (and vice versa), and combined years of both substances (controlling for age and sex in all models). As no control groups were available for DTI, all analyses were within CUD/AUD subjects. Combined years of use was calculated by adding the years of cocaine use to years of alcohol use. Clinical interviews at screening were used to estimate chronicity of lifetime use. The interview instruments included the ASI, SCID, and the Kreek-McHugh-Schluger-Kellogg (KMSK) scale. Based on the information obtained in these interviews, it was determined that cocaine and alcohol use patterns were consistent across individual subjects’ lifetime (e.g., no marked periods of abstinence or changes in use patterns from the time substance abuse began). Therefore, given subjects’ age range and history of use (cocaine mean years of use = 5.13, range = 5.5–36.0; alcohol mean years of use = 6.18, range = 2.75–40.0), we determined that years of use was the best proxy for cocaine and alcohol exposure with regard to recall accuracy, minimizing error in the measurement of extent of substance exposure. Notably, chronicity has been cited as a critical component in addiction diagnostics [58]. All regression models controlled for age, education, sex and Shipley score, with the significance threshold set at p < 0.005. The regression analyses resulted in a map highlighting all identified significant clusters. The relationship between the average FA value for all significant clusters was calculated for each subject and plotted as a function of years of use (see Fig 1). The same pipeline was then used for the MD, RD, and AD scalars.
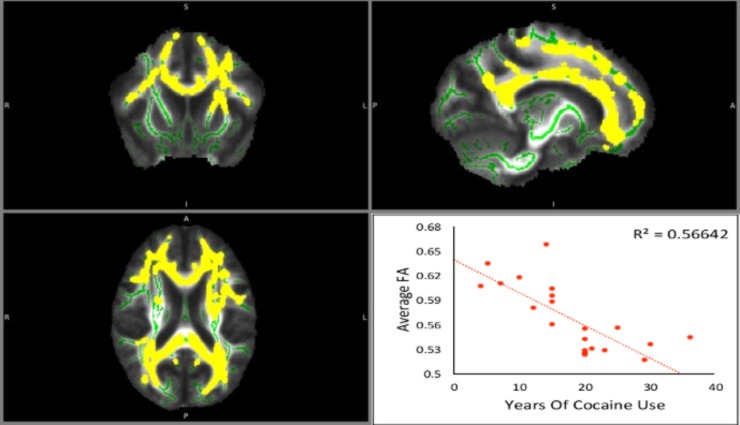
Fig 1. Fractional anisotropy (FA) maps, showing coronal, sagittal, and axial views (respectively) of white matter tracts in 22 CUD/AUD subjects.
Major tracts are outlined in green and areas highlighted in yellow represent group-level significant associations with years of cocaine use, controlling for the covariates alcohol use, age, and gender. The bottom right panel shows a scatter plot of average whole-brain FA value (y-axis) as a function of years of cocaine use (x-axis) for individual subjects (R2 = 0.56). Please note the radiological conventions marked on the sides of the Fig 1 for each view: R (right), L (left), S (superior), I (inferior), A (anterior) or P (posterior).
Anti-saccade task: Confirmatory analyses
Consistent with Dias et al [15] and with the overall literature on saccade-based performance, there were no differences between CUD and control subjects on pro-saccade trials. Accordingly, data analyses focused on anti-saccade trials. Per Pocock [59], we examined the influence of potential confounding variables (age, education, sex, Shipley score) by testing for (1) between-group differences and (2) correlations with the dependent variables of interest (total anti-saccade errors, attentional bias). Age and education showed group differences and correlations with p-values < .10, and were thus treated as covariates in linear regression models that examined differences between CUD/AUD vs. controls on total anti-saccade errors and attentional bias.
HDDM: Confirmatory analyses
The HDDM package in Python [53,55] was used to fit a hierarchical model to compare the probability distributions of differences in v (drift rate) between groups and stimulus types. The HDDM package provides estimation of differences in Bayesian posterior probability distributions by computing the proportion of posteriors in which v (drift rate) is greater in one condition than another. Differences were compared for each stimulus type (cocaine, neutral, shape) both within and between groups. Model fitting and convergence details are provided in the Supporting Information (S2 File).
After comparing the Bayesian probability distributions of differences in v (drift) between groups and between stimuli, individual v (drift) values for each subject were extracted and entered into a linear regression model controlling for age and education, in order to replicate the confirmatory frequentist models used to analyze total anti-saccade errors and attentional bias. To create a single dependent variable for the frequentist analyses, a difference score was created for each subject by subtracting v on cocaine-stimulus trials from non-cocaine stimulus (neutral+shape) trials.
Telomere length: Confirmatory analyses
The T/S ratio was examined in a linear regression model that compared differences between CUD/AUD vs. controls with age and education as covariates in same manner as described above.
Hypothesis-generating analyses: White matter, anti-saccades, and telomere length
Because the dataset was limited to 22 subjects who provided complete DTI, eye-tracking and telomere data, we utilized modern regularization techniques with penalized regression. Two primary penalized regression approaches, ridge and lasso, can be linearly combined via elastic-net regression, which overcomes limitations of each type but includes both as special cases [60,61]. Leave-one-out cross-validation (LOOCV) was employed to optimize the tuning parameters of the model, e.g., to determine the alpha (the mixing or penalty parameter, range 0–1) and lambda (regularization or coefficient shrinkage parameter) parameters of the elastic net model that minimize the mean squared error [61,62]. These analyses were conducted using R software version 3.3.2 [63] and the R glmnet package, based on modeling techniques recommended by the authors [60]. To provide further model interpretability, the R package selectiveInference [64] was integrated with the glmnet model outcomes to provide z-score, p-value, and confidence interval estimates for the obtained model coefficients, as per [62]. Using this approach, we modeled the relationship between DTI radial diffusivity (RD, dependent variable) and the following predictors: telomere length (T/S ratio); anti-saccades (HDDM difference score on v for cocaine vs. non-cocaine trials); and total years of cocaine use. To control for relevant covariates, age and years of alcohol use were included in the model. RD was selected because it contained the largest number of significant clusters related to years of cocaine use, and because of its probable connection to compromised myelination [11,32,65]. All variables were standardized by z-scoring to provide interpretability of the model coefficients.
Results
Diffusion tensor imaging
As shown in Fig 1, FA values decreased as a function of years of cocaine use, controlling for years of alcohol use, age, sex, education and Shipley score, p < .005, R2 = 0.56. The significant clusters (in yellow) associated with cocaine use were identified along several major tracts (in green), including the corpus callosum, the right thalamic radiation, the right superior longitudinal fasciculus, and the corona radiata. Notably, analysis of AD values revealed no significant relationship between AD and years of cocaine use, while RD and MD values increased with years of cocaine use, R2 = 0.51 and 0.46, respectively (p < .05 for both RD and MD). RD clusters were the most widespread and included the internal capsule, corona radiata, optic radiation, tapetum, superior longitudinal fasciculus, posterior thalamic radiation, and all clusters also found in the FA maps. Although there were significant RD clusters in both hemispheres, clusters were larger in the right hemisphere. Fig 1 highlights the significant FA clusters, and provides a scatterplot of the relationship between FA and years of cocaine use, controlling for covariates. Details for all significant clusters for the FA, RD, and MD maps are provided in the Supporting Information (S1 Table).
No significant clusters were found when examining the relationship between any of the DTI scalars with years of alcohol use or years of combined cocaine + alcohol use, controlling for other relevant covariates. With no observed relationships within the AD values, it follows that the significant clusters in the FA map are probably driven by the relationship between RD and years of cocaine use. Consequently, all of the areas significant in the FA and MD maps are also significant in the RD map. The RD map contains the largest number of significant clusters, which were not lessened by input from non-significant AD differences.
Anti-saccade task
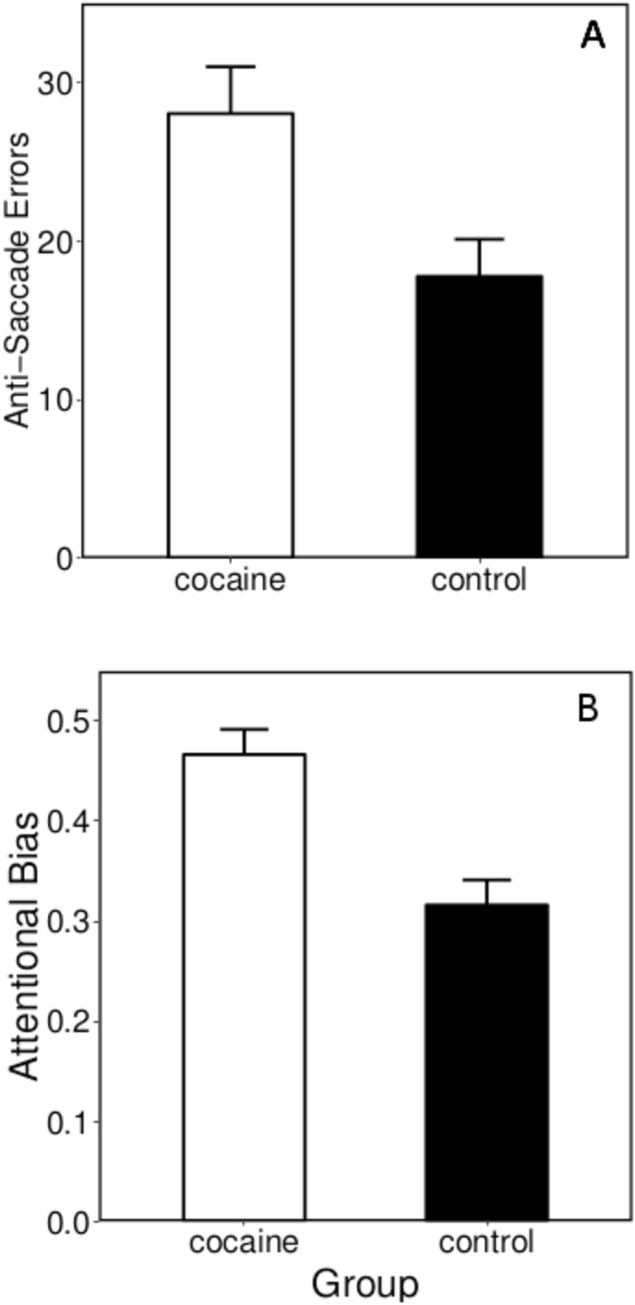
Fig 2 summarizes the total anti-saccade error and attentional bias data. For the eye-tracking data linear models, degrees of freedom and R2 values are provided along with t-values, p-values, and group means (± SEM) for any significant predictor variables. For total anti-saccade errors, df = 3, 55, R2 = 0.24: for group (t = 2.70, p < .001); for age (t = 2.31, p < .03). CUD/AUD made more anti-saccade errors than controls, 28.04 (± 2.96) vs. 17.77 (± 2.34). For attentional bias scores, df = 3, 55, R2 = 0.29; for group (t = 4.69, p < .001); for age (t = 1.04, p < .31). CUD/AUD had higher attentional bias scores than controls, 0.47 (± 0.03) vs. 0.32 (± 0.03).
Fig 2. Anti-saccade performance of CUD/AUD subjects and control subjects on the cocaine eye-tracking task.
Panels A and B show mean total anti-saccade errors and attentional bias scores (± SEM), respectively. The attentional bias score was calculated as anti-saccade errors on cocaine-stimulus trials / total anti-saccade errors on all trials, providing an indicator of attentional bias towards cocaine cues.
Anti-saccade task: HDDM
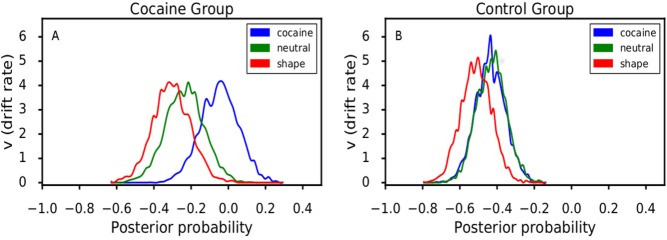
The posterior probabilities for the HDDM drift rates (v) for the CUD/AUD and control groups are shown in Fig 3, depicting both consistently longer and more highly variable drift rates in CUD/AUD across all stimulus types. Between groups, the Bayesian posterior probabilities that v for CUD/AUD > control on cocaine-, neutral-, and shape-stimulus trials were 0.99, 0.94, and 0.95, respectively. Examining v among stimulus types within the CUD/AUD group, the following Bayesian posterior probabilities were observed: cocaine > neutral = 0.90; cocaine > shape = 0.96; neutral > shape = 0.68. For the control group, the corresponding probabilities were 0.47, 0.74, and 0.77, respectively. Shown graphically in Fig 3, note that a posterior probability = 0.50 is essentially chance (note overlapping distributions in the control group corresponding to p = 0.47). For the frequentist linear model of drift rate (v) difference scores (cocaine–neutral+shape stimuli), df = 3, 55, R2 = 0.10; for group (t = 2.08, p < .05). CUD/AUD had higher drift rates than controls, 0.17 (± 0.05) vs. 0.05 (± 0.04).
Fig 3. Posterior probabilities of drift rates (v parameter) derived from the Bayesian hierarchical drift diffusion model (HDDM) for each stimulus type presented on the anti-saccade task.
The HDDM models decision making under two-option conditions; the options here were executing a saccade toward the stimulus or an anti-saccade away from the stimulus. HDDM uses Markov chain Monte Carlo to estimate posterior distributions for all model parameters based on both response accuracy and time to execute the response (e.g., execute a saccade), the results of which are plotted for v in Fig 3 (see [53] for HDDM computational details). Drift rate can be conceptualized as the rate at which information is accumulated toward a decision-threshold prior to executing a response. Stimulus contexts presenting, for example, greater conflict or increased background noise should increase drift rate. In Fig 3, drift rate parameters are shown separately for the cocaine group (panel A, left) and the control group (panel B, right).
Telomere length
Telomere length was measured as the T/S ratio in a linear model with age and education as covariates, df = 3, 45, multiple R2 = 0.04. T/S ratio of the CUD/AUD group was less than the control group (0.93 (± 0.07) vs. 1.13 (± 0.14), i.e., shorter telomeres) but these differences were not statistically significant (t = -1.16, p < 0.26), nor were age (t = -0.50, p < 0.61) and education (t = -0.47, p < 0.64).
Associations with white matter
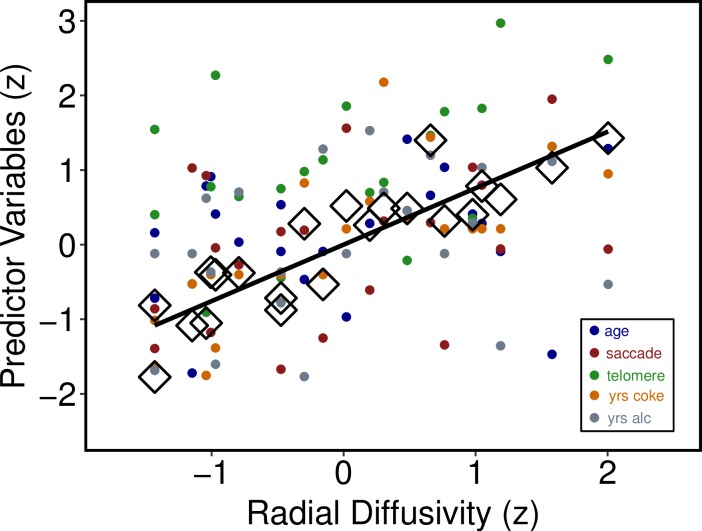
As described above, relationships among RD and cocaine and alcohol use, age, anti-saccades, and telomere length were examined with penalized regression using the elastic net with leave one out cross-validation, which established the optimal α and λ parameters based on RMSE. The best fitting model had the following features: α = 0.10, λ = .019, RMSE = 0.13, and R2 = 0.79. Utilizing the R selectiveInference package as per [62,63], age, anti-saccades (HDDM difference score), telomere length, and years of cocaine use were all important predictors (p < .05), while years of alcohol use was not. Fig 4 depicts the multivariate relationships between RD and the predictors, and Table 2 provides penalized regression coefficients with 95% CI, Z-scores, and p-values for each predictor. Table 2 reveals that years of cocaine use and age were the strongest predictors of white matter integrity as indexed by RD. The Supporting Information (S3 File) provides comprehensive graphical and numerical indices of the elastic net regression parameters and model fits.
Fig 4. Scatterplot of relationships between radial diffusivity and individual predictors in the elastic net regression model.
Within the CUD/AUD group, Fig 4 shows a scatterplot of the relationships between radial diffusivity (x axis) and individual predictors in the elastic net regression model (y-axis): age, anti-saccade drift rate differences (cocaine–non-drug stimuli, see Fig 3), telomere length (T/S ratio), years of cocaine use, and years of alcohol use. Predictors are standardized (z-scored) for graphical interpretability and presentation on a common scale. Large open diamonds (◊) show the predicted points derived from the elastic net model, and the solid black line shows the model-derived line of best fit, R2 = 0.79.
Table 2. Penalized regression coefficients with 95% CI, Z-scores, and p-values for each predictor in the elastic-net regression with DTI radial diffusivity as the outcome variable.
| Variable | Coefficient (95% CI) | Z-score | p-value |
|---|---|---|---|
| Age | 0.375 (0.148–0.595) | 2.862 | 0.004 |
| Anti-Saccade: Drift rate differene |
0.327 (0.088–0.547) | 2.453 | 0.014 |
| Telomere length: T/S ratio |
-0.330 (-0.560 –-0.004) | -2.363 | 0.047 |
| Cocaine use (years) | 0.606 (0.352–1.048) | 3.884 | < 0.001 |
| Alcohol use (years) | 0.075 (0.592 –-0.721) | 0.540 | 0.592 |
Discussion
In this dataset we showed that chronic cocaine and alcohol use were associated with: (1) WM integrity related to duration of cocaine use in extensive WM tracts, and (2) decreased saccadic control in the presence of cocaine-cues compared to control subjects. Additionally, we found that radial diffusivity was predicted by years of cocaine use, age, anti-saccade performance, and telomere length. While each of the predictors will require verification via systematic replication, one interpretation of the collective results is a (partial) depiction of the allostatic load imparted by chronic cocaine and alcohol use.
Studies of this nature are fundamentally constrained by measurement of a limited set of many potential key variables and the ability to address alternative hypotheses, imposing the requisite conclusion that the findings should be considered preliminary. In addition, limitations in sample size and study design likely prevented uncovering pairwise associations among all these individual predictors, if they are indeed related. Accordingly, one might cautiously presuppose that the present results are related to chronic cocaine use plus the additional burden of alcohol abuse (although alcohol use provided no independent predictive utility), plus the influence of unmeasured factors. Such factors are likely to include variables known to alter neurobehavioral trajectories, e.g., trauma exposure, traumatic brain injury, genotypic variation, and prenatal exposure to abused substances and environmental toxicants [12,16,66–69]. Additionally, as noted in the introduction, CUD is most commonly accompanied by the use or abuse of other drugs, including marijuana, alcohol, tobacco, and other stimulants. While we examined the effects of CUD and AUD in the present study, the allostatic burden of a lifetime of polysubstance use warrants greater consideration. Such considerations must account not only for the neurobiological changes imparted by multiple drugs of abuse, but also the accompanying lifestyle and behavior patterns. The modest scope of this study precludes systematic examination of these variables, but larger collaborative efforts should consider an allostatic framework for understanding polysubstance abuse in large multivariate datasets.
With regard to other measurement limitations, markers of HPA-axis, hormone, and immune system activation, as well as hedonic reward deficits are well-established indicators of allostatic load [3,70]. The addition of these markers in the present study would have allowed for analyses of co-variation among established markers and those reported here. Clearly, as work in this area matures, connecting markers like FA/RD and cell aging with markers of HPA-axis, immune system response, and hedonic deficits will advance allostatic load hypotheses in human substance use disorders. One challenge to this aim will be overcoming measurement incongruity. DTI and cell aging (e.g., telomere length) markers tend to be static over the time durations of most experimental work, while HPA-axis and immune responses are dynamic systems subject to phasic changes over short time periods. Nevertheless, bridging these measurement domain stands to advance understanding of allostatic processes in SUD.
Collectively, the data suggest that these variables are possible indicators of CUD/AUD dysregulation in important biobehavioral systems. For chronic SUD, this is consistent with models of allostatis, which “…involves the whole brain and body instead of simply local feedbacks… When demands become chronic, the brain-body system tonically adapts at essentially all levels of organization …” [71]. Notably, duration of cocaine use, anti-saccade performance, and telomere length were all predictors of decreased white matter integrity. Given the study limitations, including the restricted sample, none of the outcomes should be individually considered as strong evidence of allostatic load. However, together the aggregate results suggest a possible allostatic shift associated with chronic cocaine and alcohol use. Duration of cocaine use and telomere length can be considered indicators of chronicity. Previous studies have shown that severity and/or extent of cocaine use (with polysubstance use) was related to decreased WM integrity [12,72], while abstinence from cocaine was related to specific fiber tract improvements in FA value [35,73]. Associations between CUD and reductions in white matter integrity suggest allostatic shifts and possible neurotoxicity to white matter neurons [11,74,75]. These arguments are not fully verifiable based on the present dataset, but provide intriguing hypotheses for systematic replications in broader samples of participants with CUD/AUD. Because the regression analysis was conducted in an exploratory manner, it should be considered hypothesis generating rather than confirmatory of any relationships specified a priori. Moreover, alterations in common WM regions have been observed between substance abuse and other addictions such as gambling [76], raising the alternative explanation of preexisting conditions rather than cocaine-alcohol neurotoxicity. Previous work has established a link between WM impairment (FA, RD) and chronic alcohol abuse [9,13]. The participants in the present dataset had considerably less lifetime alcohol use than typically represented in the alcohol-DTI literature, which may explain why we did not observe independent effects of alcohol use on DTI metrics. Such questions are best addressed by comprehensive longitudinal studies such as the ongoing ABCD project [77].
As AD measures diffusivity running along axons and RD measures the diffusion perpendicular to axons, low AD values have been implicated in internal axonal degeneration [40,41]. Conversely, low RD values have been interpreted as indicators of degeneration of myelin, associated with neurological pathologies, including multiple sclerosis [42], Alzheimer’s [43], and schizophrenia [44]. Indeed, our preclinical work in cocaine-exposed rodents indicates that RD reflects altered myelin integrity [11]. In this context, we observed no relationships between CUD and AD values but significant associations between CUD and RD / FA (R2 = 0.51 and 0.56), providing additional support linking CUD to myelin impairment [11, 78]. Whether these findings are related to direct neurotoxic properties of cocaine on white matter fibers, or water-like edema, or interactions with pro-inflammatory mechanisms (glial cell activation, [79]), intra-axonal injury, CNS stress mechanisms (HPA-axis activation, [6]), or dysregulation of myelin-related gene expression (Myelin Basic Protein, [80]) are unknown. In vitro work at cellular and molecular targets may help reveal the role of these putative mechanisms.
While T/S ratio was shorter in CUD/SUD participants, we did not observe a statistically significant difference from controls. This may represent a limitation of sample size; studies of telomere length in psychiatric or SUD samples have typically examined larger samples [17,18,26,27,81]. Additionally, while the T/S index is well established, more recent measurement techniques involving DNA methylation and mitochondrial DNA offer potentially greater measurement sensitivity [82,83]. However, within the CUD/AUD group, T/S ratio was negatively associated with RD. Reductions in telomere length may indicate common processes in neurodegenerative disease [84].
Collectively, the results add to a growing literature suggesting that chronic cocaine use–and the risk factors associated with a CUD lifestyle–impart an allostatic load measurable across multiple domains of inquiry. While not part of the stock indices of allostatic load (e.g., HPA-axis dysregulation, hypertension, cell aging, oxidative stress), important domains to be considered for future work include white matter integrity, epigenetic changes, neuroimmune mechanisms, and cognitive integrity.
Supporting information
Details for DTI methods, metrics, and analyses.
(PDF)
Individual and group parameter estimates, and statistical and graphical convergence tests from the Hierarchical Bayesian Drift Diffusion Model (HDDM) output of analysis of the anti-saccade data, using the Python HDDM package. For further details, see (1) manuscript text; (2) Wiecki, Sofer & Frank (2013). Frontiers in Neuroinformatics, 7, 1–10: doi:10.3389/fninf.2013.00014; and (3) http://ski.clps.brown.edu/hddm_docs/.
(PDF)
Code, outcome parameters, and graphical information for the penalized regression using the elastic net via the R packages glmnet and selectiveInference.
(PDF)
Details for identified significant white matter (WM) clusters (number and percent) with location of tract label, for FA, MD, and RD values from the TBSS analyses regressing WM metrics and years of cocaine use, controlling for years of alcohol use, age, sex, and education.
(PDF)
Acknowledgments
The authors wish to thank Vipul Kumar Patel, Jessica Vincent, Edward Zuninga, Joseph Alcorn 3rd, and Zahra N. Kamdar for their excellent technical support.
Data Availability
A majority of the aggregate and individual-subject level data are within the paper and its Supporting Information files. Additional files at the individual subject level are available at the Open Science Framework: https://osf.io/ev2xt/.
Funding Statement
This work was supported by National Institute on Drug Abuse [NIDA: https://urldefense.proofpoint.com/v2/url?u=https-3A__www.drugabuse.gov_&d=DwIGaQ&c=6vgNTiRn9_pqCD9hKx9JgXN1VapJQ8JVoF8oWH1AgfQ&r=5vaE3IBw6zz-86SyHJInHsFEiwslapZNIH07dRsjURA&m=K_DJoqSa6wnTYXO7mbeOme1QKtqIm7mAXcPND20GYz8&s=r4NvZd9yoTfIIxkes__I0o3GW9xSaIojjuYmQ0jWkgM&e=] grants DA P50 009262 (JMS, FGM, SDL, PAN), U54DA038999 (FGM) and UL1TR002649 (FGM), the UTHealth [https://med.uth.edu/] McGovern Scholars Award (SDL), and funds from the Center for Neurobehavioral Research on Addictions [https://med.uth.edu/psychiatry/research/centers/addiction/] at the UTHealth McGovern Medical School (JMS, SDL). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.McEwen BS. Allostasis and allostatic load: implications for neuropsychopharmacology. Neuropsychopharmacology. 2000;22(2):108–124. 10.1016/S0893-133X(99)00129-3 [DOI] [PubMed] [Google Scholar]
- 2.George O, Le Moal M, Koob GF. Allostasis and addiction: role of the dopamine and corticotropin-releasing factor systems. Physiol Behav. 2012;106(1):58–64. 10.1016/j.physbeh.2011.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McEwen BS. Brain on stress: how the social environment gets under the skin. Proc Natl Acad Sci U S A. 2012;109 Suppl:17180–17185. 10.1073/pnas.1121254109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ahmed SH, Koob GF. Transition from moderate to excessive drug intake: change in hedonic set point. Science (80-). 1998;282(5387):298–300. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=9765157. [DOI] [PubMed] [Google Scholar]
- 5.Ahmed SH, Kenny PJ, Koob GF, Markou A. Neurobiological evidence for hedonic allostasis associated with escalating cocaine use. Nat Neurosci. 2002;5(7):625–626. 10.1038/nn872 [DOI] [PubMed] [Google Scholar]
- 6.Koob G, Kreek MJ. Stress, dysregulation of drug reward pathways, and the transition to drug dependence. Am J Psychiatry. 2007;164(8):1149–1159. 164/8/1149 [pii] 10.1176/appi.ajp.2007.05030503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Church MW, Holmes PA, Overbeck GW, Tilak JP, Zajac CS. Interactive effects of prenatal alcohol and cocaine exposures on postnatal mortality, development and behavior in the Long-Evans rat. Neurotoxicol Teratol. 1991;13(4):377–386. [DOI] [PubMed] [Google Scholar]
- 8.Koob GF, Volkow ND. Neurobiology of addiction: a neurocircuitry analysis. The lancet Psychiatry. 2016;3(8):760–773. 10.1016/S2215-0366(16)00104-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sullivan E V, Harris RA, Pfefferbaum A. Alcohol’s effects on brain and behavior. Alcohol Res Health. 2010;33(1–2):127–143. [PMC free article] [PubMed] [Google Scholar]
- 10.Bierut LJ, Strickland JR, Thompson JR, Afful SE, Cottler LB. Drug use and dependence in cocaine dependent subjects, community-based individuals, and their siblings. Drug Alcohol Depend. 2008;95(1–2):14–22. 10.1016/j.drugalcdep.2007.11.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Narayana PA, Herrera JJ, Bockhorst KH, et al. Chronic cocaine administration causes extensive white matter damage in brain: diffusion tensor imaging and immunohistochemistry studies. Psychiatry Res. 2014;221(3):220–230. 10.1016/j.pscychresns.2014.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kaag AM, van Wingen GA, Caan MWA, Homberg JR, van den Brink W, Reneman L. White matter alterations in cocaine users are negatively related to the number of additionally (ab)used substances. Addict Biol. 2017;22(4):1048–1056. 10.1111/adb.12375 [DOI] [PubMed] [Google Scholar]
- 13.Pfefferbaum A, Rosenbloom MJ, Chu W, et al. White matter microstructural recovery with abstinence and decline with relapse in alcohol dependence interacts with normal ageing: a controlled longitudinal DTI study. The lancet Psychiatry. 2014;1(3):202–212. 10.1016/S2215-0366(14)70301-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marks KR, Roberts W, Stoops WW, Pike E, Fillmore MT, Rush CR. Fixation time is a sensitive measure of cocaine cue attentional bias. Addiction. 2014;109(9):1501–1508. 10.1111/add.12635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dias NR, Schmitz JM, Rathnayaka N, et al. Anti-saccade error rates as a measure of attentional bias in cocaine dependent subjects. Behav Brain Res. 2015;292 10.1016/j.bbr.2015.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Levandowski ML, Tractenberg SG, de Azeredo LA, et al. Crack cocaine addiction, early life stress and accelerated cellular aging among women. Prog Neuropsychopharmacol Biol Psychiatry. 2016;71:83–89. 10.1016/j.pnpbp.2016.06.009 [DOI] [PubMed] [Google Scholar]
- 17.Fyhrquist F, Saijonmaa O. Telomere length and cardiovascular aging. Ann Med. 2012;44 Suppl 1:S138–42. 10.3109/07853890.2012.660497 [DOI] [PubMed] [Google Scholar]
- 18.Pavanello S, Hoxha M, Dioni L, et al. Shortened telomeres in individuals with abuse in alcohol consumption. Int J cancer. 2011;129(4):983–992. 10.1002/ijc.25999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Roman CAF, Arnett PA. Structural brain indices and executive functioning in multiple sclerosis: A review. J Clin Exp Neuropsychol. 2016;38(3):261–274. 10.1080/13803395.2015.1105199 [DOI] [PubMed] [Google Scholar]
- 20.Tomimoto H. White matter integrity and cognitive dysfunction: Radiological and neuropsychological correlations. Geriatr Gerontol Int. 2015;15 Suppl 1:3–9. 10.1111/ggi.12661 [DOI] [PubMed] [Google Scholar]
- 21.Crawford TJ, Higham S, Renvoize T, et al. Inhibitory control of saccadic eye movements and cognitive impairment in Alzheimer’s disease. Biol Psychiatry. 2005;57(9):1052–1060. 10.1016/j.biopsych.2005.01.017 [DOI] [PubMed] [Google Scholar]
- 22.Abel LA, Levin S, Holzman PS. Abnormalities of smooth pursuit and saccadic control in schizophrenia and affective disorders. Vision Res. 1992;32(6):1009–1014. [DOI] [PubMed] [Google Scholar]
- 23.Tessitore A, Giordano A, Russo A, Tedeschi G. Structural connectivity in Parkinson’s disease. Parkinsonism Relat Disord. 2016;22 Suppl 1:S56–9. 10.1016/j.parkreldis.2015.09.018 [DOI] [PubMed] [Google Scholar]
- 24.Tamnes CK, Agartz I. White Matter Microstructure in Early-Onset Schizophrenia: A Systematic Review of Diffusion Tensor Imaging Studies. J Am Acad Child Adolesc Psychiatry. 2016;55(4):269–279. 10.1016/j.jaac.2016.01.004 [DOI] [PubMed] [Google Scholar]
- 25.O’Donoghue S, Holleran L, Cannon DM, McDonald C. Anatomical dysconnectivity in bipolar disorder compared with schizophrenia: A selective review of structural network analyses using diffusion MRI. J Affect Disord. 2017;209:217–228. 10.1016/j.jad.2016.11.015 [DOI] [PubMed] [Google Scholar]
- 26.Lindqvist D, Epel ES, Mellon SH, et al. Psychiatric disorders and leukocyte telomere length: Underlying mechanisms linking mental illness with cellular aging. Neurosci Biobehav Rev. 2015;55:333–364. 10.1016/j.neubiorev.2015.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Darrow SM, Verhoeven JE, Revesz D, et al. The Association Between Psychiatric Disorders and Telomere Length: A Meta-Analysis Involving 14,827 Persons. Psychosom Med. 2016;78(7):776–787. 10.1097/PSY.0000000000000356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rizvi S, Raza ST, Mahdi F. Telomere length variations in aging and age-related diseases. Curr Aging Sci. 2014;7(3):161–167. [DOI] [PubMed] [Google Scholar]
- 29.Eitan E, Hutchison ER, Mattson MP. Telomere shortening in neurological disorders: an abundance of unanswered questions. Trends Neurosci. 2014;37(5):256–263. 10.1016/j.tins.2014.02.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chan F, Armstrong IT, Pari G, Riopelle RJ, Munoz DP. Deficits in saccadic eye-movement control in Parkinson’s disease. Neuropsychologia. 2005;43(5):784–796. 10.1016/j.neuropsychologia.2004.06.026 [DOI] [PubMed] [Google Scholar]
- 31.Schmitz JM, Green CE, Hasan KM, et al. PPAR-gamma agonist pioglitazone modifies craving intensity and brain white matter integrity in patients with primary cocaine use disorder: A double-blind randomized controlled pilot trial. Addiction. 2017. 10.1111/add.13868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Moeller FG, Hasan KM, Steinberg JL, et al. Diffusion tensor imaging eigenvalues: preliminary evidence for altered myelin in cocaine dependence. Psychiatry Res. 2007;154(3):253–258. S0925-4927(06)00198-3 [pii] 10.1016/j.pscychresns.2006.11.004 [DOI] [PubMed] [Google Scholar]
- 33.Lane SD, Steinberg JL, Ma L, et al. Diffusion tensor imaging and decision making in cocaine dependence. PLoS One. 2010;5(7). 10.1371/journal.pone.0011591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lim KO, Wozniak JR, Mueller BA, et al. Brain macrostructural and microstructural abnormalities in cocaine dependence. Drug Alcohol Depend. 2008;92(1–3):164–172. S0376-8716(07)00288-8 [pii] 10.1016/j.drugalcdep.2007.07.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Xu J, Devito EE, Worhunsky PD, Carroll KM, Rounsaville BJ, Potenza MN. White Matter Integrity is Associated with Treatment Outcome Measures in Cocaine Dependence. Neuropsychopharmacology. 2010;35(7):1541–1549. 10.1038/npp.2010.25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shipley WC, Gruber CP, Martin TA, Klein AM. Shipley-2: Manual. Los Angeles, CA: Western Psychological Services; 2009. [Google Scholar]
- 37.First MB, Gibbon M, Spitzer RL, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition. New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- 38.McLellan AT, Kushner H, Metzger D, et al. The Fifth Edition of the Addiction Severity Index. J Subst Abus Treat. 1992;9(3):199–213. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=1334156. [DOI] [PubMed] [Google Scholar]
- 39.Kellogg SH, McHugh PF, Bell K, et al. The Kreek-McHugh-Schluger-Kellogg scale: a new, rapid method for quantifying substance abuse and its possible applications. Drug Alcohol Depend. 2003;69(2):137–150. doi:S0376871602003083 [pii] [DOI] [PubMed] [Google Scholar]
- 40.Song S-K, Sun S-W, Ju W-K, Lin S-J, Cross AH, Neufeld AH. Diffusion tensor imaging detects and differentiates axon and myelin degeneration in mouse optic nerve after retinal ischemia. Neuroimage. 2003;20(3):1714–1722. [DOI] [PubMed] [Google Scholar]
- 41.Song S, Sun S, Ramsbottom MJ, Chang C, Russell J, Cross AH. Dysmyelination revealed through MRI as increased radial (but unchanged axial) diffusion of water. 2002;1436:1429–1436. 10.1006/nimg.2002.1267 [DOI] [PubMed] [Google Scholar]
- 42.Sbardella E, Tona F, Petsas N, Pantano P. DTI Measurements in Multiple Sclerosis: Evaluation of Brain Damage and Clinical Implications. Mult Scler Int. 2013;2013:671730 10.1155/2013/671730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nir TM, Jahanshad N, Villalon-Reina JE, et al. Effectiveness of regional DTI measures in distinguishing Alzheimer’s disease, MCI, and normal aging. NeuroImage Clin. 2013;3:180–195. 10.1016/j.nicl.2013.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lee S-H, Kubicki M, Asami T, et al. Extensive white matter abnormalities in patients with first-episode schizophrenia: a Diffusion Tensor Imaging (DTI) study. Schizophr Res. 2013;143(2–3):231–238. 10.1016/j.schres.2012.11.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jenkinson M, Beckmann CF, Behrens TE, Woolrich MW, Smith SM. FSL. Neuroimage. 2012;62:782–790. 10.1016/j.neuroimage.2011.09.015 [DOI] [PubMed] [Google Scholar]
- 46.Smith SM, Jenkinson M, Woolrich MW, et al. Advances in functional and structural MR image analysis and implementation as FSL. Neuroimage. 2004;23 Suppl 1:S208–19. 10.1016/j.neuroimage.2004.07.051 [DOI] [PubMed] [Google Scholar]
- 47.Smith SM, Jenkinson M, Johansen-Berg H, et al. Tract-based spatial statistics: voxelwise analysis of multi-subject diffusion data. Neuroimage. 2006;31(4):1487–1505. 10.1016/j.neuroimage.2006.02.024 [DOI] [PubMed] [Google Scholar]
- 48.Winkler AM, Ridgway GR, Webster MA, Smith SM, Nichols TE. Permutation inference for the general linear model. Neuroimage. 2014;92:381–397. 10.1016/j.neuroimage.2014.01.060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hutton SB, Ettinger U. The Antisaccade Task as a Research Tool in Psychopathology: A Critical Review. 2004;(1):1–37. [DOI] [PubMed] [Google Scholar]
- 50.Shaikh AG, Zee DS. Eye Movement Research in the Twenty-First Century-a Window to the Brain, Mind, and More. Cerebellum. December 2017. 10.1007/s12311-017-0910-5 [DOI] [PubMed] [Google Scholar]
- 51.Field M, Marhe R, Franken IH. The clinical relevance of attentional bias in substance use disorders. CNS Spectr. 2014;19(3):225–230. 10.1017/S1092852913000321 [DOI] [PubMed] [Google Scholar]
- 52.Marks KR, Pike E, Stoops WW, Rush CR. The magnitude of drug attentional bias is specific to substance use disorder. Psychol Addict Behav. 2015;29(3):690–695. 10.1037/adb0000084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wiecki T V, Sofer I, Frank MJ. HDDM: Hierarchical Bayesian estimation of the Drift-Diffusion Model in Python. Front Neuroinform. 2013;7:14 10.3389/fninf.2013.00014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lee MD, Wagenmakers E-J. Bayesian Cognitive Modeling. Cambridge, UK: Cambridge University Press; 2013. [Google Scholar]
- 55.Cavanagh JF, Wiecki T V, Kochar A, Frank MJ. Eye tracking and pupillometry are indicators of dissociable latent decision processes. J Exp Psychol Gen. 2014;143(4):1476–1488. 10.1037/a0035813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zhang J, Rowe JB. Dissociable mechanisms of speed-accuracy tradeoff during visual perceptual learning are revealed by a hierarchical drift-diffusion model. Front Neurosci. 2014;8:69 10.3389/fnins.2014.00069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cawthon RM. Telomere measurement by quantitative PCR. Nucleic Acids Res. 2002;30(10):e47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Steinley D, Lane SP, Sher KJ. Determining optimal diagnostic criteria through chronicity and comorbidity. silico Pharmacol. 2016;4(1):1 10.1186/s40203-016-0015-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Pocock SJ, Assmann SE, Enos LE, Kasten LE. Subgroup analysis, covariate adjustment and baseline comparisons in clinical trial reporting: current practice and problems. Stat Med. 2002;21(19):2917–2930. 10.1002/sim.1296 [DOI] [PubMed] [Google Scholar]
- 60.Friedman J, Hastie T, Tibshirani R. Regularization Paths for Generalized Linear Models via Coordinate Descent. J Stat Softw. 2010;33(1):1–22. [PMC free article] [PubMed] [Google Scholar]
- 61.Hastie T, Tibshirani R, Friedman J. The Elements of Statistical Learning: Data Mining, Inference, and Prediction. Stanford, CA: Springer-Verlag; 2009. [Google Scholar]
- 62.Finch WH, Finch MEH. Regularization Methods for Fitting Linear Models with Small Sample Sizes: Fitting the Lasso Estimator using R. Pract Assessment, Res Eval. 2016;21(7):1–13. http://www.pareonline.net/getvn.asp?v=21&n=7. [Google Scholar]
- 63.R Core Team (2013). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria: ISBN 3-900051-07-0, URL http://www.R-project.org/. [Google Scholar]
- 64.Tibshirani R, Tibshirani R, Taylor J, Loftusm J, Reid S. Package ‘selectiveInference.’ 2017.https://cran.rproject.org/web/packages/selectiveInference/selectiveInference.pdf
- 65.Aung WY, Mar S, Benzinger TL. Diffusion tensor MRI as a biomarker in axonal and myelin damage. Imaging Med. 2013;5(5):427–440. 10.2217/iim.13.49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ma L, Steinberg JL, Keyser-marcus L, et al. Altered white matter in cocaine-dependent subjects with traumatic brain injury: A diffusion tensor imaging study *. 2015:128–134. 10.1016/j.drugalcdep.2015.03.015.Altered [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Morie KP, Yip SW, Zhai ZW, et al. White-matter crossing-fiber microstructure in adolescents prenatally exposed to cocaine. Drug Alcohol Depend. 2017;174:23–29. 10.1016/j.drugalcdep.2017.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Miller MM, Meyer AE, Sprowles JLN, Sable HJK. Cocaine self-administration in male and female rats perinatally exposed to PCBs: Evaluating drug use in an animal model of environmental contaminant exposure. Exp Clin Psychopharmacol. 2017;25(2):114–124. 10.1037/pha0000113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Zakiniaeiz Y, Yip SW, Balodis IM, et al. Altered functional connectivity to stressful stimuli in prenatally cocaine-exposed adolescents. Drug Alcohol Depend. 2017;180:129–136. 10.1016/j.drugalcdep.2017.07.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Koob G, Kreek MJ. Stress, dysregulation of drug reward pathways, and the transition to drug dependence. Am J Psychiatry. 2007;164(8):1149–1159. 10.1176/appi.ajp.2007.05030503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Koob GF, Le Moal M. Drug addiction, dysregulation of reward, and allostasis. Neuropsychopharmacology. 2001;24(2):97–129. 10.1016/S0893-133X(00)00195-0 [DOI] [PubMed] [Google Scholar]
- 72.van Son D, Wiers RW, Catena A, Perez-Garcia M, Verdejo-Garcia A. White matter disruptions in male cocaine polysubstance users: Associations with severity of drug use and duration of abstinence. Drug Alcohol Depend. 2016;168:247–254. 10.1016/j.drugalcdep.2016.09.023 [DOI] [PubMed] [Google Scholar]
- 73.Bell RP, Foxe JJ, Nierenberg J, Hoptman MJ, Garavan H. Assessing white matter integrity as a function of abstinence duration in former cocaine-dependent individuals. Drug Alcohol Depend. 2011;114(2–3):159–168. 10.1016/j.drugalcdep.2010.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mohammad Ahmadi Soleimani S, Ekhtiari H, Cadet JL. Drug-induced neurotoxicity in addiction medicine: From prevention to harm reduction. Prog Brain Res. 2016;223:19–41. 10.1016/bs.pbr.2015.07.004 [DOI] [PubMed] [Google Scholar]
- 75.Feng Y. Convergence and divergence in the etiology of myelin impairment in psychiatric disorders and drug addiction. Neurochem Res. 2008;33(10):1940–1949. 10.1007/s11064-008-9693-x [DOI] [PubMed] [Google Scholar]
- 76.Yip SW, Morie KP, Xu J, et al. Shared microstructural features of behavioral and substance addictions revealed in areas of crossing fibers. Biol psychiatry Cogn Neurosci neuroimaging. 2017;2(2):188–195. 10.1016/j.bpsc.2016.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Volkow ND, Koob GF, Croyle RT, et al. The conception of the ABCD study: From substance use to a broad NIH collaboration. Dev Cogn Neurosci. October 2017. 10.1016/j.dcn.2017.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Periyasamy P, Guo M-L, Buch S. Cocaine induces astrocytosis through ER stress-mediated activation of autophagy. Autophagy. 2016;12(8):1310–1329. 10.1080/15548627.2016.1183844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Nielsen DA, Huang W, Hamon SC, et al. Forced abstinence from cocaine self-administration is associated with DNA methylation changes in myelin genes in the corpus callosum: A preliminary study. Front Psychiatry. 2012;3(JUN):1–9. 10.3389/fpsyt.2012.00060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Albertson DN, Pruetz B, Schmidt CJ, Kuhn DM, Kapatos G, Bannon MJ. Gene expression profile of the nucleus accumbens of human cocaine abusers: evidence for dysregulation of myelin. J Neurochem. 2004;88(5):1211–1219. 2247 [pii] 10.1046/j.1471-4159.2003.02247.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ahrens KA, Rossen LM, Simon AE. Relationship Between Mean Leucocyte Telomere Length and Measures of Allostatic Load in US Reproductive-Aged Women, NHANES 1999–2002. Paediatr Perinat Epidemiol. 2016;30(4):325–335. 10.1111/ppe.12277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Jones MJ, Goodman SJ, Kobor MS. DNA methylation and healthy human aging. Aging Cell. 2015;14(6):924–932. 10.1111/acel.12349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Chistiakov DA, Sobenin IA, Revin V V, Orekhov AN, Bobryshev Y V. Mitochondrial aging and age-related dysfunction of mitochondria. Biomed Res Int. 2014;2014:238463 10.1155/2014/238463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kota LN, Bharath S, Purushottam M, et al. Reduced telomere length in neurodegenerative disorders may suggest shared biology. J Neuropsychiatry Clin Neurosci. 2015;27(2):e92–6. 10.1176/appi.neuropsych.13100240 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Details for DTI methods, metrics, and analyses.
(PDF)
Individual and group parameter estimates, and statistical and graphical convergence tests from the Hierarchical Bayesian Drift Diffusion Model (HDDM) output of analysis of the anti-saccade data, using the Python HDDM package. For further details, see (1) manuscript text; (2) Wiecki, Sofer & Frank (2013). Frontiers in Neuroinformatics, 7, 1–10: doi:10.3389/fninf.2013.00014; and (3) http://ski.clps.brown.edu/hddm_docs/.
(PDF)
Code, outcome parameters, and graphical information for the penalized regression using the elastic net via the R packages glmnet and selectiveInference.
(PDF)
Details for identified significant white matter (WM) clusters (number and percent) with location of tract label, for FA, MD, and RD values from the TBSS analyses regressing WM metrics and years of cocaine use, controlling for years of alcohol use, age, sex, and education.
(PDF)
Data Availability Statement
A majority of the aggregate and individual-subject level data are within the paper and its Supporting Information files. Additional files at the individual subject level are available at the Open Science Framework: https://osf.io/ev2xt/.