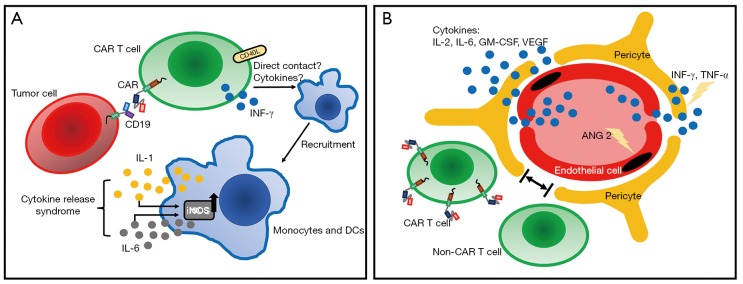
Figure 2.
Models of CRS and neurologic toxicities. (A) CRS is mediated by CAR T cells and bystander immune cells such as monocytes and DCs. In the peripheral blood, when CAR T cells and tumor cells are engaged, CAR T cells are activated and start recruiting monocytes through direct contact such as CD40L-CD40 interaction, or through T-cell derived cytokines such as INF-γ. Activated monocytes can secrete key CRS cytokines IL-1 and IL-6, which in addition to cause symptoms of CRS, can further activate monocytes through iNOS. (B) Neurologic toxicities are caused by cytokines and/or CAR T and non-CAR T cells, secondary to increased BBB permeability. BBB is comprised of ECs and pericytes. Following increased levels of cytokines during CRS, ECs are activated with secretion of angiopoietin 2 (ANG2), which further promotes endothelial activation and microvascular permeability. Next, cytokines such as INF-γ and TNF-α can cross ECs and cause pericyte stress, further increasing BBB permeability. Analysis of CSF showed high levels of IL-2, IL-6, GM-CSF and VEGF, as well as CAR T cells and non-CAR T cells. CRS, cytokine release syndrome; CAR, chimeric antigen receptor; DC, dendritic cell; iNOS, inducible nitric oxide synthase; BBB, blood-brain barrier; EC, endothelial cells; CSF, cerebrospinal fluid.