Abstract
Implant placement is a challenge in the anterior maxilla if the available bone is reduced and esthetics is challenging. The ideal implant position should be considered in all three dimensions: mesiodistal, apicocoronal, and orofacial. This article includes a review and a case report for the anatomical and clinical perspective of implant placement in nasopalatine foramen (near incisal canal). In this case report, the edentulous space is mutilated in between the area #12 and #21 teeth. Therefore, only one, 3.0 W/10.00 L implant (bone size 4.2 mm width and 11 mm length) could be placed. Radiographically, D2 bone quality was diagnosed. Before surgery, an emphasis was given over the proper implant selection to avoid oversized implants due to critical anatomical landmark. Careful and with minimal trauma, the soft tissue was handled and implant placement was performed in a proper position, using information from panoramic radiograph, 3-D Dentascan. A surgical guide was used for placement of the implant. Finally, immediate loading of temporary implant prosthesis was done. The primary outcome was satisfactory, as after 72 h, no swelling and numbness were reported. The patient has been recalled after healing period of 24 weeks for permanent restoration.
Keywords: Bone expansion, dental implants, esthetics, imaging modalities, nasopalatine foramen region
INTRODUCTION
Implant rehabilitation of the edentulous anterior maxilla remains one of the most complex restorative challenges because of several variables that affect the esthetic and functional aspects of prostheses. The intricate preexisting anatomy dictates meticulous and accurate osteotomy planning into a premaxilla reconstruction.[1,2,3] In the postextraction phase,[4,5] the high resorption rate of the maxilla could be jeopardized with the surgical osteotomy preparation and prosthesis retention. With progressive bone loss, the alveolar crest may approach to the anatomic structures. The nasopalatine nerve and vessels emerge from the crest of the ridge with palatal migration of the anterior maxillary alveolus. Careful consideration is necessary when an implant is positioned in the maxillary central incisors because of the proximity of the nasopalatine canal (incisive canal) and its contents. Difficulties and anatomic limitations regarding the location of the nasopalatine canal in relation to maxillary central incisor implants have been reported.[6] In 4% of the computed tomographic scans, the canal size was an impediment for placing root-form implants in this area. Augmentation of the area before or at the same time as implant placement is indicated in cases, in which the nasopalatine foramen is in proximity to the location of the future osteotomy.[7,8,9]
The nasopalatine canal is described as being located in the midline of the palate, posterior to the central maxillary incisors.[10] The funnel-shaped oral opening of the canal in the midline of the anterior palate is known as the incisive foramen and is usually located immediately below the incisal papilla.
The canal divides further into two canals on its way to the nasal cavity and terminates at the nasal floor with one or two openings, the foramina of Stenson, at either side of the septum.[11] The canal contains the nasopalatine (incisal) nerve and the terminal branch of the descending nasopalatine artery, as well as fibrous connective tissue, fat, and even small salivary glands.[12,13] Nevertheless, anatomical variations of the nasopalatine canal are not very well documented in the literature. The average nasopalatine foramen is 4.6 mm wide and is located 7.4 mm from the labial surface of a nonresorbed ridge. The nasopalatine canal (mean length, 8.1 mm) exits at the incisal foramen.
The anatomic variants of the canal were differentiated into three groups [Figure 1] in the vein of (a) a single canal, (b) two parallel canals, (c) variations of the Y-type of canal with one oral/palatal opening (¼ incisal foramen) and two or more nasal openings (¼ foramina of Stenson).[14]
Figure 1.
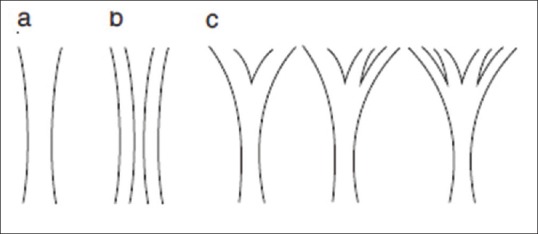
Classification of anatomic variations of the nasopalatine
In the case reported here, the incisal foramen had to be used for implant placement because the mesiodistal space between the both laterals was strongly reduced, leaving space only for one implant and one tooth thereon.
CASE REPORT
A 19-year-old male reported for the replacement of anterior missing teeth. On intraoral examination, two teeth were missing #12 and #21 in the maxilla. A mutilated edentulous space for only a single tooth was present. Mandibular arch was completely dentulous [Figure 2]. Clinical and radiographic examination revealed that remaining teeth were periodontally sound with no mobility and periapical pathology [Figure 3]. Various prosthetic treatment modalities were explained to the patient. Among the treatment options, the patient decided for a fixed prosthesis on a single implant.
Figure 2.

Upper/lower cast
Figure 3.

Intraoral periapical X-ray; #12 and #21 regions
Proper case history of the patient was recorded including medical history which was noncontributory. A routine blood investigation and dental and oral examination were also carried out. Diagnostic impressions and casts were prepared. Dentascan was done to evaluate the dimensions of available bone and an appropriate-sized implant [Figure 4]. Dentascan revealed that edentulous space between two missing central incisors was only 8.5 mm mesiodistally while bone was 4.2 mm in width and 11 mm in length, sagittally and coronally, respectively [Figures 4 and 5]. Adin Touareg-S 3 W/10 L implant was decided for placement. A surgical template in the form of conventional removable partial denture was prepared along with gutta-percha radiographic marker. Subsequently, the position of implant was decided before the surgery.
Figure 4.
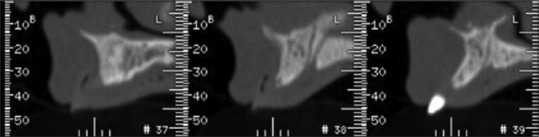
Dentascan (coronal view): with gutta radiographic marker
Figure 5.

Dentascan; orthopantomography view
Surgical phase
A full mucoperiosteal surgical flap protocol was planned. Preoperative antibiotics (combination of amoxicillin-250 mg, cloxacillin-250 mg and clavulanic acid-125 mg before ½ h) were given to the patient. Local anesthesia was infiltrated in incisive foramina and into the buccal sulcus. Incision was made beyond the boundary of incisive papilla [Figures 6–8]. With the help of template placed on the crest of the ridge, lance (1.5 mm) and pilot drill (2 mm) were used for marking the point for implant placement [Figure 9]. Paralleling tool was placed to check for angulations of the implant [Figure 10]. Sequential drilling was not done because a protocol of bone expansion is followed [Figures 11 and 12]. Transmucosal extension (healing abutment) was given for 24 h [Figure 13]. Postoperatively, radiograph showed a well placed single implant [Figure 14]. The patient was kept under postoperative care which included administration of antibiotics (combination of amoxicillin-250 mg, cloxacillin-250 mg, and clavulanic acid-125 mg, TDS for 5 days), analgesics (diclofenac sodium 50 mg + paracetamol 500 mg, SOS), metrogyl (400 mg BD for 3 days), and noninflammatory enzymes as trypsin and chymotrypsin along with probiotics. Maintenance of oral hygiene emphasized means of mouthwash. Immediate loading was done after 48 h by a temporary self cure acrylic prosthesis without any occlusal or functional contact [Figure 15]. After 6 months, the final all ceramic crown was fabricated and delivered [Figure 16].
Figure 6.
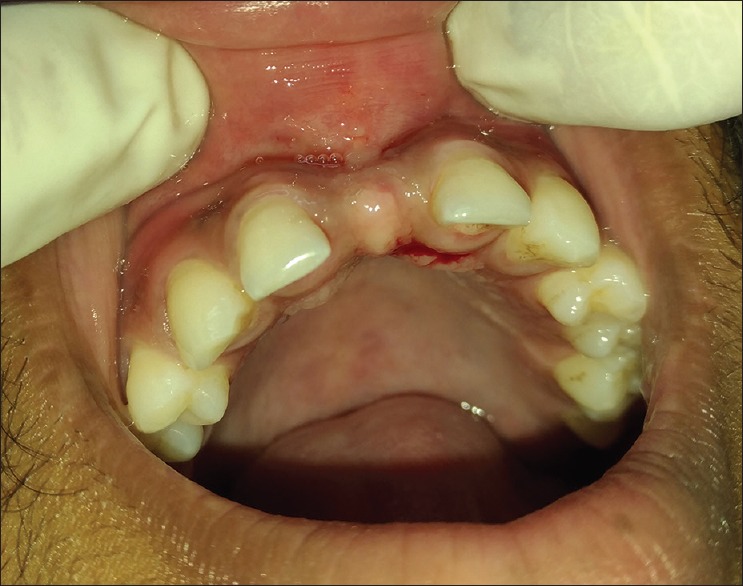
Preoperative
Figure 8.
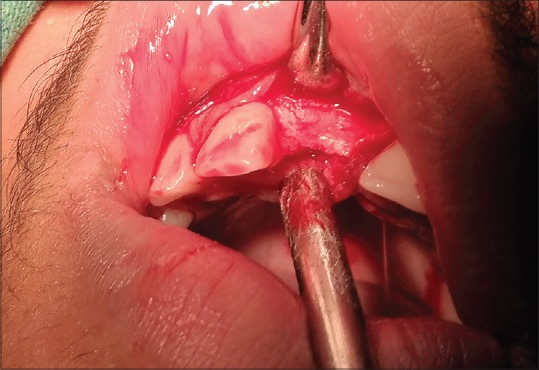
Surgical – Incisal view
Figure 9.

Pilot drill aspect
Figure 10.

Parallel pin
Figure 11.

Bone expander – Tip 1.6 mm to crest 2.6 mm
Figure 12.

Bone expander at surgical site
Figure 13.

Per mucosal extension
Figure 14.

Intraoral periapical X-ray, after surgery
Figure 15.

Temporary prosthesis
Figure 16.

Final prosthesis with all-ceramic zirconia crown
Figure 7.

Mucoperiosteal flap (reflection view) showing incisive foramina
DISCUSSION
A large incisive canal (mean canal length was 10.86–2.67 mm, and mean diameter was 2.59–0.91 mm[15]) may be an obstacle to implant placement in the central incisor region. Whenever a large canal is present, it generally results in some numbness of the anterior palatal tissue, after implant surgery. In some other cases, missing facial bone wall (during surgery) may be augmented using a proper surgical technique, such as guided bone regeneration with barrier membranes and appropriate bone grafts and/or bone substitutes.
The potential factor of esthetic implant “emerging profile” was reviewed on the basis such as horizontal or vertical bone deficiencies and iatrogenic factors such as improper implant selection and malpositioning of dental implant.
In this case report, a buccal bony cortical plate expansion is done by bone expanders (dimensions: tip 1.6 mm and crest 2.6 mm) and also by the self-drilling of implant. The bone expansion helps in osseodensification which provides in good osseointegration.[16] This perspective will keep the implant buccally and prevent pressure on the nasopalatine fossa (Authors gave and advocate more pressure on buccal wall and less pressure on lingual wall at the time of osseodensification). Preplanning and review of anatomy of the region before surgical procedures helped to avoid the problems.[17] Subsequently, in three dimensions such as mesiodistally, buccolingually, and apicocoronally, the implant was well placed. However, if after tooth extractions and with age the maxilla atrophies in all directions, the nasopalatine canal tends to enlarge itself in all dimensions (as a result of exactly this 3D-atrophy). The palatal opening (the incisive foramen) enlarges by a mean of 32% and may occupy up to 58% of the alveolar ridge width in the potential area of the two central incisor implants.[15] Therefore, smaller-sized implants are a solution to anterior maxilla (Adin Touareg-S 3 W/10 L implant).
CONCLUSIONS
Familiarity, with the anatomic structures pertaining to dental Implantology, is critically important. In this case report, implant is placed adjacent to nasopalatine canal, and at the same time, buccal plate was expanded so as to maintain the width of the bone. A surgical template was utilized for reaching the desired position and orientation of the dental implant. Dentascan provided the visualized information of the maxillary arch in cross-sectional and tangential/panoramic images that enabled the accurate preprosthetic treatment planning. The case proved to be a success owing to the coordinated teamwork of a radiologist, a maxillofacial surgeon, and a prosthodontist.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Hoffmann KD. Anatomic considerations in the partially and fully edentulous maxilla. Atlas Oral Maxillofac Surg Clin North Am. 1994;2:31–9. [PubMed] [Google Scholar]
- 2.Buser D, Martin W, Belser UC. Optimizing esthetics for implant restorations in the anterior maxilla: Anatomic and surgical considerations. Int J Oral Maxillofac Implants. 2004;19(Suppl):43–61. [PubMed] [Google Scholar]
- 3.Bosse LP, Taylor TD. Problems associated with implant rehabilitation of the edentulous maxilla. Dent Clin North Am. 1998;42:117–27. [PubMed] [Google Scholar]
- 4.Carlsson GE, Bergman B, Hedegård B. Changes in contour of the maxillary alveolar process under immediate dentures. A longitudinal clinical and x-ray cephalometric study covering 5 years. Acta Odontol Scand. 1967;25:45–75. doi: 10.3109/00016356709072522. [DOI] [PubMed] [Google Scholar]
- 5.Atwood DA. Some clinical factors related to rate of resorption of residual ridges. J Prosthet Dent. 1962;12:441–50. doi: 10.1067/mpr.2001.117609. [DOI] [PubMed] [Google Scholar]
- 6.Kraut RA, Boyden DK. Location of incisive canal in relation to central incisor implants. Implant Dent. 1998;7:221–5. doi: 10.1097/00008505-199807030-00010. [DOI] [PubMed] [Google Scholar]
- 7.Rosenquist JB, Nyström E. Occlusion of the incisal canal with bone chips. A procedure to facilitate insertion of implants in the anterior maxilla. Int J Oral Maxillofac Surg. 1992;21:210–1. doi: 10.1016/s0901-5027(05)80220-6. [DOI] [PubMed] [Google Scholar]
- 8.Scher EL. Use of the incisive canal as a recipient site for root form implants: Preliminary clinical reports. Implant Dent. 1994;3:38–41. doi: 10.1097/00008505-199404000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Artzi Z, Nemcovsky CE, Bitlitum I, Segal P. Displacement of the incisive foramen in conjunction with implant placement in the anterior maxilla without jeopardizing vitality of nasopalatine nerve and vessels: A novel surgical approach. Clin Oral Implants Res. 2000;11:505–10. doi: 10.1034/j.1600-0501.2000.011005505.x. [DOI] [PubMed] [Google Scholar]
- 10.Jacobs R, Lambrichts I, Liang X, Martens W, Mraiwa N, Adriaensens P, et al. Neurovascularization of the anterior jaw bones revisited using high-resolution magnetic resonance imaging. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:683–93. doi: 10.1016/j.tripleo.2006.11.014. [DOI] [PubMed] [Google Scholar]
- 11.Radlanski RJ, Emmerich S, Renz H. Prenatal morphogenesis of the human incisive canal. Anat Embryol (Berl) 2004;208:265–71. doi: 10.1007/s00429-004-0389-y. [DOI] [PubMed] [Google Scholar]
- 12.Keith DA. Phenomenon of mucous retention in the incisive canal. J Oral Surg. 1979;37:832–4. [PubMed] [Google Scholar]
- 13.Liang X, Jacobs R, Martens W, Hu Y, Adriaensens P, Quirynen M, et al. Macro- and micro-anatomical, histological and computed tomography scan characterization of the nasopalatine canal. J Clin Periodontol. 2009;36:598–603. doi: 10.1111/j.1600-051X.2009.01429.x. [DOI] [PubMed] [Google Scholar]
- 14.Greenstein G, Cavallaro J, Tarnow D. Practical application of anatomy for the dental implant surgeon. J Periodontol. 2008;79:1833–46. doi: 10.1902/jop.2008.080086. [DOI] [PubMed] [Google Scholar]
- 15.Tözüm TF, Güncü GN, Yıldırım YD, Yılmaz HG, Galindo-Moreno P, Velasco-Torres M, et al. Evaluation of maxillary incisive canal characteristics related to dental implant treatment with computerized tomography: A clinical multicenter study. J Periodontol. 2012;83:337–43. doi: 10.1902/jop.2011.110326. [DOI] [PubMed] [Google Scholar]
- 16.Pai UY, Rodrigues SJ, Talreja KS, Mundathaje M. Osseodensification – A novel approach in implant dentistry. J Indian Prosthodont Soc. 2018;18:196–200. doi: 10.4103/jips.jips_292_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bornstein MM, Balsiger R, Sendi P, von Arx T. Morphology of the nasopalatine canal and dental implant surgery: A radiographic analysis of 100 consecutive patients using limited cone-beam computed tomography. Clin Oral Implants Res. 2011;22:295–301. doi: 10.1111/j.1600-0501.2010.02010.x. [DOI] [PubMed] [Google Scholar]


