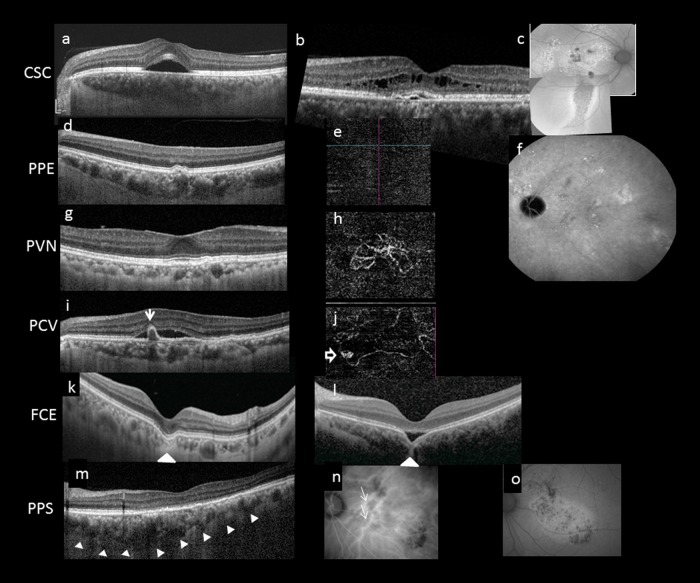
Fig. 2.
Multimodal imaging features of pachychoroid disease. Several clinical manifestations have been described to reside within the pachychoroid disease spectrum, including central serous chorioretinopathy (CSC) (a–c), pachychoroid pigment epitheliopathy (PPE) (d–f), pachychoroid neovasculopathy (PVN) (g, h), polypoidal choroidal vasculopathy (PCV)/aneurysmal type 1 neovascularization (AT1) (i, j), focal choroidal excavation (FCE) (k, l), and peripapillary pachchoroid syndrome (PPS) (m–o). Note that the choroidal features described in Fig. 1 can be seen in all cases in Fig. 2. In acute CSC (a), a solitary neurosensory detachment is commonly seen. In contrast, in chronic CSC (b), the neurosensory detachment tends to be shallower and broader. A shallow pigment epithelial detachment (PED), shallow subretinal fluid (SRF), and cystic intraretinal fluid can also be seen in this case. The RPE changes are best evaluated using fundus autofluorescence (FAF). In chronic CSC (c), multiple areas showing mixed hyperautofluorescence and hypoautofluorescence can be seen in the posterior pole. A downward gravitational tract of hypoautofluorescent can be seen. PPE is thought to be a forme fruste of CSC. On irregular RPE elevation overlying pachychoroid disease features without subretinal fluid can be seen in d. OCTA confirmed absence of neovascularization (e) and FAF showed milder granular autofluorescence disturbance than in c, without a gravitational tract. Cross-sectional OCT findings in PCN may be similar to those in chronic CSC and PPE, characterized by irregular RPE elevation with or without SRF. OCTA can readily detect the presence of neovascularization (h). Features of PCV/AT1 overlap significantly with PCN, with the additional feature of aneurysms. Although indocyanine green angiography (ICGA) is considered the gold standard for diagnosing PCV/AT1, common features on OCT include irregular RPE elevation overlying pachychoroid disease changes and narrow-peaked PEDs (arrow). In the corresponding OCTA (j), an aneurysm (hollow arrow) can be seen to arise from a branching vascular network. FCE is characterized by a localized area of choroidal excavation on OCT. In the conforming type (k), the photoreceptor tips are not separated from the underlying RPE, whereas in the non-conforming type (l) a hyporeflective space can be observed between the photoreceptor tips and RPE. Unusual hyperreflective choroidal tissue (arrowhead) can be seen to bridge the space between the bottom of the excavation and the outer choroidal boundary. Dilated choroidal vessel and thickened choroid can be seen on either side of the excavation. In PPS, the choroid is thicker on the nasal side to the fovea compared to the temporal side in the cross-sectional OCT (m). More dilated choroidal vessels (white arrows) are seen on the nasal side compared to the temporal side of the fovea on ICGA (n). Fundus autofluorescence illustrates mottled autofluorescence temporal to the disc and extending downwards (o)