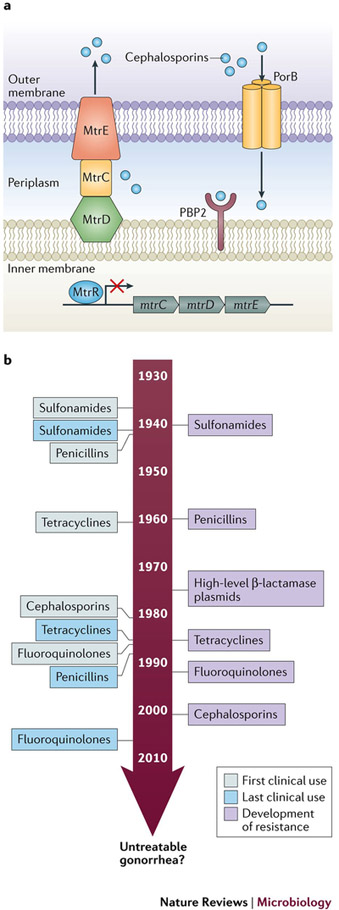
Figure 5: Antibiotic resistance in Neisseria gonorrhoeae a. Main resistance determinants of N. gonorrhoeae.
Transpeptidase penicillin binding protein 2 (PBP2), encoded by penA is a periplasmic transpeptidase and the main lethal target of cephalosporins; most resistant isolates contain mosaic mutations in penA. The efflux pump, MtrCDE, composed of subunits MtrE, MtrC, and MtrD, and its repressor MtrR contribute to N. gonorrhoeae resistance through antimicrobial efflux. The major porin protein, PorB, encoded by penB, is also a main resistance determinant that cannot manifest independently, but requires concomitant mutation in mtrR. b. Timeline of antibiotic resistance development. Since the treatment of N. gonorrhoeae with sulfonamides in the 1930s, N. gonorrhoeae have acquired genetic resistance determinants that prevent killing by all major classes of antibiotics that are used as first line methods of treatment for gonorrhea infection143,145,147,182. As shown in the timeline, each new class of antibiotics that served as first line treatment for N. gonorrhoeae have been stopped as all strains gained resistance. Recently, resistance was observed for the last available first line treatment for N. gonorrhoeae infection, the extended-spectrum cephalosporins143. The ability of N. gonorrhoeae to evolve resistance has lead the World Health Organization and Center for Disease Control, United States to term it a ‘superbug’, and speculate that, if new therapies are not developed soon, we may face an era of untreatable antimicrobial resistant gonorrhea3.