Abstract
Objective
Clear understanding of the long-term consequences of critical care survivorship is essential. We investigated the care process and individual factors associated with long-term mortality among ICU survivors and explored hospital use in this group.
Design
Population based data linkage study using the Secure Anonymised Information Linkage (SAIL) databank.
Setting
All ICUs between 2006-2013 in Wales, UK.
Patients
We identified 40,631 patients discharged alive from Welsh adult ICUs.
Intervention
none.
Measurements and Main results
Primary outcome was 365-day survival. The secondary outcomes were 30 and 90-day survival and hospital utilisation in the 365 days following ICU discharge. Kaplan-Meier curves were plotted to compare survival rates. Cox proportional hazards regression models were used to determine risk factors of mortality. 7,883 (19.4%) patients died during the 1-year follow-up period. In the multivariable Cox regression analysis, advanced age and comorbidities were significant determinants of long-term mortality. Expedited discharge due to ICU bed shortage was associated with higher risk. The rate of hospitalisation in the year prior to the critical care admission was 28 hospitalised days/1000 days, post critical care was 88 hospitalised days/1000 days for those who were still alive; and 57 hospitalised days/1000 days and 412 hospitalised days/1000 days for those who died by the end of the study, respectively.
Conclusions
One in five ICU survivors die within one year, with advanced age and comorbidity being significant predictors of outcome, leading to high resource use. Care process factors indicating high system stress were associated with increased risk. More detailed understanding is needed on the effects of the potentially modifiable factors to optimise service delivery and improve long-term outcomes of the critically ill.
Keywords: long-term outcome, mortality, epidemiology, intensive care unit, healthcare utilisation
Introduction
Demand for critical care services is rising in many countries due to population ageing (1), advances in medical care and changes in patient, public and clinical expectations (2, 3). However, as healthcare becomes more expensive, there is heightened interest in the appropriate use of expensive care modalities, particularly where financial austerity is felt (4). For critical care, a clear understanding of the short- and long-term consequences of intervention is essential if access to critical care resources is to be robust, transparent and equitable (5).
The importance of age, acute physiological derangement and admission diagnosis in predicting intensive care unit (ICU) mortality have been long-established, though historically focus has been predominantly on short-term outcomes (e.g. ICU- or 30-day mortality) (6). More recent studies have suggested that beyond the initial critical illness, the rate and extent of recovery among critical care survivors is more dependent upon chronic morbidity and on sub-acute factors, than on acute illness (7–12). To date no studies have explored the potential impact of care process factors on the long-term mortality of ICU survivors.
The aim of this study is to investigate care process and patient level factors associated with long-term mortality among ICU survivors. We also set out to explore the hospital use 1 year before critical care admission and 1 year following critical care discharge in this group.
Methods
Datasets
We used the Secure Anonymised Information Linkage (SAIL) databank (www.saildatabank.com) to investigate long-term hospital utilisation and mortality in patients surviving to critical care discharge. The development of the SAIL databank as a secure databank of anonymised person-based records has been described previously (13–15). The analysis of anonymised linked data was approved by the Information Governance Review Panel of the SAIL Collaboration Review System (Longitudinal analysis of Critical Care Outcomes in Wales, Project No: 0634, 20/06/2017)
The datasets linked within the SAIL databank we utilised for this study were: the Welsh Critical Care Dataset (WCCD, collated from the monthly exports of the Critical Care Minimum Dataset from all Welsh ICUs - including organ support, admission and discharge data), the Welsh Demographic Service Dataset (WDSD, demographic data submitted by primary care services), the Patient Episode Database for Wales (PEDW), and the Annual District Death extract of the Office for National Statistics (ONS, see Supplementary Digital Content (SDC) for further details on Data Sources).
Study cohort
We identified our study population as patients discharged alive from Welsh adult ICUs between April 2006 and December 2013 from the WCCD. This dataset was linked with the WDSD to obtain patient factors such as week of birth, sex, date of death and anonymised address details. We used the week of birth to generate age on discharge date from critical care and anonymised NHS registration address histories to determine time periods over which patients had lived in Wales.
We included the first index critical care admissions for all patients aged 16 years or more discharged alive from critical care. We excluded patients transferred to another ICU, for whom we could not be sure of previous ICU exposure, and we excluded those discharged to palliative care. Furthermore, we limited the cohort to those with high quality matching from the identity linkage and anonymisation process. Patients were followed up until 365 days after ICU discharge, death or outward migration.
Sample classification
We used ICD-10 codes from the PEDW inpatient dataset to determine the reason for the hospital admission and specifically to determine if the admission was due to trauma using a formula we have developed previously and to generate the Comorbidity Index score (16, 17). The modified Charlson Comorbidity Index described by Bottle and Aylin was generated using ICD-10 codes from all hospital admissions in the year preceding the discharge date (17, 18) (see SDC for further details). Scores were categorised into three groups: low (-1-0), medium (1-10) and high (>10) (17). We used anonymised address histories to determine a patient’s Welsh Index of Multiple Deprivation (WIMD) 2011 quintile (see SDC for further details).
Description of organisational constrains and care processes
On average, there are 3.2 intensive care beds per 100,000 people in Wales. All Welsh Critical Care units have participated in the Intensive Care National Audit and Research Centre Case Mix Programme (ICNARC CMP) since 2008. The Annual Quality reports generated by ICNARC have indicated that all Welsh critical care units are within 2SD of the predicted mortality derived from the wider CMP database, with low reported numbers of critical care acquired infections and longer than average delays in discharging patients from critical care. Case mix, acuity, length of stay and number of organs supported among patients admitted to Critical Care units in Wales are otherwise consistent with that reported for the wider CMP population. We provide detailed links to publicly available reports and datasets which describe the organisational structure, the changes occurred, and the care processes applied in the Welsh critical care service in the SDC.
Outcomes
The primary outcome was 365-day survival. The secondary outcomes were 30 and 90-day survival and total number of days in hospital per 1000 days in the 365 days following ICU discharge.
Hospital days pre- and post-critical care
Days spent in hospital during the year before and the year after the index ICU admission was measured using the PEDW inpatient dataset for each patient and presented as a proportion of total 365 days pre-ICU and a proportion of time to migration, death or 365 days (whichever was the shortest), respectively. We also reported hospital days per 1000 follow-up days both before and after the index episode. Data errors such as null hospital admission and discharge dates were identified and excluded from the analysis.
Statistical analysis
Statistical analysis was performed in R using the ‘Survival’ and ‘Survminer’ packages (19).
Basic demographic data are presented as counts and percentages.
Cox proportional hazards regression models were used to determine risk factors of mortality. Variables were classified as individual patient and care process factors (See Table S1 in the SDC). The Akaike information criterion (AIC) and backward elimination methods were used separately to determine the significant factors associated with mortality. The likelihood ratio test was used in the backward elimination method using a significance level of p<0.05. We only considered main effects in this analysis; interaction terms were not included in the models. Proportional hazards were tested by observing the parallel ln[-ln{S(t)}] curves for each variable and testing the correlation between scaled Schoenfeld residuals and Kaplan Meier survival time. Time dependent coefficients were incorporated in extended Cox models for variables that failed the proportional hazards assumption. Categories were created to denote missing data and we assumed data missing at random.
Results are presented in the form of hazard ratios (HR) with 95% confidence intervals (95% CI) and p-values.
Hospital utilisation is presented as median (IQR) and incident rate ratios were calculated from the ratios of the total days in hospital and the total follow-up time. The Wilcoxon rank-sum test was used to test for differences in the proportion of time spent in hospital between those alive at the end of the study and those who died.
Results
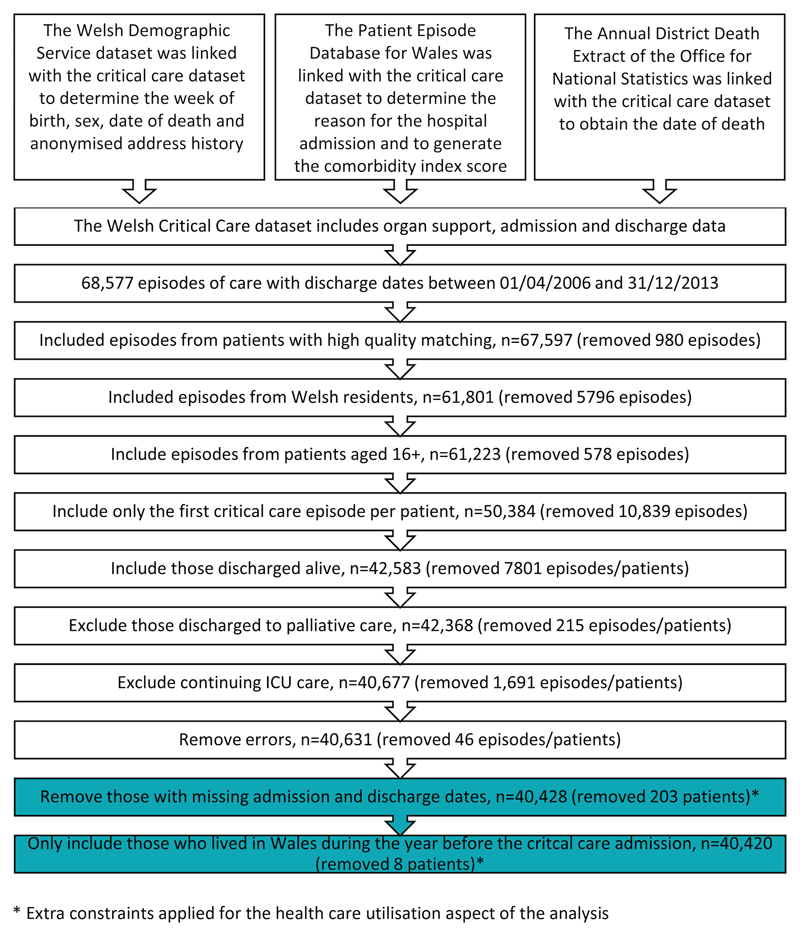
The critical care dataset included 68,577 episodes of care between 1st April 2006 and 31st December 2013. The following flowchart demonstrates how the survival cohort of 40,631 patients and the hospital utilisation cohort of 40,420 patients were obtained (Figure 1.).
Figure 1. Organisational flowchart of the study.
High quality matching: using the Matching Algorithm for Consistent Results in Anonymised Linkage (MACRAL) algorithm to apply deterministic record linkage and probabilistic record linkage methods to the set of linked variables (15); First critical care episode: re-admission episodes during the study period were excluded; Discharged alive: patients who died while on the ICU were excluded; Continuing ICU care: patients who were transferred internally within the same critical care unit were excluded.
Survival Analysis
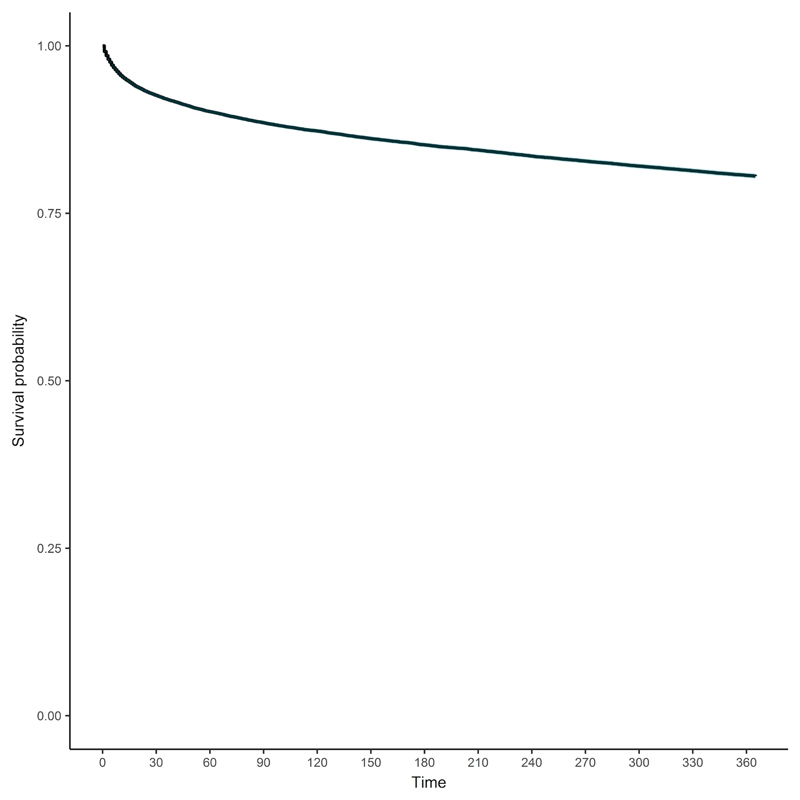
Of the 40,631 patients discharged alive from critical care, 7,883 (19.4%) died during the 1-year follow-up period. Survival probability at 30 days, 90 days and 1 year following ICU discharge was 0.926 (95% CI 0.923-0.928), 0.885 (0.882-0.888) and 0.805 (0.801-0.809) respectively (Figure 2 and Figure S1 in SDC). This was almost identical throughout the study period (Figure S2 in SDC). Baseline characteristics, organ support and discharge data is shown in SDC Table S2 and Table S3. Comparison of patients who died without leaving the hospital following the index critical care admission vs. those who were discharged alive from the hospital but died later is presented in SDC Table S4.
Figure 2. 1-year survival probability of patients discharged from the Welsh intensive care units during the study period.
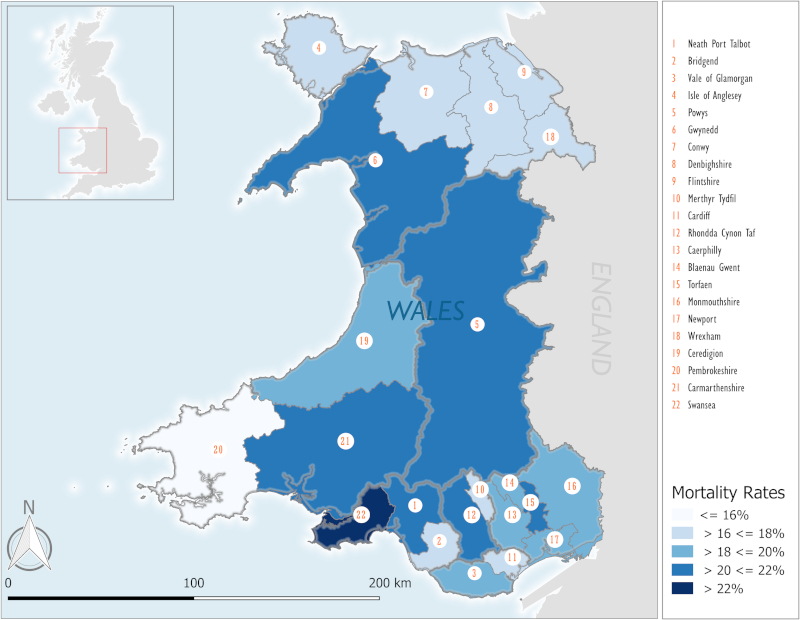
The geographical distribution of the patients who died during the study period is presented in Figure 3.
Figure 3. Geographical distribution of deaths during the study period.
Percentage of death: % of patients who died during the entire study period in a Local Authority area. University Health Board boundaries (consisting of 2 or 3 Local Authorities) are depicted as grey borders. Population details of each Local Authority area is provided in Table S8 in the Supplemental Digital Content.
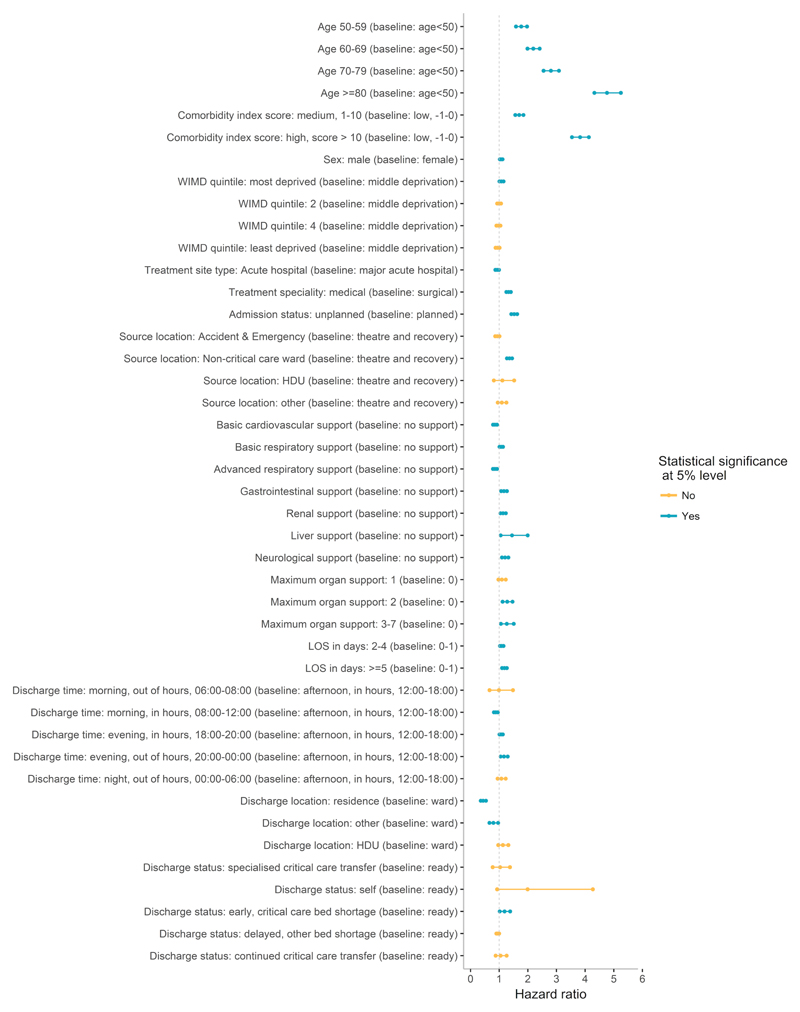
In the multivariable Cox regression analysis, we found multiple patient and care process factors associated with higher risk of mortality after 1 year (Figure 4, also see SDC Table S5). Both the AIC and backward elimination methods identified the same variables. Advanced age and comorbidities were significant determinants of long term mortality (Figure S3 and S4 in SDC). Unplanned acute admissions, admissions for medical reasons, admissions from a hospital ward and the provision of basic respiratory, gastrointestinal, liver, neurological or renal support as defined by the CCMDS were associated with increased hazard (more detailed information on organ support definitions can be found in the SDC). Expedited discharge from the ICU due to critical care bed shortage and evening discharges were associated with higher risks of death. Discharges direct to home appear to reduce the hazard. Details on the variables that failed the proportional hazards assumption are available in the SDC Table S6.
Figure 4. Factors affecting survival from the multivariate Cox-regression model.
WIMD: Welsh Index of Multiple Deprivation; Admission status: unplanned: acute admission from the Emergency Department or the ward; Comorbidity score calculation and organ support definitions are described in the Supplemental Digital Content; Acute hospital: provide a range of acute in-patient and out-patient services, specialist services (including some surgical acute specialties) but not the wide range available in major acute hospitals and may not have 24/7 Emergency Department. LOS: Length of stay; HDU: High dependency unit. Discharge status: specialised critical care transfer: Transferred from critical care unit for tertiary specialist critical care provision; Discharge status: early, critical care bed shortage: Transferred from critical care before deemed clinically ready to lower acuity beds due to ICU capacity reasons; Discharge status: continued critical care transfer: Transferred from critical care unit due to capacity reasons.
Hospital utilisation
40,420 patients were included in the hospital day utilisation aspect of the analysis, of whom 7,821 had died by the end of the study. The rate of hospitalisation in the year prior to the critical care admission was 28 hospitalised days/1000 days for those who were still alive at the end of the observation period and was 57 hospitalised days/1000 days for those who died by the end of the observation period. The rate during the follow-up period post critical care for those alive and those who died was 88 hospitalised days/1000 days and 412 hospitalised days/1000 days, respectively. The incident rate ratio of hospitalisation for those who were alive and those who died by the end of the study period was 3.19 (95% CI: 3.173, 3.198) and 7.28 (95% CI: 7.233, 7.320), respectively (Table S7 and Figure S5 and S6 in SDC). Of the 32,599 survivors, 17,696 were re-hospitalised during the follow-up period.
In the time period after the critical care admission, the proportion of follow-up time spent in hospital in those who died was significantly higher compared to those who were alive within 1-year of ICU discharge (median= 0.97 IQR= 0.69 for non-survivors vs. median= 0.04, IQR=0.08 for survivors, respectively, p< 0.001.)
Discussion
We found that one in five patients who were discharged alive from critical care died within 1 year, with most events within 90 days of ICU discharge. In a multi-variate analysis, advancing age and multiple comorbidities were associated with adverse outcome, together with need for multiple organ support and length of ICU stay. Importantly, we have discovered several organisational factors which were associated with improved survival, notably, discharge during the morning in office hours and discharge directly to home from the ICU. We found that those who died in the 1-year follow-up period had a higher rate of hospitalisation before and after the critical care admission. Almost half of the patients who died after critical care discharge, died before leaving hospital.
Our study is the first large scale population-based analysis of ICU survivors in the Welsh NHS, encompassing almost a decade. We have confirmed, that 1-year survival is primarily determined by patient factors such as age and chronic comorbidities (20). A contemporary population-based study looking at long-term outcomes over a 10-year period found almost identical 1-year mortality, risk factors and healthcare utilisation of ICU survivors in Canada (21). Similar to our findings age, comorbidity, and primary diagnosis were strongest predictors of 1-year survival in large cohorts of Australian and Dutch patients from point of hospital discharge after critical illness (10, 11). Lone et al. recently reported a 1-year mortality of 10.9% in Scotland (8). Whilst this appears to be half of our 19.5% mortality, their cohort only consisted of ICU survivors who were also alive at hospital discharge. We included all patients, who were discharged alive from the ICU and found that the post-ICU hospital mortality was 9.4%. Thus, our cohort also had a 1-year mortality of 10.8%, when we only look at ICU survivors who were alive at hospital discharge.
Half of the patients who died during our study period did so without leaving the hospital following the critical care index episode. These patients were older, had more comorbidities, had longer ICU stay and received more organ support compared to the ones who died following hospital discharge. It is also possible that these patients had higher illness severity on ICU admission, however we could not quantify this from data available for our analysis. Whilst it is plausible that higher severity of illness on ICU admission results in worse long-term outcomes, it appears to be more important in the short-term, within 30-days of ICU discharge when examined in large, population-based datasets (8, 22, 23). Indeed, investigating determinants of short- and long-term survival in a population-based study set between 1999-2008, Garland and colleagues concluded that short-term mortality was largely determined by acute illness factors, whereas mortality beyond three months was mainly determined by age and comorbidity (7). Our results suggest that despite surviving the acute organ dysfunction and ICU stay, patients older than 80 years of age with comorbidities are at high risk of death within 1-year of ICU discharge. The mortality following ICU discharge in this patient group was worse than the pessimistic prediction model developed in Norway, but similar to the data reported elsewhere on contemporary cohorts (5, 22, 23).
Large percentage of patients who died lived in geographical areas where the over 65 years old population is well above the Welsh average (24). However, in two areas (covered by Cwm Taf and Aneurin Bevan University Health Boards) the number of deaths over the study period seemed to be more closely aligned with high level of deprivation and known concentration of chronic illnesses, primarily due to strong industrial heritage, whilst the over 65 years old population is lower (24). Previously Welch et al. reported that significantly more patients are admitted to critical care in England from areas of high social deprivation, with worse hospital outcomes (25). Our data suggest that lack of critical care capacity may play part in the observed mortality as these are the two health boards that have the least amount of critical care beds per 100.000 population in Wales, whilst according to the ICNARC data hospital mortality for patients admitted to the critical care units serving these areas was within 1SD of national average (26).
Admissions for medical conditions, patients needing multiple organ support and long ICU stay were independent predictors of death after 1-year of ICU discharge. All these factors have been reported previously as significant determinants of short-term ICU and hospital mortality (7, 10, 21, 27, 28). In line with the recently published analysis of the whole ICNARC dataset, admissions or discharges at night were not associated with adverse outcomes (29). On the other hand, premature discharge, due to lack of critical care bed availability, which happens usually out-of-hours and at times of high nursing and medical workload, is associated with higher mortality. Similar findings have been reported from multiple groups, giving external validity to our data (30, 31). Discharge to home directly from the ICU was associated with better outcome, presumably as patients in this group were younger with fewer comorbidities and reversible single system pathology, in keeping with the findings of Lau et al. (32).
We are the first to provide population-based data on hospital utilisation both before and after the index episode of ICU survivors. Our findings, that the length of hospitalisation in the year prior to ICU admission can be used as a predictor of post-ICU outcome, strengthen our argument on the importance of comorbidities and potentially frailty being key drivers for long-term mortality. The rate and length of hospitalisation associated with ICU survivorship can be used to inform health policy for health care systems similar to the Welsh NHS. Unsurprisingly, hospitalisation was longest amongst the non-survivors, both before and after ICU. This correlates with the high index of comorbidity in this group. Our results will help to inform discussions with patients, family members and healthcare professionals of the consequences of surviving an admission to ICU.
The strengths of this study are the use of a complete national cohort of patients, inclusion of all patients discharged from the ICU, near complete follow-up and use of an integrated data linkage system (14). These factors minimize the risks of selection and loss to follow up biases frequently encountered in prospective observational studies and provide external validity (33). However, there are certain limitations. The national administrative inpatient data lacks detailed information about disease severity and medical treatments, and co-morbidities based on the ICD-10 coding may not be accurate. We could not analyse the impact of illness severity on ICU admission, as this data is not available currently in the SAIL databank. Although this is an important limitation, the currently available evidence suggests following ICU and hospital discharge acute illness severity has diminishing impact on long-term outcomes (7, 8). We did not assess the impact of frailty, which has been shown to have a significant association with short- and long-term mortality in other regions (34–36). In the current analysis, we were unable to evaluate some important long-term outcomes that are not routinely recorded, such as self-rated health and ability to perform activities of daily living. However, we are working on extending data linkage to primary and social care to evaluate outcomes expected to be related to these factors.
Conclusions
One in five ICU survivors die within one year, with advanced age and comorbidity being significant predictors of outcome. Premature discharge due to unavailability of ICU bed was associated with higher mortality. Hospital use before and after the ICU discharge was high, especially in non-survivors who tended to be older and with significant co-morbidities. While age and co-morbidity are non-modifiable factors, we highlighted potentially adaptable organisational and care process factors to optimise service provision and improve long-term outcomes of the critically ill.
Supplementary Material
Acknowledgements
The authors are grateful for the help of Dr Richard Fry in producing the geographic maps for the study.
Funding:
This work was supported by a grant from the Critical Illness Implementation Group, Welsh Assembly Government
Footnotes
Conflict of interest:
The authors declare that no conflict of interest exists.
Copyright form disclosure: Drs. Szakmany and Pugh’s institution received funding from the Critical Illness Implementation Group, Welsh Assembly Government. Dr. Szakmany’s institution also received funding from a Medical research Council DPFS Grant, a patent pending on biomarker panels for sepsis, Fiona Elizabeth Agnew Trust (FEATURES Award), Welsh Intensive Care Society Research Grant, and the Society of Critical Care Medicine (travel). He received funding from Couton Mutton Diagnostics Ltd, and disclosed that he is one of the Clinical Leads of the All Wales Critical Care and Trauma Network, which oversees the strategic development of critical care services in Wales. Dr. Walters’ institution received funding from the Farr Institute CIPHER, which is supported by a 10- funder consortium: Arthritis Research UK, the British Heart Foundation, Cancer Research UK, the Economic and Social Research Council, the Engineering and Physical Sciences Research Council, the Medical Research Council, the National Institute of Health Research, the National Institute for Social Care and Health Research (Welsh Assembly Government), the Chief Scientist Office (Scottish Government Health Directorates), and the Wellcome Trust, (MRC Grant No: MR/K006525/1). Dr. Pugh’s institution also received funding from Clinical Research Time Award, Health and Social Services Group, Welsh Government. Dr. Lyons’ institution received funding from National Health Service Wales, Medical Research Council, Economic and Social Research Council, Engineering and Physical Sciences Research Council, British Heart Foundation, Wellcome Trust, National Institute of Health Research, Welsh Government, and he received support for article research from Wellcome Trust/COAF and Research Councils UK. The remaining authors have disclosed that they do not have any potential conflicts of interest.
References
- 1.Halpern NA, Goldman DA, Tan KS, et al. Trends in Critical Care Beds and Use Among Population Groups and Medicare and Medicaid Beneficiaries in the United States: 2000-2010. Crit Care Med. 2016;44:1490–1499. doi: 10.1097/CCM.0000000000001722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cox CE, Martinu T, Sathy SJ, et al. Expectations and outcomes of prolonged mechanical ventilation. Crit Care Med. 2009;37:2888–94. doi: 10.1097/CCM.0b013e3181ab86ed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pugh R, Subbe CP, Thorpe C, et al. The Baby Boom and later life: is critical care fit for the future? Anaesthesiol Intensive Ther. 2017;49:441–444. doi: 10.5603/AIT.a2017.0078. [DOI] [PubMed] [Google Scholar]
- 4.Angus DC. Admitting Elderly Patients to the Intensive Care Unit-Is it the Right Decision? JAMA. 2017;318:1443–1444. doi: 10.1001/jama.2017.14535. [DOI] [PubMed] [Google Scholar]
- 5.Docherty AB, Anderson NH, Walsh TS, et al. Equity of Access to Critical Care Among Elderly Patients in Scotland: A National Cohort Study. Crit Care Med. 2016;44:3–13. doi: 10.1097/CCM.0000000000001377. [DOI] [PubMed] [Google Scholar]
- 6.Vincent J-L, Marshall JC, Namendys-Silva SA, et al. Assessment of the worldwide burden of critical illness: the intensive care over nations (ICON) audit. Lancet Respir Med. 2014;2:380–386. doi: 10.1016/S2213-2600(14)70061-X. [DOI] [PubMed] [Google Scholar]
- 7.Garland A, Olafson K, Ramsey CD, et al. Distinct determinants of long-term and short-term survival in critical illness. Intensive Care Med. 2014;40:1097–1105. doi: 10.1007/s00134-014-3348-y. [DOI] [PubMed] [Google Scholar]
- 8.Lone NI, Gillies MA, Haddow C, et al. Five-Year Mortality and Hospital Costs Associated with Surviving Intensive Care. Am J Respir Crit Care Med. 2016;194:198–208. doi: 10.1164/rccm.201511-2234OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ranzani OT, Zampieri FG, Besen BAMP, et al. One-year survival and resource use after critical illness: impact of organ failure and residual organ dysfunction in a cohort study in Brazil. Crit Care. 2015;19:269. doi: 10.1186/s13054-015-0986-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brinkman S, Bakhshi-Raiez F, Abu-Hanna A, et al. Determinants of mortality after hospital discharge in ICU patients: literature review and Dutch cohort study. Crit Care Med. 2013;41:1237–1251. doi: 10.1097/CCM.0b013e31827ca4f9. [DOI] [PubMed] [Google Scholar]
- 11.Williams TA, Dobb GJ, Finn JC, et al. Determinants of long-term survival after intensive care. Crit Care Med. 2008;36:1523–1530. doi: 10.1097/CCM.0b013e318170a405. [DOI] [PubMed] [Google Scholar]
- 12.Kaarlola A, Tallgren M, Pettilä V. Long-term survival, quality of life, and quality-adjusted life-years among critically ill elderly patients. Crit Care Med. 2006;34:2120–2126. doi: 10.1097/01.CCM.0000227656.31911.2E. [DOI] [PubMed] [Google Scholar]
- 13.Jones KH, Ford DV, Jones C, et al. A case study of the Secure Anonymous Information Linkage (SAIL) Gateway: a privacy-protecting remote access system for health-related research and evaluation. J Biomed Inform. 2014;50:196–204. doi: 10.1016/j.jbi.2014.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ford DV, Jones KH, Verplancke J-P, et al. The SAIL Databank: building a national architecture for e-health research and evaluation. BMC Health Serv Res. 2009;9:157. doi: 10.1186/1472-6963-9-157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lyons RA, Jones KH, John G, et al. The SAIL databank: linking multiple health and social care datasets. BMC Med Inform Decis Mak. 2009;9:3. doi: 10.1186/1472-6947-9-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lyons RA, Turner S, Lyons J, et al. All Wales Injury Surveillance System revised: development of a population-based system to evaluate single-level and multilevel interventions. Inj Prev. 2016;22(Suppl 1):i50–5. doi: 10.1136/injuryprev-2015-041814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bottle A, Aylin P. Comorbidity scores for administrative data benefited from adaptation to local coding and diagnostic practices. J Clin Epidemiol. 2011;64:1426–1433. doi: 10.1016/j.jclinepi.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 18.Team CI. Summary Hospital-level Mortality Indicator (SHMI) 1st. NHS Digital; 2017. https://files.digital.nhs.uk/4E/52CC64/SHMI%20specification.pdf. [Google Scholar]
- 19.Crawley MJ. The R Book. Chichester, UK: John Wiley & Sons; 2012. [Google Scholar]
- 20.Orwelius L, Nordlund A, Nordlund P, et al. Pre-existing disease: the most important factor for health related quality of life long-term after critical illness: a prospective, longitudinal, multicentre trial. Crit Care. 2010;14:R67. doi: 10.1186/cc8967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hill AD, Fowler RA, Pinto R, et al. Long-term outcomes and healthcare utilization following critical illness--a population-based study. Crit Care. 2016;20:76. doi: 10.1186/s13054-016-1248-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chin-Yee N, D'Egidio G, Thavorn K, et al. Cost analysis of the very elderly admitted to intensive care units. Crit Care. 2017;21:109. doi: 10.1186/s13054-017-1689-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lindemark F, Haaland ØA, Kvåle R, et al. Age, risk, and life expectancy in Norwegian intensive care: a registry-based population modelling study. PLoS ONE. 2015;10:e0125907. doi: 10.1371/journal.pone.0125907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Statistics OON. Broad Age Population Estimates in Wales. [accessed on 05/03/2018]; https://www.healthmapswales.wales.nhs.uk/IAS/dataviews/report/multiple?reportId=60&viewId=178&geoTypeId=107,108,109,110,111.
- 25.Welch CA, Harrison DA, Hutchings A, et al. The association between deprivation and hospital mortality for admissions to critical care units in England. J Crit Care. 2010;25:382–390. doi: 10.1016/j.jcrc.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 26.Rhodes A, Ferdinande P, Flaatten H, et al. The variability of critical care bed numbers in Europe. Intensive Care Med. 2012;38:1647–1653. doi: 10.1007/s00134-012-2627-8. [DOI] [PubMed] [Google Scholar]
- 27.Garland A, Olafson K, Ramsey CD, et al. A population-based observational study of intensive care unit-related outcomes. With emphasis on post-hospital outcomes. Ann Am Thorac Soc. 2015;12:202–208. doi: 10.1513/AnnalsATS.201405-201CME. [DOI] [PubMed] [Google Scholar]
- 28.Brinkman S, de Jonge E, Abu-Hanna A, et al. Mortality after hospital discharge in ICU patients. Crit Care Med. 2013;41:1229–1236. doi: 10.1097/CCM.0b013e31827ca4e1. [DOI] [PubMed] [Google Scholar]
- 29.Arulkumaran N, Harrison DA, Brett SJ. Association between day and time of admission to critical care and acute hospital outcome for unplanned admissions to adult general critical care units: cohort study exploring the 'weekend effect'. British Journal of Anaesthesia. 2017;118:112–122. doi: 10.1093/bja/aew398. [DOI] [PubMed] [Google Scholar]
- 30.Yang S, Wang Z, Liu Z, et al. Association between time of discharge from ICU and hospital mortality: a systematic review and meta-analysis. Crit Care. 2016;20:390. doi: 10.1186/s13054-016-1569-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Neuraz A, Guérin C, Payet C, et al. Patient Mortality Is Associated With Staff Resources and Workload in the ICU: A Multicenter Observational Study. Crit Care Med. 2015;43:1587–1594. doi: 10.1097/CCM.0000000000001015. [DOI] [PubMed] [Google Scholar]
- 32.Lau VI, Priestap FA, Lam JNH, et al. Factors Associated With the Increasing Rates of Discharges Directly Home From Intensive Care Units-A Direct From ICU Sent Home Study. Journal of Intensive Care Medicine. 2018;33:121–127. doi: 10.1177/0885066616668483. [DOI] [PubMed] [Google Scholar]
- 33.Williams TA, Leslie GD. Challenges and possible solutions for long-term follow-up of patients surviving critical illness. Aust Crit Care. 2011;24:175–185. doi: 10.1016/j.aucc.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 34.Flaatten H, de Lange DW, Morandi A, et al. The impact of frailty on ICU and 30-day mortality and the level of care in very elderly patients (≥ 80 years) Intensive Care Med. 2017;43:1820–1828. doi: 10.1007/s00134-017-4940-8. [DOI] [PubMed] [Google Scholar]
- 35.Heyland DK, Garland A, Bagshaw SM, et al. Recovery after critical illness in patients aged 80 years or older: a multi-center prospective observational cohort study. Intensive Care Med. 2015;41:1911–1920. doi: 10.1007/s00134-015-4028-2. [DOI] [PubMed] [Google Scholar]
- 36.Brummel NE, Bell SP, Girard TD, et al. Frailty and Subsequent Disability and Mortality among Patients with Critical Illness. Am J Respir Crit Care Med. 2017;196:64–72. doi: 10.1164/rccm.201605-0939OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.