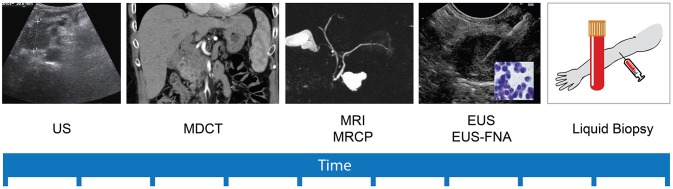
Figure 1.
Timeline of development of pancreatic cancer diagnostic and staging modalities. Pancreatic cancer (PC) diagnosis and staging depends, substantially, on imaging modalities. Abdominal Ultrasonography (US) was the first to appear, but lacks sensitivity to detect small treatable lesions. Multidetector computed tomography (MDCT) is nowadays frequently used to detect and stage pancreatic masses, with good accuracy specially for 2 cm and larger lesions. Magnetic resonance imaging (MRI) and its variant magnetic resonance cholangiopancreatography (MRCP) improved the sensitivity for characterization small cystic lesions. More recently, endoscopic ultrasonography (EUS) with the possibility to perform fine needle aspiration (FNA) constitutes a prime modality for precise diagnosis and local staging of small (< 2 cm) solid and cystic pancreatic lesions. The innovative concept of liquid biopsy refers to a simple and painless collection of a body fluid sample (usually blood), in order to study proved and anticipated biomarkers with the potential to detect PC in its early non detectable stages and even the premalignant precursors.