Abstract
Hypothesis and background
Accurate measurement of range of motion (ROM) is important in evaluating a pathologic shoulder and calculating shoulder scores. The aim of this study was to establish the reliability and validity of different smartphone applications (apps) in assessing pathologic shoulder ROM and to determine whether differences in recorded ROM measurements affect calculated shoulder scores. The authors hypothesized that there is no difference between shoulder ROM assessment methods and calculated shoulder scores.
Methods
In this nonrandomized controlled clinical trial, ROM of 75 participants with a history of shoulder disease (21 women, 54 men) was assessed using a smartphone inclinometer and virtual goniometer, a standard goniometer, and clinicians' visual estimation. Shoulder strength was assessed, and Constant-Murley (CM) and University of California–Los Angeles (UCLA) shoulder scores were calculated.
Results
Independent of diagnosis or operation, all cases (except for passive glenohumeral abduction of unstable shoulders) showed excellent intraclass correlation coefficients (>0.84). Interobserver reliability was excellent for all ROM measures (intraclass correlation coefficient > 0.97). All modalities had excellent agreement to values attained with the universal goniometer. There were no differences for the calculated CM or UCLA scores between the modalities employed to measure ROM.
Conclusions
A smartphone inclinometer or virtual goniometer is comparable to other clinical methods of measuring pathologic shoulder ROM. Clinicians can employ smartphone applications with confidence to measure shoulder ROM and to calculate UCLA and CM scores. The apps are also available to patients and may be a useful adjunct to physiotherapy, especially in cases of limited access to health care services.
Keywords: Shoulder range of motion, Inclinometer, Goniometer, Smartphone application, Constant-Murley score, UCLA score
Accurate and reliable measurement of shoulder range of motion (ROM) is integral to the physical examination and functional evaluation of a pathologic shoulder. A universal goniometer (UG) is considered the “gold standard” for measuring shoulder ROM1; however, visual estimation is common in clinical practice as it is more time efficient, and a goniometer is often not available.2, 26, 28 Other methods for measuring shoulder ROM include digital inclinometry, digital motion capture, and high-speed cinematography, but these require expensive, specialized equipment with limited availability.9, 10, 13, 16, 24, 28
Smartphone applications (apps) have recently been proposed as an alternative method of measuring pathologic shoulder ROM.15, 21, 22, 26, 29 Apps rely on an internal smartphone inclinometer26 or a photographic virtual goniometer21 to measure ROM. Several studies have demonstrated joint ROM measured with apps to be reliable and accurate compared with traditional methods,7, 14, 15, 19, 21, 23, 25, 26, 29 but studies performed on the shoulder were limited by inclusion of only participants with no joint disease (for whom they have the most potential clinical application). In addition, no shoulder study considered the impact that ROM variability may have on shoulder scores with an objective ROM component.
The Constant-Murley (CM) score5 and the University of California–Los Angeles11 (UCLA) shoulder score are commonly used shoulder assessment tools that evaluate level of function and efficacy of surgical interventions and observe clinical change over time. These shoulder patient-reported outcome measures have the advantage over other scoring systems of including subjective patient-derived inputs as well as objective clinician-derived inputs, allowing a more balanced interpretation of shoulder function.5
Shoulder scores enhance communication during the physician-patient consultation6, 8 and aid in clinical decision-making. As shoulder ROM is an important component of these scores, measurements must be accurate and reliable for the scores to be of clinical use.
Apps have been shown to be accurate and reliable in measuring ROM in normal shoulders; however, their use in the pathologic shoulder is yet to be assessed. The authors hypothesized that smartphone ROM apps will provide accurate and reliable measurements when tested on pathologic shoulders.
Materials and methods
Patients were recruited from the outpatient department of 2 tertiary orthopedic units between February 2015 and February 2016. Inclusion criteria were being English speaking, older than 18 years, and willing to provide informed consent and having a documented current shoulder disease. Patients were excluded if they had cognitive impairment or were unable to follow the assessor's instructions. In cases of bilateral shoulder disease, both shoulders were assessed independently and included.
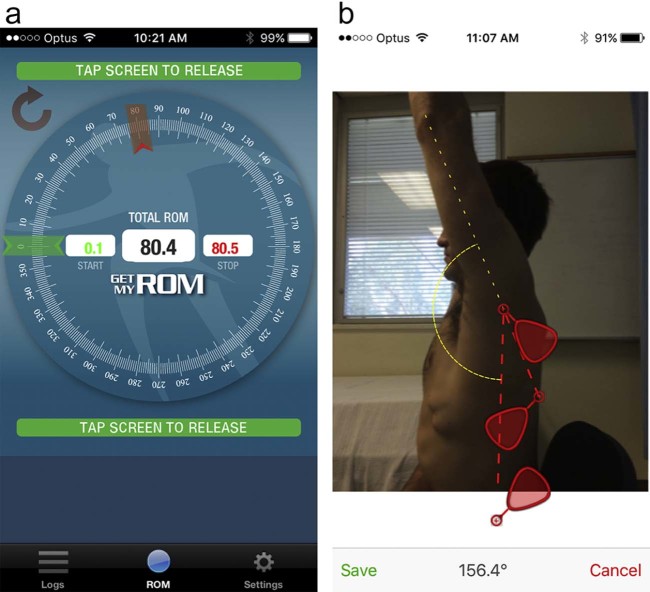
One iPhone (Model 5S) was used in the study and the software not updated during data collection. Two iPhone apps were used to measure shoulder range of movement (ROM): GetMyROM (version 1.0.3; Interactive Medical Productions, Hampton, NH, USA), an inclinometry-based app (Fig. 1, A); and DrGoniometer (version 1.2; CDM S.r.L, Milano, Italy), a photo capture–based application (Fig. 1, B). Visual ROM estimates were recorded for each subject, as were measurements made using a standard, manual goniometer as a control. A questionnaire recorded the subjective and functional questions of the UCLA and CM shoulder scores.
Figure 1.
The iPhone applications. (A) GetMyROM. (B) DrGoniometer.
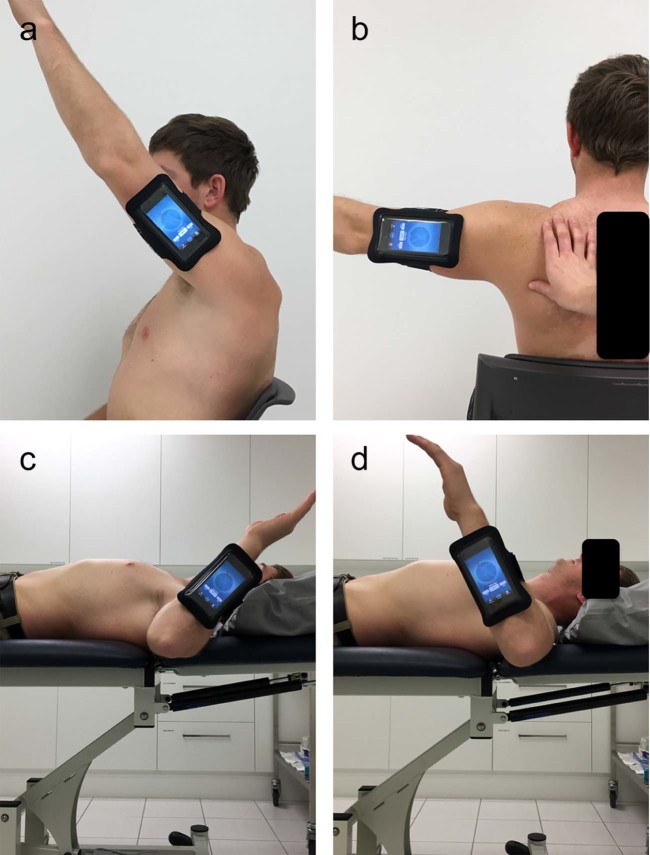
All participants were assessed with exposed shoulders. Two medical practitioner observers with experience in musculoskeletal disease collected the data independently with an assistant. Participants initially sat upright and straight on a fixed chair to stabilize the spine. In this position, the following measurements were observed: active forward flexion (Fig. 2, A), total abduction, active glenohumeral abduction (Fig. 2, B), and passive glenohumeral abduction. To assess glenohumeral joint abduction, the participants were asked to abduct the arm while the examiner stabilized the scapular. Commencement of scapula rotation was used to determine the limit of glenohumeral joint movement.
Figure 2.
Measurements of (A) forward flexion, (B) glenohumeral abduction, (C) external rotation, and (D) internal rotation.
Rotation of the shoulder was measured with participants supine on a standard examination table. The shoulder was positioned in 90° of abduction with 90° of flexion at the elbow. With the forearm in neutral rotation and the proximal two-thirds of the humerus supported by the table, measurements were taken for active (Fig. 2, C) and passive external rotation and active (Fig. 2, D) and passive internal rotation. If shoulder disease prevented the participant from abducting the shoulder to 90°, supine external rotation was measured with the elbow in contact with the side of the body (0° abduction), and internal rotation measures were not recorded. With all ROM tests, care was taken to avoid compensatory movements, such as elbow extension or scapular elevation, and if these were observed, the measurement was repeated.
Shoulder ROM was first assessed using the smartphone inclinometer attached to the participant with a DualFit Armband (Belkin; Playa Vista, CA, USA). The armband was attached to the distal portion of the humerus for seated movements, then repositioned to the wrist for measurements performed with the participant supine. The inclinometer was positioned with the screen facing away from the observer. The assistant read and recorded the ROM value with the observer blinded to the reading. Next, the observer captured photographs of the participant with the shoulder positioned at the limits of ROM, to be analyzed at a later date using DrGoniometer. Third, the observer gave a visual estimate of shoulder ROM and last measured the ROM using the standard goniometer.
A myometer (Isometer; Innovative Design Orthopaedics Ltd., London, UK) was employed to measure shoulder strength using the method described by Constant et al.5 Participants stood with their feet shoulder-width apart and the arm held at 90° of abduction in the scapular plane. The forearm was placed in full pronation and shoulder internal rotation. A looped arm strap was placed 2 cm proximal to the wrist. With the elbow straight at all times, participants were instructed to lift up with maximal strength. The measurement was repeated 2 more times and the highest value used to calculate the CM score.5, 29 Participants who were not able to establish the desired degrees of abduction or experienced pain when completing this part of the assessment were assigned a strength score of 0 and were not subjected to further strength measurement. Strength measurements were used in conjunction with the questionnaires to calculate the UCLA and CM shoulder scores.
To assess the reliability of the 4 methods, all measurements were completed by 2 independent observers. An intraclass correlation coefficient (ICC) was calculated using SAS 9.3 (SAS Institute, Cary, NC, USA). An ICC was calculated for each ROM test, interpreted as follows: 0.00-0.40, poor correlation; 0.41-0.59, fair correlation; 0.60-0.74, good correlation; and 0.75-1.00, excellent correlation.4
A Bland-Altman analysis was used to assess the level of agreement between the ROM measurement modalities. A 95% limit of agreement was defined as ±1.96 standard deviations around the mean difference from measurements obtained by the UG, thus producing a lower and upper level of agreement.
A negative binomial generalized estimating equation was used to account for clustering on random effects of the subjects and raters. Assumptions of linear regression were not upheld. Modeling was performed for the CM scores and ROM as well as for UCLA scores and ROM.
Results
From February 2015 to February 2016, 75 patients were recruited from the outpatient department of 2 tertiary orthopedic units (21 women, 54 men). The average age was 46 years (range, 24-94 years). Fourteen patients had bilateral shoulder disease.
The underlying shoulder diseases in descending order of frequency included shoulder instability (n = 23), degenerative changes/arthritis (n = 9), inflammation (n = 9), prior fracture (n = 4), and soft tissue disease (n = 30). Diagnoses and surgical interventions are presented in Table I.
Table I.
Diagnoses and operations of participants (N = 75)
| Diagnosis | Operation |
|---|---|
| Inflammation (n = 9) SA bursitis ± impingement Scapulothoracic bursitis/snapping scapula Fractures (n = 4) Proximal humerus Clavicle Degenerative/arthritic (n = 9) ACJ osteoarthritis SCJ osteoarthritis GHJ osteoarthritis Septic arthritis Instability (n = 23) Traumatic (including dislocations) ACJ dislocation/subluxation Soft tissue (n = 30) Proximal biceps tendon tear (long head) Rotator cuff tear SLAP biceps tear Supraspinatus tendinopathy |
No operation (n = 58) Arthroscopic surgery (n = 6) Rotator cuff repair Labral stabilization Other therapeutic procedure Open nonarthroplasty procedures (n = 10) Latarjet/Bristow ACJ lateral clavicle excision Rotator cuff repair Open washout of shoulder joint Total shoulder arthroplasty (n = 1) Reverse |
SA, subacromial; ACJ, acromioclavicular joint; SCJ, sternoclavicular joint; GHJ, glenohumeral joint; SLAP, superior labral tear from anterior to posterior.
In all cases for the group diagnoses (except for passive glenohumeral abduction of the instability group), ICC values were classified as having excellent agreement (>0.84). In regard to surgical intervention, the ICC value for each ROM test was >0.95.
The ICC values are presented in Table II. All values were >0.97, indicating excellent agreement between the 4 methods of measurement for each ROM. Each ROM variable showed a left-skewed distribution.
Table II.
Interobserver reliability for each range of motion (ROM) measurement method
| ROM test | Method | ICC | Lower 95% limit | Upper 95% limit |
|---|---|---|---|---|
| Forward flexion | Clinician | 1.00 | 0.99 | 1.00 |
| Goniometer | 0.99 | 0.99 | 1.00 | |
| GetMyROM | 0.99 | 0.98 | 0.99 | |
| DrGoniometer | 1.00 | 0.99 | 1.00 | |
| Total active abduction | Clinician | 1.00 | 0.99 | 1.00 |
| Goniometer | 0.99 | 0.99 | 1.00 | |
| GetMyROM | 0.99 | 0.99 | 1.00 | |
| DrGoniometer | 0.99 | 0.99 | 1.00 | |
| Active glenohumeral abduction | Clinician | 0.99 | 0.99 | 1.00 |
| Goniometer | 0.98 | 0.97 | 0.99 | |
| GetMyROM | 0.98 | 0.97 | 0.99 | |
| DrGoniometer | 0.98 | 0.97 | 0.99 | |
| Passive glenohumeral abduction | Clinician | 0.99 | 0.99 | 1.00 |
| Goniometer | 0.98 | 0.99 | 0.99 | |
| GetMyROM | 0.97 | 0.95 | 0.99 | |
| DrGoniometer | 0.98 | 0.96 | 0.99 | |
| Active internal rotation | Clinician | 0.99 | 0.99 | 0.99 |
| Goniometer | 0.99 | 0.99 | 0.99 | |
| GetMyROM | 0.98 | 0.97 | 0.99 | |
| DrGoniometer | 0.99 | 0.99 | 1.00 | |
| Passive internal rotation | Clinician | 0.99 | 0.98 | 0.99 |
| Goniometer | 0.99 | 0.99 | 0.99 | |
| GetMyROM | 0.98 | 0.96 | 0.98 | |
| DrGoniometer | 1.00 | 0.99 | 1.00 | |
| Active external rotation | Clinician | 0.99 | 0.98 | 0.99 |
| Goniometer | 0.99 | 0.98 | 0.99 | |
| GetMyROM | 0.99 | 0.98 | 0.99 | |
| DrGoniometer | 1.00 | 0.99 | 1.00 | |
| Passive external rotation | Clinician | 0.99 | 0.99 | 1.00 |
| Goniometer | 1.00 | 0.99 | 1.00 | |
| GetMyROM | 0.99 | 0.98 | 0.99 | |
| DrGoniometer | 0.99 | 0.99 | 1.00 |
ICC, intraclass correlation coefficient.
The results of Bland-Altman plots, comparing the other 3 methods of measurement with the measurements obtained by the UG, are presented in Table III. These values are within a narrow range and indicate generally superior agreement, although active and passive glenohumeral abduction had the narrowest limit range (ie, more agreement between the methods of measurement and UG), and forward flexion resulted in a larger range of values.
Table III.
Bland-Altman plots comparing measurement modalities to the “gold standard” goniometer
| Comparison measurement mean to universal goniometer | Comparative measurement technique | Mean difference | Lower 95% limit | Upper 95% limit |
|---|---|---|---|---|
| Forward flexion | Clinician | 1.69 | −5.17 | 8.55 |
| GetMyROM | −0.76 | −9.64 | 8.11 | |
| DrGoniometer | −0.56 | −9.63 | 8.52 | |
| Total active abduction | Clinician | 0.37 | −6.46 | 7.20 |
| GetMyROM | 0.47 | −7.87 | 8.81 | |
| DrGoniometer | 0.81 | −7.73 | 9.35 | |
| Active glenohumeral abduction | Clinician | −0.18 | −2.90 | 2.54 |
| GetMyROM | −0.19 | −4.71 | 4.32 | |
| DrGoniometer | −0.41 | −6.93 | 6.12 | |
| Passive glenohumeral abduction | Clinician | −0.07 | −2.04 | 1.90 |
| GetMyROM | −0.38 | −4.02 | 3.25 | |
| DrGoniometer | −0.01 | −2.32 | 2.30 | |
| Active internal rotation | Clinician | −0.29 | −5.51 | 4.93 |
| GetMyROM | 0.51 | −7.11 | 8.14 | |
| DrGoniometer | −1.29 | −10.00 | 7.43 | |
| Passive internal rotation | Clinician | 0.00 | −4.66 | 4.66 |
| GetMyROM | 0.55 | −5.04 | 6.13 | |
| DrGoniometer | −1.41 | −9.83 | 7.01 | |
| Active external rotation | Clinician | 0.01 | −5.02 | 5.05 |
| GetMyROM | −0.08 | −8.32 | 8.17 | |
| DrGoniometer | 0.20 | −8.23 | 8.63 | |
| Passive external rotation | Clinician | 0.42 | −5.18 | 6.02 |
| GetMyROM | 0.40 | −7.58 | 8.37 | |
| DrGoniometer | 0.13 | −7.65 | 7.91 |
Nineteen participants (25.3%) were not able to complete strength assessments as a result of pain (n = 15) or loss of ROM (n = 4). These participants were assigned a strength score of 0 in calculating UCLA and CM scores. When the CM and UCLA scores were calculated for each method of assessing ROM, all methods revealed identical mean CM scores (74; range, 6-100) and mean UCLA scores (29; range, 7-35).
Discussion
This study demonstrated that the ROM measurements in pathologic shoulders are consistent in comparing a UG with visual estimates and 2 different smartphone ROM apps. It also demonstrated that there is no difference in the calculated shoulder UCLA and CM scores using the 4 different methods, suggesting that newer technologies that use smartphone applications may be a useful tool in the clinical setting.
Previous studies3, 12, 17, 30 have assessed the accuracy and validity of smartphone apps in measuring joint ROM; however, those focused on the shoulder were limited by assessing only normal shoulders in healthy, young individuals.15, 18, 21 In contrast, this study assessed patients of varying ages with a spectrum of shoulder diseases, thus providing a relevant clinical context and a broader spectrum of assessable shoulder ranges over which to compare the assessment modalities. Previous studies were also limited to the assessment of active shoulder motion only.15, 18, 21 In addition to examining both active and passive ROM, this study also assessed a more complete set of shoulder movements, including internal and external rotation, abduction, and forward flexion. This study also assessed the clinically relevant movement of glenohumeral joint abduction, an important sign that can assist in differentiating subacromial and subdeltoid adhesions from adhesive capsulitis in pathologic and postoperative patients. To the authors' knowledge, this movement has not previously been investigated using different ROM assessment modalities.
This study is the first to compare 4 different shoulder ROM assessment tools in a pathologic patient cohort. The 4 assessment modalities used (the clinician's visual estimation, inclinometer-based smartphone application [GetMyROM], photograph-based [DrGoniometer] smartphone application, and UG) demonstrated excellent agreement. This finding was similar to that of Werner et al, who assessed postsurgical shoulder ROM in patients having undergone total shoulder replacement surgery and reported excellent correlation when using an inclinometer Smartphone application in isolation.29 This study is also one of the few studies that assessed an older population cohort (mean age, 46 years), in various planes of shoulder movement, with various shoulder diseases and diagnoses. The only other study to examine inclinometer- and photograph-based shoulder assessment tools relied exclusively on measurements of external rotation performed on young, healthy subjects (mean age, 26.4 ± 7.6 years).21
Certain advantages exist in adopting these new technologies. Inclinometry-based applications allow fast, reliable measurements of shoulder ROM and are widely available and cost-effective, given the prevalence of smartphone ownership in the general population. They are available not only to physicians but also to allied health professionals and patients. As well as being used in a clinical setting, the inclinometry-based apps allow patient self-measurement,12 providing real-time feedback for exercise completed at home. This may be of particular benefit to those with limited access to health care because of rural location or disability, for whom some assessment may be performed by a combination of telephone, tele-link, or secured e-mail.
Photograph-based applications, whereby clinicians make measurements in a delayed fashion (post-production and independent of the patient's location), allow images to be printed and filed in patient notes for comparison during subsequent visits. Like inclinometry-based apps, photograph-based applications allow accurate ROM assessment when a goniometer is not available or when a face-to-face interaction with a health professional is not immediately available. Moreover, the physician-patient interaction can potentially be enhanced by demonstrating the patient's progress in ROM over time.12, 20
Whereas visual assessment of ROM may require experience to give an accurate estimation, a recent study29 reported that the skill level of medical assessor does not influence the ROM assessment with use of smartphone applications (ie, student vs. medical clinician). This is important, as clinicians and allied health practitioners who do not have exclusively musculoskeletal practices may employ these smartphone applications with the confidence that they will produce consistent results. Non–musculoskeletal-focused clinicians are less likely to have experience with visual estimation of shoulder ROM, and consequently the measurements obtained may be affected.
The UCLA and CM scores are important adjuncts to the management of patients with shoulder disease and can be used to assess for change in function over time. Both have subjective and objective components that allow a more balanced interpretation of a patient's true shoulder function. This is the first study to compare smartphone applications for measuring shoulder ROM in a pathologic patient cohort and subsequently using these measurements to calculate and to compare UCLA and CM shoulder scores. In this study, both the UCLA and CM shoulder scores were similar in comparing various modalities of ROM measurement. These findings suggest that these smartphone applications can be used with confidence to calculate UCLA and CM shoulder scores in patients with a spectrum of shoulder diseases.
Limitations exist in using inclinometer- and photograph-based smartphone applications for shoulder ROM measurement. Inclinometer applications require the mobile device to be in contact with the patient. This is best achieved with an instrument that physically holds the phone to the patient (such as an armband).26 Hygiene issues may be raised when an armband is used repeatedly and suggest the need for disposable armbands.1, 27 The position of the measurement device is important to achieve consistent results. It was our experience that the armband sometimes required adjustment (eg, rotated around the longitudinal axis of the humerus) to attain the appropriate measure. Vigilance of the assessor was required to adjust the armband if it slipped or loosened after initial application.
Photograph-based smartphone applications had similar considerations, especially when the examiner was taking the picture and in positioning the virtual goniometer on anatomic landmarks to measure the angles under investigation.12 Errors could be made if the picture was taken short of maximal ROM or if the photograph was mistimed (and not picked up). Care needed to be taken in measuring the angles under investigation in the photographs, especially in placing markers on the desired anatomic landmarks.
There are limitations to this study. The 2 observers were highly trained and had many years of experience in shoulder examination. This may have influenced the visual estimation results, which may not be reproducible for clinicians with less experience. Care should be taken in interpreting this result, as visual estimation requires a certain level of expertise and practice, which may take several years to achieve. This modality has the most inherent variability and is not recommended for routine use (especially for clinicians who have not self-evaluated their assessments). Ongoing self-evaluation is required to confirm that this technique is valid for each clinician.
Another limitation was the sample size, which was not randomized and was composed of more men than women. The average age of the sample was skewed to the elderly (likely representative of the larger proportion of disease found in the older age groups). A broader and larger sample would allow a more in-depth analysis by gender and age subsets. Future studies could incorporate examination of dynamic movements in addition to static assessments.
Conclusion
Technologic advances offer the opportunity to adopt new tools that can improve patient assessments and follow-up and ultimately lead to improved clinical outcomes. Smartphone app use is a widely available, cost-effective method to assist clinicians in accurately measuring joint range of movement, including that of the shoulder, knee, spine, elbow, and ankle.3, 12, 17, 30 This study demonstrates that shoulder ROM can be reproducibly measured using 4 independent methods. Smartphones can be used with confidence by clinicians to provide a reliable, reproducible, practical, and inexpensive way of assessing shoulder ROM.
Disclaimer
The investigators independently paid for a license to use the research software and database. The individual research tool registrations were paid for by OBERD Pty Ltd and are included as part of the licensing agreement.
The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Acknowledgments
The authors thank Suzanne Edwards, Statistician, Data Management and Analysis Centre at the University of Adelaide, for her help with the statistical analysis of the collected data.
Footnotes
The Human Research Ethics Committee, The Queen Elizabeth Hospital, Basil Heizel Institute DX465101, approved this study: HREC/14/TQEHLMH/239.
References
- 1.Albrecht U.V., von Jan U., Sedlacek L., Groos S., Suerbaum S., Vonberg R.P. Standardized, App-based disinfection of iPads in a clinical and nonclinical setting: comparative analysis. J Med Internet Res. 2013;15:e176. doi: 10.2196/jmir.2643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Awan R., Smith J., Boon A.J. Measuring shoulder internal rotation range of motion: a comparison of 3 techniques. Arch Phys Med Rehabil. 2002;83:1229–1234. doi: 10.1053/apmr.2002.34815. [DOI] [PubMed] [Google Scholar]
- 3.Blonna D., Zarkadas P.C., Fitzsimmons J.S., O'Driscoll S.W. Validation of a photography-based goniometry method for measuring joint range of motion. J Shoulder Elbow Surg. 2012;21:29–35. doi: 10.1016/j.jse.2011.06.018. [DOI] [PubMed] [Google Scholar]
- 4.Cicchetti D.V. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess. 1994;6:284–290. [Google Scholar]
- 5.Constant C.R., Gerber C., Emery R.J., Sojbjerg J.O., Gohlke F., Boileau P. A review of the Constant score: modifications and guidelines for its use. J Shoulder Elbow Surg. 2008;17:355–361. doi: 10.1016/j.jse.2007.06.022. [DOI] [PubMed] [Google Scholar]
- 6.Coons S.J., Gwaltney C.J., Hays R.D., Lundy J.J., Sloan J.A., Revicki D.A. Recommendations on evidence needed to support measurement equivalence between electronic and paper-based patient-reported outcome (PRO) measures: ISPOR ePRO Good Research Practices Task Force report. Value Health. 2009;12:419–429. doi: 10.1111/j.1524-4733.2008.00470.x. [DOI] [PubMed] [Google Scholar]
- 7.Cuesta-Vargas A.I., Roldan-Jimenez C. Validity and reliability of arm abduction angle measured on smartphone: a cross-sectional study. BMC Musculoskelet Disord. 2016;17:93. doi: 10.1186/s12891-016-0957-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dawson J., Fitzpatrick R., Carr A. Questionnaire on the perceptions of patients about shoulder surgery. J Bone Joint Surg Br. 1996;78:593–600. [PubMed] [Google Scholar]
- 9.De Winter A.F., Heemskerk M.A., Terwee C.B., Jans M.P., Deville W., Schaardenburg D.J. Inter-observer reproducibility of measurements of range of motion in patients with shoulder pain using a digital inclinometer. BMC Musculoskelet Disord. 2004;5:18. doi: 10.1186/1471-2474-5-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.El-Zayat B.F., Efe T., Heidrich A., Wolf U., Timmesfeld N., Heyse T.J. Objective assessment of shoulder mobility with a new 3D gyroscope—a validation study. BMC Musculoskelet Disord. 2011;12:168. doi: 10.1186/1471-2474-12-168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ellman H., Hanker G., Bayer M. Repair of the rotator cuff. End-result study of factors influencing reconstruction. J Bone Joint Surg Am. 1986;68:1136–1144. [PubMed] [Google Scholar]
- 12.Ferriero G., Vercelli S., Sartorio F., Munoz Lasa S., Ilieva E., Brigatti E. Reliability of a smartphone-based goniometer for knee joint goniometry. Int J Rehabil Res. 2013;36:146–151. doi: 10.1097/MRR.0b013e32835b8269. [DOI] [PubMed] [Google Scholar]
- 13.Hayes K., Walton J.R., Szomor Z.R., Murrell G.A. Reliability of five methods for assessing shoulder range of motion. Aust J Physiother. 2001;47:289–294. doi: 10.1016/s0004-9514(14)60274-9. [DOI] [PubMed] [Google Scholar]
- 14.Jenny J.Y. Measurement of the knee flexion angle with a Smartphone-application is precise and accurate. J Arthroplasty. 2013;28:784–787. doi: 10.1016/j.arth.2012.11.013. [DOI] [PubMed] [Google Scholar]
- 15.Johnson L.B., Sumner S., Duong T., Yan P., Bajcsy R., Abresch R.T. Validity and reliability of smartphone magnetometer-based goniometer evaluation of shoulder abduction—a pilot study. Man Ther. 2015;20:777–782. doi: 10.1016/j.math.2015.03.004. [DOI] [PubMed] [Google Scholar]
- 16.Jordan K., Dziedzic K., Jones P.W., Ong B.N., Dawes P.T. The reliability of the three-dimensional FASTRAK measurement system in measuring cervical spine and shoulder range of motion in healthy subjects. Rheumatology (Oxford) 2000;39:382–388. doi: 10.1093/rheumatology/39.4.382. [DOI] [PubMed] [Google Scholar]
- 17.Kolber M.J., Pizzini M., Robinson A., Yanez D., Hanney W.J. The reliability and concurrent validity of measurements used to quantify lumbar spine mobility: an analysis of an iphone application and gravity based inclinometry. Int J Sports Phys Ther. 2013;8:129–137. [PMC free article] [PubMed] [Google Scholar]
- 18.Lim J.Y., Kim T.H., Lee J.S. Reliability of measuring the passive range of shoulder horizontal adduction using a smartphone in the supine versus the side-lying position. J Phys Ther Sci. 2015;27:3119–3122. doi: 10.1589/jpts.27.3119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Milanese S., Gordon S., Buettner P., Flavell C., Ruston S., Coe D. Reliability and concurrent validity of knee angle measurement: smart phone app versus universal goniometer used by experienced and novice clinicians. Man Ther. 2014;19:569–574. doi: 10.1016/j.math.2014.05.009. [DOI] [PubMed] [Google Scholar]
- 20.Milani P., Coccetta C.A., Rabini A., Sciarra T., Massazza G., Ferriero G. Mobile smartphone applications for body position measurement in rehabilitation: a review of goniometric tools. PM R. 2014;6:1038–1043. doi: 10.1016/j.pmrj.2014.05.003. [DOI] [PubMed] [Google Scholar]
- 21.Mitchell K., Gutierrez S.B., Sutton S., Morton S., Morgenthaler A. Reliability and validity of goniometric iPhone applications for the assessment of active shoulder external rotation. Physiother Theory Pract. 2014;30:521–525. doi: 10.3109/09593985.2014.900593. [DOI] [PubMed] [Google Scholar]
- 22.Mourcou Q., Fleury A., Diot B., Franco C., Vuillerme N. Mobile phone-based joint angle measurement for functional assessment and rehabilitation of proprioception. Biomed Res Int. 2015;2015:328142. doi: 10.1155/2015/328142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pichonnaz C., Duc C., Gleeson N., Ancey C., Jaccard H., Lécureux E. Measurement properties of the smartphone-based B-B Score in current shoulder pathologies. Sensors (Basel) 2015;15:26801–26817. doi: 10.3390/s151026801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pohl M., Mehrholz J. A new shoulder range of motion screening measurement: its reliability and application in the assessment of the prevalence of shoulder contractures in patients with impaired consciousness caused by severe brain damage. Arch Phys Med Rehabil. 2005;86:98–104. doi: 10.1016/j.apmr.2004.01.038. [DOI] [PubMed] [Google Scholar]
- 25.Russell T.G., Jull G.A., Wootton R. Can the Internet be used as a medium to evaluate knee angle? Man Ther. 2003;8:242–246. doi: 10.1016/S1356-689X(03)00016-X. [DOI] [PubMed] [Google Scholar]
- 26.Shin S.H., Ro du H., Lee O.S., Oh J.H., Kim S.H. Within-day reliability of shoulder range of motion measurement with a smartphone. Man Ther. 2012;17:298–304. doi: 10.1016/j.math.2012.02.010. [DOI] [PubMed] [Google Scholar]
- 27.Tekerekoǧlu M.S., Duman Y., Serindağ A., Cuǧlan S.S., Kaysadu H., Tunc E. Do mobile phones of patients, companions and visitors carry multidrug-resistant hospital pathogens? Am J Infect Control. 2011;39:379–381. doi: 10.1016/j.ajic.2010.10.026. [DOI] [PubMed] [Google Scholar]
- 28.Terwee C.B., de Winter A.F., Scholten R.J., Jans M.P., Deville W., van Schaardenburg D. Interobserver reproducibility of the visual estimation of range of motion of the shoulder. Arch Phys Med Rehabil. 2005;86:1356–1361. doi: 10.1016/j.apmr.2004.12.031. [DOI] [PubMed] [Google Scholar]
- 29.Werner B.C., Holzgrefe R.E., Griffin J.W., Lyons M.L., Cosgrove C.T., Hart J.M. Validation of an innovative method of shoulder range-of-motion measurement using a smartphone clinometer application. J Shoulder Elbow Surg. 2014;23:e275–e282. doi: 10.1016/j.jse.2014.02.030. [DOI] [PubMed] [Google Scholar]
- 30.Williams C.M., Caserta A.J., Haines T.P. The TiltMeter app is a novel and accurate measurement tool for the weight bearing lunge test. J Sci Med Sport. 2013;16:392–395. doi: 10.1016/j.jsams.2013.02.001. [DOI] [PubMed] [Google Scholar]