Abstract
Purpose
Pathologic corneal neovascularization is a major cause of blindness worldwide, and treatment options are currently limited. VEGF is one of the critical mediators of corneal neovascularization but current anti-VEGF therapies have produced limited results in the cornea. Thus, additional therapeutic agents are needed to enhance the antiangiogenic arsenal. Our group previously demonstrated epithelial membrane protein-2 (EMP2) involvement in pathologic angiogenesis in multiple cancer models including breast cancer and glioblastoma. In this paper, we investigate the efficacy of anti-EMP2 immunotherapy in the prevention of corneal neovascularization.
Methods
An in vivo murine cornea alkali burn model was used to study pathologic neovascularization. A unilateral corneal burn was induced using NaOH, and subconjunctival injection of either anti-EMP2 antibody, control antibody, or sterile saline was performed after corneal burn. Neovascularization was clinically scored at 7 days postalkali burn, and eyes were enucleated for histologic analysis and immunostaining including VEGF, CD31, and CD34 expression.
Results
Anti-EMP2 antibody, compared to control antibody or vehicle, significantly reduced neovascularization as measured by clinical score and central cornea thickness, as well as by histologic reduction of neovascularization, decreased CD34 staining, and decreased CD31 staining. Incubation of corneal limbal cells in vitro with anti-EMP2 blocking antibody significantly decreased EMP2 expression, VEGF expression and secretion, and cell migration.
Conclusions
This work demonstrates the effectiveness of EMP2 as a novel target in pathologic corneal neovascularization in an animal model and supports additional investigation into EMP2 antibody blockade as a potential new therapeutic option.
Keywords: cornea, corneal neovascularization, epithelial membrane protein-2, vascular endothelial growth factor, angiogenesis
The cornea is a transparent tissue that plays a critical role in light refraction and vision. As it is in physical contact with the external environment, the cornea also acts as a mechanical barrier to provide protection against microorganisms, toxicants, and injury. Under normal conditions, the cornea is clear and has several antiangiogenic factors including soluble VEGF-R1 which helps maintain its unique avascular status.1 However, pathologic neovascularization can occur secondary to trauma, chemical burns, immunologic disease, or infection,2 leading to an upregulation of proangiogenic factors including VEGF-A that promotes hemangiogenesis and inflammation.3 Corneal neovascularization typically presents as ingrowth of blood vessels from the limbus toward the clear center of the cornea. The resulting abnormal blood vessel growth, corneal opacity, and corneal edema reduces the transparency of the cornea, which is critical for good visual acuity.4 As such, neovascularization remains a major cause of blindness worldwide. As many as 1.4 million Americans are seen by physicians each year for vision impairment secondary to abnormal blood vessel growth,5,6 and these causes of corneal blindness present a pressing challenge to address.
Treatment options for corneal neovascularization are limited. Steroids and anti-inflammatory drugs are currently used, but efficacy can be variable and these drugs can produce significant side effects when chronically administered.2 Biologic agents, including intravitreal injections of anti-VEGF antibodies, are increasingly being used to treat a wide variety of ocular diseases involving abnormal retinal neovascularization, including age-related macular degeneration, diabetic retinopathy, and retinopathy of prematurity. Given the clinical efficacy of anti-VEGF in the treatment of these retinal diseases, some studies support efficacy in reducing corneal neovascularization in both animal models and clinical trials.7–9 These anti-VEGF agents have shown initial therapeutic success with at least partial reduction of corneal neovascularization through topical, subconjunctival, and intraocular application.10–14 Although these results are encouraging, anti-VEGF biologics have been associated with significant systemic toxicity and severe ocular complications,15 and additional therapeutics to complement these drugs would be advantageous.
Our lab has extensively studied the role of EMP2, a membrane bound tetraspan protein, in multiple models of vascular development. Prior studies demonstrated a role for EMP2 in pathologic angiogenesis in breast cancer,16 endometrial cancer,17–20 glioblastoma,21–23 and placental angiogenesis.24 EMP2 mRNA is expressed at high levels in the eye, lung, and uterus.25 In the eye, EMP2 is localized to the epithelial layers of the cornea, ciliary body, RPE-choroid, and stromal layers of the sclera.26 Within the retina, EMP2 is found on the membrane of the RPE, and appears to contribute to the pathogenesis observed in proliferative vitreoretinopathy.27–30 EMP2 controls VEGF expression in the RPE cell line ARPE-19.31 Given the protein's role in development of vasculature in multiple disease contexts, and its expression in several discrete subanatomic locations in the eye including corneal epithelium, we sought to investigate its involvement in pathologic neovascularization of the cornea. In this paper, we characterize the expression of EMP2 in the human cornea and localize it to the corneal epithelium. Moreover, we show that EMP2 contributes to corneal neovascularization in a murine corneal burn model in vivo and VEGF expression in vitro in a corneal limbal derived cell line.
Materials and Methods
Animals
We obtained 6- to 8-week-old female Balb/c mice from Jackson Laboratories (Bar Harbor, ME, USA), and housed at the University of California, Los Angeles, in the Division of Laboratory Animal Medicine facility. All animal experiments were reviewed and approved by the University of California, Los Angeles, Chancellor's Animal Research Committee, in adherence to the Association for Research in Vision and Ophthalmology Statement for the Use of Animals in Ophthalmic and Vision Research.
Corneal Neovascularization Induction and Treatment
Corneal neovascularization was induced in 6- to 8-week-old female Balb/c mice using an alkali burn method.32 Animals were anesthetized with 100 μL of ketamine (50 mg/kg) and xylazine (5 mg/kg) solution delivered via intraperitoneal route. The right eye (OD) of each animal was exposed to a 2-mm diameter filter paper soaked with sterile 1 M NaOH for 45 seconds, filter paper was removed using sterile forceps, and the eye was immediately rinsed twice with 10 mL of sterile saline. The left eye (OS) of each animal remained unburned as an untreated internal control. Following the alkali burn, the animals were treated once with either saline, 175 μg of control antibody (human IgG antibody, Sigma-Aldrich Corp., St. Louis, MO, USA), or 175 μg of human anti-EMP2 antibody (purified humanized monoclonal IgG1) via one subconjunctival injection in the temporal region of the conjunctiva. A total of eight mice were used per treatment group. We administered 100 μL of buprenorphine (0.1 mg/kg) via subcutaneous route in the shoulder area prior to alkali burn to aid with pain management. Erythromycin ointment was applied daily for 3 days and monitored daily. The experiment was terminated using euthanasia at day 7 postburn and both eyes were enucleated for additional evaluation.
Clinical Vascular Evaluation
Assessment of corneal neovascularization was performed in a masked fashion using a surgical microscope (Leica S6D; Leica Microsystems; Buffalo Grove, IL, USA). Neovascularization scoring was based on a scale of 0 to 3, as previously described32 at 7 days post-alkali burn, and prior to enucleation.
Areas of neovascularization in the corneas exposed to alkali burn were traced using the Simple Neurite Tracer plugin via NIH ImageJ software33 (http://imagej.nih.gov/ij/; provided in the public domain by the National Institutes of Health, Bethesda, MD, USA). Images were automatically converted to 32-bit grayscale images by the Simple Neurite Tracer plugin.
Cell Culture
Human corneal limbal epithelial (HCLE; HCLE cells were provided by Ilene Gipson, PhD, at Schepens Eye Research Institute, Harvard Medical School) cells were cultured using 1X keratinocyte serum-free medium, per manufacturer's formulation (Thermo Fisher Scientific, Waltham, MA, USA) at 37°C, in a humidified 5% CO2 incubator. HCLE cells were grown to 80% confluency and exposed to 60 μg/mL of anti-EMP2 antibody for 6, 12, 24, or 48 hours. Human umbilical vein endothelial cells (HUVEC; ATCC, Manassas, VA, USA) were cultured in VEC MCDB-131 complete media (VEC Technologies, Rensselaer, NY, USA) at 37°C in a humidified 5% CO2 incubator. HUVECs for in vitro assays were used at passage number 3.
Western Blot Analysis
Cell lysates were prepared and lysed in Laemmli buffer. Proteins were separated on 4% to 20% SDS-PAGE gel (Thermo Fisher Scientific) under reducing conditions, transferred to nitrocellulose membranes (GE Healthcare, Chicago, IL, USA), and blocked with 10% nonfat dry milk in Tris-buffered saline with 0.1% Tween 20. Membranes were probed with the following primary antibodies: anti-VEGF (1 μg/mL; Santa Cruz Biotechnology, Dallas, TX, USA); anti-EMP2 (1:2000; polyclonal antibody; created in our lab and previously published26); anti-β-actin (0.5 μg/mL; US Biological, Salem, MA, USA). Protein bands were detected using horseradish peroxidase (HRP)-labeled secondary antibodies (Southern Biotechnology, Birmingham, AL, USA), followed by chemiluminescence (ECL; EMD Millipore, Burlington, MA, USA). Densitometric analysis of the protein bands were performed using NIH ImageJ software. Loading variability between samples were normalized to β-actin loading controls. At least three independent experiments were performed, and statistical significance was evaluated using Student's t-test.
ELISA
Conditioned media were collected from HCLE cells incubated with media only, or with 60 μg/mL of anti-EMP2 antibody for 6, 12, 24, or 48 hours. Secreted VEGF from conditioned media was detected and analyzed per manufacturer's instructions (Human VEGF Quantikine ELISA kit; R&D Systems, Minneapolis, MN, USA). Each condition was assayed in duplicate and VEGF standards were provided by the manufacturer for quantitation. Optical density was determined using a microplate reader (SpectraMax; Molecular Devices, Sunnyvale, CA, USA) at 540 and 450 nm. Wavelength correction was performed to correct for optical imperfections in the plate. At least three independent experiments were performed, and statistical significance was evaluated using Student's t-test.
Cell Migration Assay
HUVECs were seeded into the upper compartment of transwell inserts of Boyden chambers (24-well plate; Corning, Corning, NY, USA). Conditioned media from HCLE cells were prepared as described above. Bevacizumab (Avastin; Genentech BioOncology, San Francisco, CA, USA) at 60 μg/mL was added to untreated HCLE media as a negative control for the migration assay. We added 500 μL of HCLE conditioned media into the lower compartment of the Boyden chamber. After 5 hours of incubation at 37°C in a humidified 5% CO2 incubator with the conditioned media, the transwell inserts were fixed with 4% paraformaldehyde and stained with 0.2% crystal violet. The inserts were carefully washed with distilled water and left to dry overnight at room temperature. The inserts were imaged and the migrated cells were quantified to determine number of migrated HUVEC cells. At least three independent experiments were performed, and statistical significance was evaluated using Student's t-test.
Immunostaining and Immunofluorescent Microscopy
We fixed 5 μm OCT frozen sections from unfixed human corneal limbus samples (gift from Sophie Deng, MD, PhD, Stein Eye Institute, University of California, Los Angeles, CA, USA) were fixed with 4% paraformaldehyde for 10 minutes, blocked with 1% normal goat serum for 1 hour, and incubated overnight at 4°C with anti-EMP2 (1:1500; polyclonal antibody). Visualization of the immunostaining was performed using an anti-rabbit kit (IgG ABC Vector kit; Vector Laboratories, Burlingame, CA, USA), according to manufacturer's instructions. Alcian blue/methyl green counterstain was used, and slides were mounted for brightfield microscopy (BX51; Olympus, Waltham, MA, USA).
HCLE cells were cultured on glass cover slips for 24 to 48 hours at 37°C, in a humidified 5% CO2 incubator. Cells were fixed with 4% paraformaldehyde for 10 minutes, and stained with primary antibody, anti-EMP2 (1:500; polyclonal antibody) overnight at 4°C. Goat anti-rabbit IgG AlexaFluor 594 (2 μg/mL; Thermo Fisher Scientific) was used for secondary detection. Coverslips were counterstained with DAPI and mounted. Images were obtained at ×400 magnification by immunofluorescence microscopy (Olympus).
Unburned and alkali-burned eyes were enucleated, formalin-fixed, and sectioned at 4 μm. Some sections were stained using hematoxylin and eosin (H&E). Additional sections were deparaffinized and incubated at 95°C for 25 minutes in 0.1 M citrate, pH 6.0, for antigen retrieval and use in immunohistochemical studies. The following primary antibodies were used: anti-CD34 (5 μg/mL; Abcam, Cambridge, MA, USA), anti-CD31 (10 μg/mL; Dianova, Hamburg, Germany), anti-LYVE-1 (0.2 μg/mL; R&D Systems) and anti-VEGF (4 μg/mL, clone A-20; Santa Cruz Biotechnology). Detection of the immunostaining was executed using anti-rat IgG and anti-rabbit kit (Vector Laboratories), according to manufacturer's instructions. Sections were counterstained and mounted. Detection of bound anti-CD31 or the anti-LYVE-1 antibodies was performed using anti-rat IgG AlexaFluor 594 and anti-goat IgG AlexaFluor 594 (Thermo Fisher Scientific) and immunofluorescent evaluation. Sections were counterstained with DAPI, and mounted with Prolong (Thermo Fisher Scientific). Images were obtained at ×400 magnification by brightfield microscopy (Olympus). NIH ImageJ software was used to quantitate CD31 and LYVE-1 fluorescent staining. Images were converted to 8-bit grayscale images and positively stained areas were quantitated.
Results
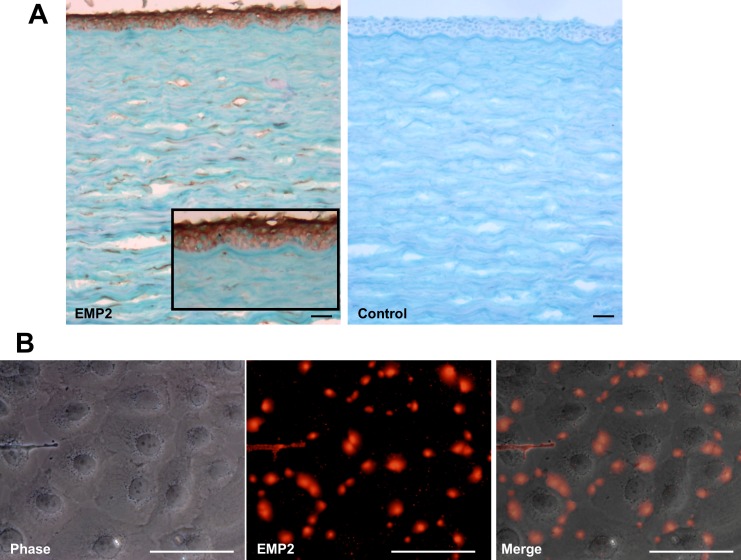
EMP2 is Expressed in Human Corneal Epithelium and HCLE Cells
Sections of human cornea were stained for EMP2 expression to confirm EMP2 localization in human cornea. EMP2 was strongly expressed in corneal epithelium (Fig. 1A). EMP2 expression was also independently confirmed in human corneal-limbal epithelial (HCLE) cells, a frequently used immortalized human corneal epithelial cell line (Fig. 1B). The HCLE cells demonstrated strong punctate staining of EMP2, which interestingly appeared to be localized to sites of direct cell-cell contact, as observed in other cell types.28,36,37
Figure 1.
EMP2 is expressed in human corneal epithelium and HCLE cells. (A) Sections of human cornea were stained via immunohistochemistry for EMP2 expression using a polyclonal anti-human EMP2 antibody. EMP2 was noted to be expressed in the corneal epithelium. Scale bar: 200 μm. (B) HCLE cells demonstrated strong punctate staining of EMP2. Notably, EMP2 was only expressed in cells with direct cell-cell contact. Phase contrast, EMP2 staining (red), and merged images shown. Scale bar: 50 μm.
We next sought to explore whether EMP2 expression plays a pathologic role in a murine model of aberrant corneal neovascularization. To study corneal neovascularization, we utilized an in vivo murine corneal burn model as described in the methods section.32
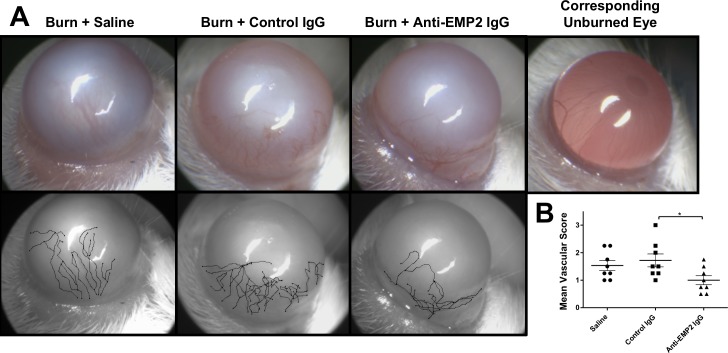
Blockade of EMP2 Results in Clinically Decreased Corneal Neovascularization in an In Vivo Mouse Burn Model
Alkali burn resulted in significant opacification and neovascularization of the cornea in all burned eyes compared to internal unburned control (data not shown). No cases of corneal perforations or infections were observed at any point in these studies. All eyes were used in subsequent analyses. Surgical microscopy images at 7 days postcorneal burn showed significantly less neovascularization in the anti-EMP2 treated eyes compared to saline control and control antibody treated eyes (Fig. 2). Vasculature was manually traced to highlight the degree of neovascularization (Fig. 2A, lower panel). A clinical scoring protocol was used to quantitate neovascularization based on a previously published clinical assessment protocol.32 Corneal neovascularization was clinically scored by masked observers using day 7 corneal images comparing burned eye with internal control eye, with 0 = no neovascularization; 1 = minor neovascularization at the corneal limbus; 2 = moderate neovascularization at the corneal limbus with few vessels approaching corneal center; 3 = extensive neovascularization at the corneal limbus and moderate to many vessels spanning the corneal center.32 The mean clinical neovascularization score from 8 animals per group revealed significantly less corneal neovascularization in the anti-EMP2 antibody treated group compared to controls (Fig. 2B).
Figure 2.
Blockade of EMP2 results in clinically decreased corneal neovascularization in an in vivo mouse burn model. (A) Surgical microscopy images at 7 days postalkali burn and antibody treatment reveal corneal opacity and corneal neovascularization across all three groups of animals. Less corneal neovascularization is observed in anti-EMP2 antibody–treated eyes, when compared to saline and control antibody treated animals. Vasculature was manually traced using ImageJ to emphasize degree of neovascularization. (B) The mean clinical neovascularization score from eight animals per group shows that control antibody treated animals have more corneal neovascularization than the anti-EMP2 antibody–treated group (*P < 0.05).
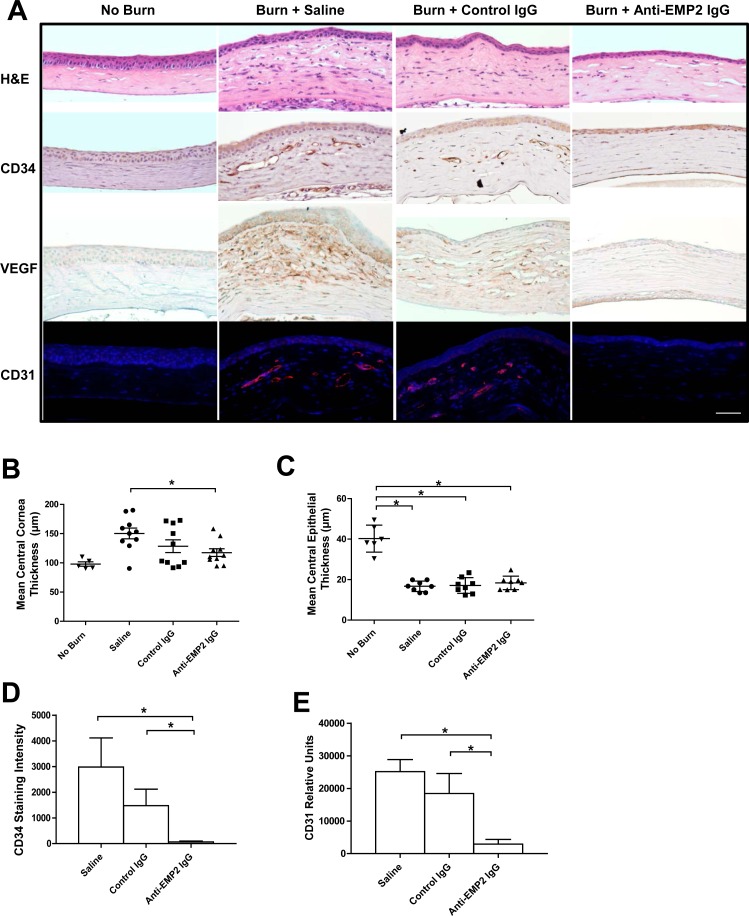
Anti-EMP2–Treated Animals Have Reduced Central Cornea Thickness and Decreased CD34, VEGF, and CD31 Staining in Cornea
The foregoing results suggested that antibody-targeting of EMP2, when given at the time of injury, decreased development of pathologic corneal neovascularization. To further characterize this finding, alkali burned eyes from the anti-EMP2 antibody, control antibody, and saline groups were further compared histologically and immunohistochemically for the markers CD34, VEGF, and CD31 (Fig. 3A). Notably, anti-EMP2–treated corneas have significantly reduced corneal thickness as compared to saline treated eyes (Fig. 3B). This may be clinically important because corneal edema independently contributes to loss of visual acuity even in the absence of neovascularization, as in the case of a variety of diseases involving corneal endothelial dysfunction.34 Burned eyes demonstrate reduced thickness of the corneal epithelial layer, however when all of the eyes were evaluated the average epithelial thickness is unchanged regardless of treatment (Fig. 3C). Expression of CD34, a marker for hematopoietic progenitor cells35 and a probe for neovascularization in multiple tumor models,17,36 was identified using immunohistochemistry. Corneas from animals that received anti-EMP2 antibody showed significantly decreased CD34 staining compared to controls (Fig. 3A, second row), quantified by immunohistologic staining intensity (Fig. 3D). CD34 staining was more strongly observed in the corneal epithelium and the areas adjacent to the corneal endothelium with minimal expression in the corneal stroma. Little to no CD34 expression is observed in control unburned corneas. Expression of an endothelial cell specific marker, CD31, was also used as an independent validation to detect neovascularization, via immunofluorescent staining (Fig. 3A, bottom row). Quantitation of positively stained CD31 areas of immunofluorescent staining, showed that anti-EMP2 antibody significantly decreased CD31 staining compared to vehicle and IgG controls (Fig. 3E). Corneal staining with CD34 and CD31 were concordant, in that anti-EMP2 antibody treated animals showed reduced neovascularization compared to control groups. Anti-EMP2–treated eyes also showed a similar reduction in VEGF expression compared to saline and control antibody treated eyes (Fig. 3A, third row), with minimal to no expression of VEGF in anti-EMP2 antibody treated eyes. Additional staining using a marker for lymphatics (LYVE-1) was used and did not show significant staining in the central cornea under any of the tested conditions (Supplementary Fig. 1A, top panel). LYVE-1 staining was observed in the peripheral cornea of all 3 tested conditions (Supplementary Fig. 1A, bottom panel); however, upon quantitation of the stained areas, no significant differences across the three groups were observed (Supplementary Fig. 1B). We proceeded to further characterize the relationship between EMP2 and VEGF in vitro.
Figure 3.
Anti-EMP2–treated animals have reduced central cornea thickness and decreased CD34, VEGF, and CD31 staining in cornea. ([A], top row) H&E-stained sections were obtained, and the average of three measurements in the central region of each burned cornea were taken. ([A], second row) Immunohistochemical staining of CD34 expression in the treated and untreated corneas show an increase in CD34-positive staining in the saline and control antibody–treated animals, with markedly reduced CD34 staining in anti-EMP2 treated animals. Little to no CD34 expression is observed in the control unburned cornea. (A, third row) Immunohistochemical staining of VEGF expression shows a similar increase in VEGF expression of saline and control antibody treated animals, with markedly reduced VEGF staining in anti-EMP2 treated animals. (A, bottom row) Staining via immunofluorescence with anti-CD31, an endothelial cell specific marker, shows increased expression, as predicted, in the control burns (burn + saline and burn + control IgG), as compared to the unburned cornea. However, concordant with the CD34 histochemical staining, the animals who received the burn and anti-EMP2 IgG exhibited reduced new vessel formation as compared with the control burns. (B) The overall thickness of the central cornea in the anti-EMP2 antibody treated group is significantly reduced compared to the saline treated group (*P < 0.05). (C) The average of three measurements per eye of epithelial thickness from central cornea were taken. Although all burned eyes have significantly reduced epithelial thickness compared to unburned control, the overall thickness of the epithelial layer of the cornea is unchanged and unaffected regardless of type of treatment (saline, control IgG, or anti-EMP2 IgG). (D) Quantitation of CD34 and (E) CD31 positively stained corneal sections demonstrate similar trends with immunohistochemical and immunofluorescent staining (*P < 0.05). Scale bar: 50 μm.
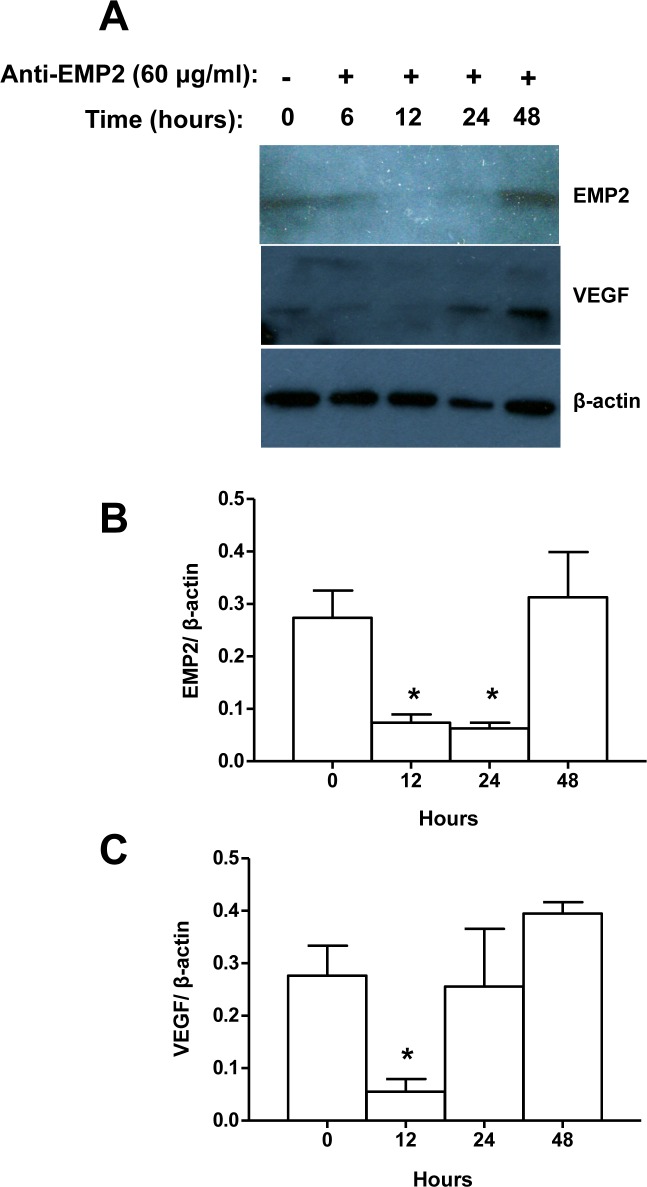
Incubation With Anti-EMP2 Antibody Results in Decreased EMP2 Expression and Decreased VEGF Expression In Vitro in HCLE Cells
Our lab had previously demonstrated that EMP2 controls VEGF expression in the retinal cell line ARPE-19.31 To investigate the relationship between EMP2 expression and VEGF expression in cells derived from the corneal epithelium, we used the human HCLE cell line exposed to anti-EMP2 antibody and quantified expression of EMP2 and VEGF by western blot (Fig. 4A). Anti-EMP2 treatment appears to decrease both EMP2 and VEGF expression in a time-dependent fashion. Expression of EMP2 protein reached a nadir after 12 to 24 hours of anti-EMP2 blockade (Fig. 4B), while expression of VEGF reached a nadir at 12 hours of anti-EMP2 blockade (Fig. 4C). This demonstrated that the expression of EMP2 and VEGF is correlated, and both can be downregulated in a time-dependent fashion by EMP2 antibody blockade.
Figure 4.
Incubation with anti-EMP2 antibody results in decreased EMP2 expression and decreased VEGF expression in vitro in HCLE cells. (A) HCLE cells were incubated with the anti-EMP2 antibody for up to 48 hours, and expression of EMP2 and VEGF quantified by Western blot. (B) Reduction of EMP2 expression decreased to a nadir at 12 to 24 hours, and (C) reduction in VEGF expression reached a nadir at 12 hours.
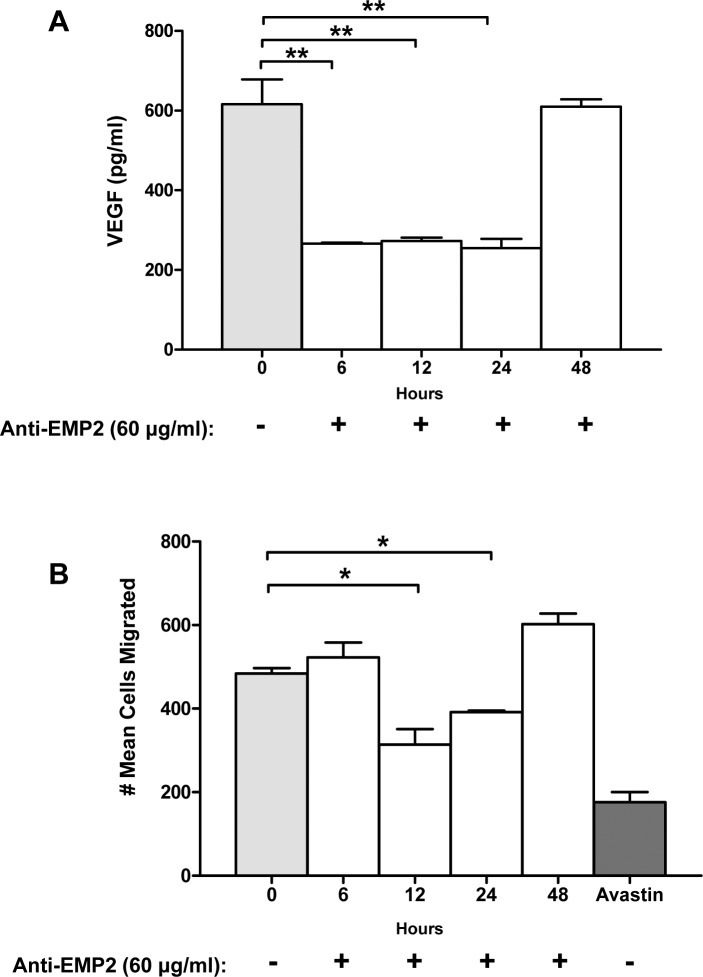
Supernatants From HCLE Cells Previously Incubated With Anti-EMP2 Antibody Show Reduction in Secreted VEGF and Reduced Cell Migration in a Transwell Migration Assay
Supernatants from HCLE cells treated with EMP2 antibody were further tested for presence of secreted VEGF and its functional capacity in a transwell migration assay. Secreted VEGF-A was directly measured by ELISA and demonstrated a time-dependent reduction in VEGF secretion with EMP2 blockade (Fig. 5A). The supernatants were also used to test function in an HUVEC transwell migration assay. Notably, there is a statistically significant reduction in number of cells migrated at 12 and 24 hours using supernatants from HCLE cells exposed to EMP2 blockade (Fig. 5B). This reduced cell migration is likely secondary to reduction in secreted growth factors including VEGF following exposure to the anti-EMP2 antibody.
Figure 5.
Supernatants from HCLE cells previously incubated with anti-EMP2 antibody show reduction in secreted VEGF and reduced cell migration in a transwell migration assay. (A) Secreted VEGF-A was measured by ELISA in the cell culture supernatants of HCLE cells incubated with anti-EMP2 antibody for 0 to 48 hours. There is a time-dependent reduction in VEGF secretion with EMP2 blockade. (B) Supernatants of HCLE cells incubated with anti-EMP2 for 0 to 48 hours were used to test function in an HUVEC transwell migration assay. Of note, there is a statistically significant reduction in the number of cells that have migrated after 12 and 24 hours (*P < 0.05).
Discussion
In this paper, an interaction between EMP2 and VEGF in the murine alkali burn model of corneal neovascularization is demonstrated, which is concordant to other studies that link EMP2 to control of VEGF in tumor models and in the retinal epithelial cell line ARPE-19.17,22,29,31 EMP2 blockade using anti-EMP2 antibodies reduce pathologic neovascularization and corneal edema following corneal burn. This suggests EMP2 as a potentially new target for prevention of corneal neovascularization.
In corneal epithelium and model HCLE cells, we observed that EMP2 was localized to sites of direct cell-cell contact. EMP2 is a member of the GAS-3 protein family, whose cell biology includes interaction with integrins37 and caveolin-1,38 mediation of protein trafficking including MHC class I to lipid raft microdomains,39 a role in apical membrane recycling, and in cell-cell and cell-extracellular matrix interactions.26 These biologic precedents are consistent with localization of EMP2 in sites of cell-cell contact in corneal epithelium, and suggest an analogous functional cell biology in this cell type.
In normal and neoplastic cell types, EMP2 previously has been shown to promote autonomous VEGF expression, a phenotype that could be reversed by molecular inhibition of EMP2 expression or antibody blockade with anti-EMP2 antibody.17,22,29,31 These precedents, and EMP2 expression in corneal epithelium, formed the rationale for testing whether EMP2 blockade could block corneal neovascularization.
We demonstrated that blocking EMP2 signaling results in a time dependent decrease in EMP2 expression as well as VEGF expression. Our experiments showed that after anti-EMP2 blockade, expression of EMP2 protein reached a nadir after 12 to 24 hours. Correspondingly, VEGF secretion was decreased between 6 and 24 hours, with a nadir around 12 hours. This is consistent with our hypothesis that VEGF expression decreases in response to an EMP2 decrease, with the caveat that use of the anti-EMP2 blocking antibody does not characterize the relative production of EMP2 and VEGF protein in a time dependent manner. However, previous experiments have shown that siRNA knock-down of EMP2 reduces total VEGF expression by 57%, and conversely EMP2 overexpression increased VEGF expression by 1.5-fold.31
The expression of the growth factor VEGF is complex and regulated by many factors at the transcription, translation, and secretion levels. Rapid release is possible due to preexisting pools of protein regulated at the secretion level, with inducible secretion seen as rapidly as within 30 min in human vascular smooth muscle cells, platelets, and neutrophils,40 as well as neuroblastoma tumor cells.41 Additionally, certain ocular cell models (retinal pigment epithelium/choroid in ex vivo organ culture42 and the human retinal pigment epithelium cell line ARPE-1943) constitutively express and secrete VEGF, with their constitutive secretion further modifiable by external factors. Furthermore, low levels of constitutive expression of VEGF-A has also been reported in human corneal epithelial cells and human corneal stromal fibroblasts,44 corroborating evidence here that VEGF and EMP2 play integral roles in the corneal vascular state.
Anti-VEGF antibody therapy is an FDA approved and clinically successful treatment for multiple conditions involving abnormal angiogenesis, including retinal neovascularization.45 Several direct VEGF pathway inhibitors are currently FDA approved, including various classes of biologicals and orally available small molecule downstream tyrosine kinase inhibitors.46–49 In addition to therapeutic efficacy in several human cancers,50 anti-VEGF immunotherapy has an established role in ophthalmology,51 including age-related macular degeneration52,53 and proliferative diabetic retinopathy.54 Additionally, anti-VEGF therapy has evidence of efficacy in other neovascular diseases, including diabetic macular edema,55,56 neovascular glaucoma,57 branch retinal vein occlusion, and central retinal vein occlusion,58–60 iris neovascularization,61 and retinopathy of prematurity.62–65
However, adverse events may occur as a clinical factor in therapeutic VEGF inhibition. This includes systemic vascular toxicity such as arterial and venous thromboembolic events and its cardiac complications,66,67 and systemic effects of intraocular administration in one large meta-analysis68 (although not observed in other studies).69,70 There is also clinical evidence of local toxicity from VEGF blockade,71,72 including acute and chronic elevated intraocular pressure.73,74
Based on the present findings, anti-EMP2 antibody therapy might offer a biologically distinct strategy to reduce neovascularization. Moreover, it offers a novel treatment option that may avoid some of the side effects inherent in anti-VEGF therapy,15,75 while maintaining its inhibitory effects on neovascularization and angiogenesis. Similar to some studies using VEGF antibodies in treatment of corneal neovascularization,7,8,14 a minimally invasive subconjunctival injection route of anti-EMP2 antibody is effective in this model. Anti-EMP2 human monoclonal antibody has already shown promise in preclinical testing against both breast cancer16 and glioblastoma.21,22 Additionally, polyclonal EMP2 blocking antibodies have been used with ARPE-19 cells in the successful treatment of a rabbit model of experimental proliferative vitreoretinopathy with no evidence of toxicity to the eye by histology29 or by electroretinography (Telander D, unpublished observations, 2010). In summary, anti-EMP2 immunotherapy has efficacy in prevention of corneal neovascularization in the murine burn model. Additional studies are warranted to explore the possibility of this target in human ocular neovascular disease.
Supplementary Material
Acknowledgments
Supported by NIH R01 CA163971 (MW), NCATS UL1 TR001881, and an unrestricted grant from Research to Prevent Blindness, Inc. to the Department of Ophthalmology at UCLA.
Disclosure: M.M. Sun, None; A.M. Chan, None; S.M. Law, None; S. Duarte, None; D. Diaz-Aguilar, None; M. Wadehra, Oncoresponse (C), P; L.K. Gordon, P
References
- 1.Ambati BK, Nozaki M, Singh N, et al. Corneal avascularity is due to soluble VEGF receptor-1. Nature. 2006;443:993–997. doi: 10.1038/nature05249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shakiba Y, Mansouri K, Arshadi D, Rezaei N. Corneal neovascularization: molecular events and therapeutic options. Recent Pat Inflamm Allergy Drug Discov. 2009;3:221–231. doi: 10.2174/187221309789257450. [DOI] [PubMed] [Google Scholar]
- 3.Cursiefen C, Chen L, Borges LP, et al. VEGF-A stimulates lymphangiogenesis and hemangiogenesis in inflammatory neovascularization via macrophage recruitment. J Clin Invest. 2004;113:1040–1050. doi: 10.1172/JCI20465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chang JH, Gabison EE, Kato T, Azar DT. Corneal neovascularization. Curr Opin Ophthalmol. 2001;12:242–249. doi: 10.1097/00055735-200108000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Whitcher JP, Srinivasan M, Upadhyay MP. Corneal blindness: a global perspective. Bull World Health Organ. 2001;79:214–221. [PMC free article] [PubMed] [Google Scholar]
- 6.Qazi Y, Wong G, Monson B, Stringham J, Ambati BK. Corneal transparency: genesis, maintenance and dysfunction. Brain Res Bull. 2010;81:198–210. doi: 10.1016/j.brainresbull.2009.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chang J-H, Garg NK, Lunde E, Han K-Y, Jain S, Azar DT. Corneal neovascularization: an anti-VEGF therapy review. Surv Ophthalmol. 2012;57:415–429. doi: 10.1016/j.survophthal.2012.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Voiculescu OB, Voinea LM, Alexandrescu C. Corneal neovascularization and biological therapy. J Med Life. 2015;8:444–448. [PMC free article] [PubMed] [Google Scholar]
- 9.Keating AM, Jacobs DS. Anti-VEGF treatment of corneal neovascularization. Ocul Surf. 2011;9:227–237. doi: 10.1016/s1542-0124(11)70035-0. [DOI] [PubMed] [Google Scholar]
- 10.Avisar I, Weinberger D, Kremer I. Effect of subconjunctival and intraocular bevacizumab injections on corneal neovascularization in a mouse model. Curr Eye Res. 2010;35:108–115. doi: 10.3109/02713680903429007. [DOI] [PubMed] [Google Scholar]
- 11.Bahar I, Kaiserman I, McAllum P, Rootman D, Slomovic A. Subconjunctival bevacizumab injection for corneal neovascularization. Cornea. 2008;27:142–147. doi: 10.1097/ICO.0b013e318159019f. [DOI] [PubMed] [Google Scholar]
- 12.Bock F, König Y, Kruse F, Baier M, Cursiefen C. Bevacizumab (Avastin) eye drops inhibit corneal neovascularization. Graefes Arch Clin Exp Ophthalmol. 2008;246:281–284. doi: 10.1007/s00417-007-0684-4. [DOI] [PubMed] [Google Scholar]
- 13.Lipp M, Bucher F, Parthasarathy A, et al. Blockade of the VEGF isoforms in inflammatory corneal hemangiogenesis and lymphangiogenesis. Graefes Arch Clin Exp Ophthalmol. 2014;252:943–949. doi: 10.1007/s00417-014-2626-2. [DOI] [PubMed] [Google Scholar]
- 14.Yoo AR, Chung SK. Effects of subconjunctival tocilizumab versus bevacizumab in treatment of corneal neovascularization in rabbits. Cornea. 2014;33:1088–1094. doi: 10.1097/ICO.0000000000000220. [DOI] [PubMed] [Google Scholar]
- 15.Ghasemi Falavarjani K, Nguyen QD. Adverse events and complications associated with intravitreal injection of anti-VEGF agents: a review of literature. Eye. 2013;27:787–794. doi: 10.1038/eye.2013.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fu M, Maresh EL, Helguera GF, et al. Rationale and preclinical efficacy of a novel anti-EMP2 antibody for the treatment of invasive breast cancer. Mol Cancer Ther. 2014;13:902–915. doi: 10.1158/1535-7163.MCT-13-0199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gordon LK, Kiyohara M, Fu M, et al. EMP2 regulates angiogenesis in endometrial cancer cells through induction of VEGF. Oncogene. 2013;32:5369–5376. doi: 10.1038/onc.2012.622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fu M, Rao R, Sudhakar D, et al. Epithelial membrane protein-2 promotes endometrial tumor formation through activation of FAK and Src. PLoS One. 2011;6:e19945. doi: 10.1371/journal.pone.0019945. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 19.Fu M, Brewer S, Olafsen T, et al. Positron emission tomography imaging of endometrial cancer using engineered anti-EMP2 antibody fragments. Mol Imaging Biol. 2012;15:68–78. doi: 10.1007/s11307-012-0558-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Habeeb O, Goodglick L, Soslow RA, et al. Epithelial membrane protein-2 expression is an early predictor of endometrial cancer development. Cancer. 2010;116:4718–4726. doi: 10.1002/cncr.25259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Qin Y, Fu M, Takahashi M, et al. Epithelial membrane protein-2 (EMP2) activates Src protein and is a novel therapeutic target for glioblastoma. J Biol Chem. 2014;289:13974–13985. doi: 10.1074/jbc.M113.543728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Qin Y, Takahashi M, Sheets K, et al. Epithelial membrane protein-2 (EMP2) promotes angiogenesis in glioblastoma multiforme. J Neurooncol. 2017;14(suppl 5):v1. doi: 10.1007/s11060-017-2507-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chung LK, Bhatt NS, Lagman C, et al. Epithelial membrane protein 2: molecular interactions and clinical implications. J Clin Neurosci. 2017;44:84–88. doi: 10.1016/j.jocn.2017.06.044. [DOI] [PubMed] [Google Scholar]
- 24.Williams CJ, Chu A, Jefferson WN, et al. Epithelial membrane protein 2 (EMP2) deficiency alters placental angiogenesis, mimicking features of human placental insufficiency. J Pathol. 2017;242:246–259. doi: 10.1002/path.4893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang CX, Wadehra M, Fisk BC, Goodglick L, Braun J. Epithelial membrane protein 2, a 4-transmembrane protein that suppresses B-cell lymphoma tumorigenicity. Blood. 2001;97:3890–3895. doi: 10.1182/blood.v97.12.3890. [DOI] [PubMed] [Google Scholar]
- 26.Wadehra M, Sulur GG, Braun J, Gordon LK, Goodglick L. Epithelial membrane protein-2 is expressed in discrete anatomical regions of the eye. Exp Mol Pathol. 2003;74:106–112. doi: 10.1016/s0014-4800(03)00009-1. [DOI] [PubMed] [Google Scholar]
- 27.Morales SA, Mareninov S, Wadehra M, et al. FAK activation and the role of epithelial membrane protein 2 (EMP2) in collagen gel contraction. Invest Ophthalmol Vis Sci. 2009;50:462–469. doi: 10.1167/iovs.07-1598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Morales SA, Mareninov S, Coulam P, et al. Functional consequences of interactions between FAK and epithelial membrane protein 2 (EMP2) Invest Ophthalmol Vis Sci. 2009;50:4949–4956. doi: 10.1167/iovs.08-3315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Telander DG, Morales SA, Mareninov S, Forward K, Gordon LK. Epithelial membrane protein-2 (EMP2) and experimental proliferative vitreoretinopathy (PVR) Curr Eye Res. 2011;36:546–552. doi: 10.3109/02713683.2011.561468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Telander DG, Yu AK, Forward KI, et al. Epithelial membrane protein-2 in human proliferative vitreoretinopathy and epiretinal membranes. Invest Ophthalmol Vis Sci. 2016;57:3112–3117. doi: 10.1167/iovs.15-17791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Morales SA, Telander DG, Leon D, et al. Epithelial membrane protein 2 controls VEGF expression in ARPE-19 cells. Invest Ophthalmol Vis Sci. 2013;54:2367–2372. doi: 10.1167/iovs.12-11013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Anderson C, Zhou Q, Wang S. An alkali-burn injury model of corneal neovascularization in the mouse. J Vis Exp. 2014. pp. e51159–e51159. [DOI] [PMC free article] [PubMed]
- 33.Longair MH, Baker DA, Armstrong JD. Simple neurite tracer: open source software for reconstruction, visualization and analysis of neuronal processes. Bioinformatics. 2011;27:2453–2454. doi: 10.1093/bioinformatics/btr390. [DOI] [PubMed] [Google Scholar]
- 34.Güell JL, Husseiny El MA, Manero F, Gris O, Elies D. Historical review and update of surgical treatment for corneal endothelial diseases. Ophthalmol Ther. 2014;3:1–15. doi: 10.1007/s40123-014-0022-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Holyoake TL, Alcorn MJ, Franklin IM. The CD34 antigen: potential clinical advantages of CD34 selection. Clin Oncol (R Coll Radiol) 1996;8:214–221. doi: 10.1016/s0936-6555(05)80655-7. [DOI] [PubMed] [Google Scholar]
- 36.Arbab AS. Stem Cells and Cancer Stem Cells, Volume 9: Therapeutic Applications in Disease and Injury. Dordrecht: Springer;; 2013. CD34+/AC133+ Endothelial progenitor cells as imaging probes for neovascularization of tumors; pp. 203–217. [Google Scholar]
- 37.Wadehra M, Iyer R, Goodglick L, Braun J. The tetraspan protein epithelial membrane protein-2 interacts with β1 integrins and regulates adhesion. J Biol Chem. 2002;277:41094–41100. doi: 10.1074/jbc.M206868200. [DOI] [PubMed] [Google Scholar]
- 38.Forbes A, Wadehra M, Mareninov S, et al. The tetraspan protein EMP2 regulates expression of caveolin-1. J Biol Chem. 2007;282:26542–26551. doi: 10.1074/jbc.M702117200. [DOI] [PubMed] [Google Scholar]
- 39.Wadehra M, Su H, Gordon LK, Goodglick L, Braun J. The tetraspan protein EMP2 increases surface expression of class I major histocompatibility complex proteins and susceptibility to CTL-mediated cell death. Clin Immunol. 2003;107:129–136. doi: 10.1016/s1521-6616(03)00048-2. [DOI] [PubMed] [Google Scholar]
- 40.Koehne P, Willam C, Strauss E, Schindler R, Eckardt KU, Bührer C. Lack of hypoxic stimulation of VEGF secretion from neutrophils and platelets. Am J Physiol Heart Circ Physiol. 2000;279:H817–H824. doi: 10.1152/ajpheart.2000.279.2.H817. [DOI] [PubMed] [Google Scholar]
- 41.Schlegel C, Paul P, Lee S, et al. Protein kinase C regulates bombesin-induced rapid VEGF secretion in neuroblastoma cells. Anticancer Res. 2012;32:4691–4696. [PMC free article] [PubMed] [Google Scholar]
- 42.Klettner A, Westhues D, Lassen J, Bartsch S, Roider J. Regulation of constitutive vascular endothelial growth factor secretion in retinal pigment epithelium/choroid organ cultures: p38, nuclear factor κB, and the vascular endothelial growth factor receptor-2/phosphatidylinositol 3 kinase pathway. Mol Vis. 2013;19:281–291. [PMC free article] [PubMed] [Google Scholar]
- 43.Puddu A, Sanguineti R, Durante A, Nicolò M, Viviani GL. Vascular endothelial growth factor-C secretion is increased by advanced glycation end-products: possible implication in ocular neovascularization. Mol Vis. 2012;18:2509–2517. [PMC free article] [PubMed] [Google Scholar]
- 44.Kommineni VK, Nagineni CN, William A, Detrick B, Hooks JJ. IFN-gamma acts as anti-angiogenic cytokine in the human cornea by regulating the expression of VEGF-A and sVEGF-R1. Biochem Biophys Res Commun. 2008;374:479–484. doi: 10.1016/j.bbrc.2008.07.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kim LA, D'Amore PA. A brief history of anti-VEGF for the treatment of ocular angiogenesis. Am J Pathol. 2012;181:376–379. doi: 10.1016/j.ajpath.2012.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kong D-H, Kim MR, Jang JH, Na H-J, Lee S. A review of anti-angiogenic targets for monoclonal antibody cancer therapy. Int J Mol Sci. 2017;18:1786. doi: 10.3390/ijms18081786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rejdak R. New drug VEGF Trap-Eye – Eylea in the treatment of age-related macular degeneration, and macular edema in central retinal vein occlusion and diabetic retinopathy. Pharmacol Rep. 2013;65:26. [Google Scholar]
- 48.Aparicio LMA, Fernandez IP, Cassinello J. Tyrosine kinase inhibitors reprogramming immunity in renal cell carcinoma: rethinking cancer immunotherapy. Clin Transl Oncol. 2017;5:257–258. doi: 10.1007/s12094-017-1657-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wong HH, Eisen T. Renal Cell Carcinoma. New York, NY: Springer;; 2015. First-generation tyrosine kinase inhibitors: clinical results; pp. 177–205. [Google Scholar]
- 50.Al-Abd AM, Alamoudi AJ, Abdel-Naim AB, Neamatallah TA, Ashour OM. Anti-angiogenic agents for the treatment of solid tumors: potential pathways, therapy and current strategies – a review. J Adv Res. 2017;8:591–605. doi: 10.1016/j.jare.2017.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pożarowska D, Pożarowski P. The era of anti-vascular endothelial growth factor (VEGF) drugs in ophthalmology, VEGF and anti-VEGF therapy. Cent Eur J Immunol. 2016;3:311–316. doi: 10.5114/ceji.2016.63132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rosenfeld PJ, Brown DM, Heier JS, et al. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med. 2006;355:1419–1431. doi: 10.1056/NEJMoa054481. [DOI] [PubMed] [Google Scholar]
- 53.Folk JC, Stone EM. Ranibizumab therapy for neovascular age-related macular degeneration. N Engl J Med. 2010;363:1648–1655. doi: 10.1056/NEJMct1000495. [DOI] [PubMed] [Google Scholar]
- 54.Li X, Zarbin MA, Bhagat N. Anti-vascular endothelial growth factor injections: the new standard of care in proliferative diabetic retinopathy? Dev Ophthalmol. 2017;60:131–142. doi: 10.1159/000459699. [DOI] [PubMed] [Google Scholar]
- 55.Nguyen QD, Shah SM, Khwaja AA, et al. Two-year outcomes of the ranibizumab for edema of the macula in diabetes (READ-2) study. Ophthalmology. 2010;117:2146–2151. doi: 10.1016/j.ophtha.2010.08.016. [DOI] [PubMed] [Google Scholar]
- 56.Virgili G, Parravano M, Evans JR, Gordon I, Lucenteforte E. Anti-vascular endothelial growth factor for diabetic macular oedema: a network meta-analysis. Virgili G, editor. Cochrane Database Syst Rev. 2017;6:CD007419. doi: 10.1002/14651858.CD007419.pub5. ed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Simha A, Braganza A, Abraham L, Samuel P, Lindsley K. Anti-vascular endothelial growth factor for neovascular glaucoma. Cochrane Database Syst Rev. 2013;66:CD007920. doi: 10.1002/14651858.CD007920.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Thach AB, Yau L, Hoang C, Tuomi L. Time to clinically significant visual acuity gains after ranibizumab treatment for retinal vein occlusion: BRAVO and CRUISE trials. Ophthalmology. 2014;121:1059–1066. doi: 10.1016/j.ophtha.2013.11.022. [DOI] [PubMed] [Google Scholar]
- 59.Varma R, Bressler NM, Suñer I, et al. Improved vision-related function after ranibizumab for macular edema after retinal vein occlusion: results from the BRAVO and CRUISE trials. Ophthalmology. 2012;119:2108–2118. doi: 10.1016/j.ophtha.2012.05.017. [DOI] [PubMed] [Google Scholar]
- 60.Braithwaite T, Nanji AA, Lindsley K, Greenberg PB. Anti-vascular endothelial growth factor for macular oedema secondary to central retinal vein occlusion. Cochrane Database Syst Rev. 2014;119:CD007325. doi: 10.1002/14651858.CD007325.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Altintas AGK, Arifoglu HB, Tutar E, Koklu G, Ozcan PY. Effect on anterior chamber bevacizumab injection combined with seton implantation in treatment of rubeosis iridis in neovascular glaucoma. Cutan Ocul Toxicol. 2012;31:124–127. doi: 10.3109/15569527.2011.621917. [DOI] [PubMed] [Google Scholar]
- 62.Mintz-Hittner HA, Kennedy KA, Chuang AZ;, BEAT-ROP Cooperative Group Efficacy of intravitreal bevacizumab for stage 3+ retinopathy of prematurity. N Engl J Med. 2011;364:603–615. doi: 10.1056/NEJMoa1007374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mintz-Hittner HA, Best LM. Antivascular endothelial growth factor for retinopathy of prematurity. Curr Opin Pediatr. 2009;21:182–187. doi: 10.1097/MOP.0b013e32832925f9. [DOI] [PubMed] [Google Scholar]
- 64.Reynolds JD. Bevacizumab for retinopathy of prematurity. N Engl J Med. 2011;364:677–678. doi: 10.1056/NEJMe1100248. [DOI] [PubMed] [Google Scholar]
- 65.Stockman JA., III. Efficacy of intravitreal bevacizumab for stage 3+ retinopathy of prematurity. Yearbook of Pediatrics. 2012;2012:511–513. [Google Scholar]
- 66.Ziemssen F, Sobolewska B, Deissler H, Deissler H. Safety of monoclonal antibodies and related therapeutic proteins for the treatment of neovascular macular degeneration: addressing outstanding issues. Expert Opin Drug Saf. 2016;15:75–87. doi: 10.1517/14740338.2016.1121232. [DOI] [PubMed] [Google Scholar]
- 67.Di Lisi D, Madonna R, Zito C, et al. Anticancer therapy-induced vascular toxicity: VEGF inhibition and beyond. Int J Cardiol. 2017;227:11–17. doi: 10.1016/j.ijcard.2016.11.174. [DOI] [PubMed] [Google Scholar]
- 68.Ueta T, Noda Y, Toyama T, Yamaguchi T, Amano S. Systemic vascular safety of ranibizumab for age-related macular degeneration. Ophthalmology. 2014;121:2193–2203.e2197. doi: 10.1016/j.ophtha.2014.05.022. [DOI] [PubMed] [Google Scholar]
- 69.Scott LJ, Chakravarthy U, Reeves BC, Rogers CA. Systemic safety of anti-VEGF drugs: a commentary. Expert Opin Drug Saf. 2015;14:379–388. doi: 10.1517/14740338.2015.991712. [DOI] [PubMed] [Google Scholar]
- 70.Thulliez M, Angoulvant D, Le Lez ML, et al. Cardiovascular events and bleeding risk associated with intravitreal antivascular endothelial growth factor monoclonal antibodies. JAMA Ophthalmol. 2014;132:1317–1326. doi: 10.1001/jamaophthalmol.2014.2333. [DOI] [PubMed] [Google Scholar]
- 71.Fasih U, Shaikh N, Rahman A, Sultan S, Fehmi MS, Shaikh A. A one-year follow-up study of ocular and systemic complications of intravitreal injection of bevacizumab (Avastin) J Pak Med Assoc. 2013;63:707–710. [PubMed] [Google Scholar]
- 72.Penha FM, Rodrigues EB, Furlani BA, Dib E, Melo GB, Farah ME. Toxicological considerations for intravitreal drugs. Expert Opin Drug Metab Toxicol. 2011;7:1021–1034. doi: 10.1517/17425255.2011.585970. [DOI] [PubMed] [Google Scholar]
- 73.Good TJ, Kimura AE, Mandava N, Kahook MY. Sustained elevation of intraocular pressure after intravitreal injections of anti-VEGF agents. Br J Ophthalmol. 2011;95:1111–1114. doi: 10.1136/bjo.2010.180729. [DOI] [PubMed] [Google Scholar]
- 74.Horsley MB, Mandava N, Maycotte MA, Kahook MY. Retinal nerve fiber layer thickness in patients receiving chronic anti-vascular endothelial growth factor therapy. Am J Ophthalmol. 2010;150:558–561.e1. doi: 10.1016/j.ajo.2010.04.029. [DOI] [PubMed] [Google Scholar]
- 75.Giet M, Henkel C, Schuchardt M, Tolle M. Anti-VEGF drugs in eye diseases: local therapy with potential systemic effects. Curr Pharm Des. 2015;21:3548–3556. doi: 10.2174/1381612821666150225120314. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.