Abstract
Background: Childhood social risk has been associated with increased risk of childhood obesity. However, little is known about early exposure of cumulative social risk on BMI percentile (BMIp) trajectories in early childhood.
Methods: Public data from the Fragile Families and Child Wellbeing Study were analyzed (N = 3809). Maternal reports of experiences of multiple social risk factors were obtained at age 1 and 3 assessments of children. Two cumulative social risk scores were calculated by summing social factors assessed at age 1 and at age 3. Child BMIp was assessed at ages 3, 5, and 9. Linear mixed models were used to examine the effect of cumulative social risk on sex-specific BMIp trajectories.
Results: Compared with girls experiencing low social risk at either age 1 or 3, girls experiencing high social risk (≥ 2 factors) at age 1 or 3 only had higher initial BMIp at age 3 [β0 = 5.70 (95% confidence interval, CI: 0.15–1.26) and 1.37 (95% CI: −2.25 to 4.99), respectively] and had nonsignificantly greater BMIp growth rate [β1 = 0.39 (95% CI: −0.86 to 1.63) and 0.32 (95% CI: −0.86 to 1.63)]. Girls experiencing high social risk at both ages had nonsignificantly but consistently lower BMIp [β1 = −1.24 (95% CI: −2.93 to 0.46)]. In addition, girls experiencing a sum of ≥4 risk factors at both ages had lower BMIp growth rate [β1 = −1.77 (95% CI: −3.39 to −0.15)] compared to girls experiencing no risk factor. No associations were observed among boys.
Conclusions: Early exposure to cumulative social risk may have long-term impact on BMIp trajectories among girls, depending on timing of exposure. Understanding the effect of cumulative social risk in different contexts, including sex, chronicity, and timing of exposure, may have practical implications for informing effective intervention to combat childhood obesity.
Keywords: child abuse, food insecurity, housing insecurity, maternal depression, obesity, social stress
Introduction
Obesity is a major public health problem in the United States and a known risk factor for cardiovascular disease, cancer, and diabetes,1 especially among racial/ethnic minorities.2,3 National data from 2003 to 2007 showed that obesity prevalence increased by 23%–33% for children in low-income households. In 2007, ∼17% of children and adolescents were obese in the United States, with even higher prevalence among African American and Latino children and children from single mother households.3 Both higher BMI percentile (BMIp) and higher growth rate of BMIp in early life have been shown to predict later obesity in adolescence and adulthood.4–7 Therefore, understanding risk factors associated with BMIp increase in early life may provide opportunities for early prevention.
The high prevalence of obesity is multifactorial, including genetic, social, and environmental factors. An increasing body of literature has examined the impact of early social contexts and psychological and social stress on obesity.8–13 Chronic stress has been shown to disrupt behavioral and physiological mechanisms increasing risk for obesity development.10,14–16 Among children, single parent family structures and family dysfunction such as intimate partner violence (IPV), child abuse, and neglect have been associated with obesity, with several studies noting associations among girls.12,17–21 It is hypothesized that family dysfunction may be linked to obesity through limited parental availability for feeding, increased stress and dysregulation of hypothalamic-pituitary axis linked to hormonal changes, and unhealthy behaviors such as impulsive eating.18 In addition to family dysfunction, food and housing insecurity have also been associated with childhood obesity. Children in food-insecure households, for example, may have a diet relying more heavily on energy-dense food and, therefore, have a higher risk of weight gain.21–24 Housing insecurity can induce disruption of sleep and eating routines, which could promote changes in BMI in addition to affecting behavioral and emotional well-being.20 A recent review also showed the positive association between cumulative adverse childhood events and childhood overweight.25 However, most of these studies have relied on cross-sectional analyses, while very few longitudinal analyses targeted children 10 years of age or older.8,10 In previous analyses among participants of the Fragile Families and Child Wellbeing study (FFCWS),12 we note that cumulative social risk, at specific time points, is associated with higher odds of obesity among preschool girls, but no associations were noted among boys. Those experiencing high cumulative risk at multiple time points were not at statistically significant odds of being obese. However, little is known about the effect of early social risk exposure on BMIp trajectories in earlier life before 10 years of age, and it is unknown whether these associations remain as children grow into the preadolescent period.
As growing evidence shows that early childhood may be a “sensitive period” for obesity development and thus a time for prioritizing obesity prevention efforts,5,26,27 particularly because behaviors and/or physiology are more modifiable and norms developed early often lay the foundation for future trajectories of health,28 we examine the role of cumulative social risk on chronicity and timing on developmental trajectories of BMIp. Because sex differences in the association between psychosocial factors and obesity have been documented in previous studies, analyses were stratified by sex.12
Methods
Data Source
Data from the FFCWS were used for analyses. The FFCWS has been following a cohort of 4898 children randomly sampled according to maternal marital status (with a ratio of 3:1 for unmarried vs. married) during childbirth from 75 hospitals in 20 US cities.29 The FFCWS consists of interviews with mothers at birth and at year 1, 3, 5, and 9 and in-home assessments of children at year 3, 5, and 9, collecting information on sociodemographic characteristics, parenting behavior, and health status. We restricted analyses to children with identifiable sex information (n = 4897). Analyses were further restricted to children with complete information on height and weight and therefore BMIp in at least one of the 3-, 5-, and 9-year in-home assessments (N = 3809). Multiple imputation techniques were used to impute missing BMIp and covariates of interest. Comparison of the full sample (n = 4897) and analytic sample (n = 3809) by sociodemographics demonstrated that the analytic sample is comparable to the full sample (Supplementary Table S1; Supplementary Data are available online at www.liebertpub.com/chi).
Child BMIp
Height and weight of children were measured during 3-, 5-, and 9-year in-home assessments. The Centers for Disease Control and Prevention BMI growth reference chart was used to calculate age- and sex-specific BMIp.
Social Risk Factors
Food insecurity, housing insecurity, maternal IPV, depression, and substance use, and paternal incarceration were assessed at both year 1 and 3. Child abuse and neglect were assessed at year 3 only.
Food insecurity
Derived from questions in the Survey of Income and Program Participation, mothers were asked whether they or their children had encountered hunger but could not afford enough food in the past year, which were derived from the Survey of Income and Program Participation.30 Mothers responding “Yes” to either question were defined as experiencing food insecurity.
Housing insecurity
Mothers were asked whether they were evicted from home, didn't pay full rent or mortgage, moved in with people because of financial problems, or stayed in a place not meant for regular housing such as shelter, car, or abandoned building in the past year. These questions were derived from the Survey of Income and Program Participation and the New York City Social Indicators Survey.30,31 Mothers responding “Yes” to any questions were defined as experiencing housing insecurity.
Maternal IPV
Mothers were asked how often they were slapped/kicked, hit with fist/dangerous object, or forced to have sex/do sexual things by father/partner and whether these physical and sexual violence occurred during last month of relationship. They were also asked whether they were ever cut/bruised/seriously hurt in fight with father/partner or slapped/kicked by father/partner. The survey questions were derived from The Effect of Violence on Work and Family Project survey and The Design and Content of the National Survey of Families and Households.32,33 Mothers answering “Sometimes” or “Often” for the questions regarding violence frequency or answering “Yes” to the other questions were defined as experiencing IPV.
Maternal depression
Maternal depression was assessed through the Composite International Diagnostic Interview Short Form, a screening for depression that is based on one of the most widely used structured diagnostic interviews to assess adult psychiatric disorders in epidemiological studies.34,35 This tool was scored consistent with the developer's guidelines, which generates probable diagnosis of psychiatric disorders consistent with the DSMIV: Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition (American Psychological Association, Washington, DC, 1994). Mothers meeting the conservative depression criteria were defined as experiencing depression.
Maternal substance use
Mothers were asked whether they had >5 alcohol drinks in a day, had marijuana/pot/cocaine/crack/speed/lysergic acid diethylamide/heroin/other hard drug, had drinking/drugs interfered with their daily life or relationship, and had sought help or been treated for drug/alcohol problems in the past week. Mothers responding “Yes” to any question were defined as experiencing substance use.
Paternal incarceration
Mothers were asked whether the father of child was currently in jail.
Child neglect
Mothers were asked in past month how often they left their children at home alone but thought some adult should be with children, were so caught up with their own problems that they were not able to show love to child, were not able to make sure their children got their food when needed, were not able to make sure children went to a doctor/hospital when needed, and were so drunk/high that they had a problem taking care of their children. These questions were derived from the Parent Child Conflict Tactics Scale.36 Mothers answering ≥3 times for any question were defined as neglect.
Child abuse
Mothers were asked how often in past month they spanked their children on the bottom with bare hand, hit children on bottom with hard object (belt/hairbrush/stick/other), slapped children hand/arm/leg, pinched children, shook children, shouted/yelled/screamed at children, threatened to spank/hit children but did not actually do it, swore/cursed at children, called children dumb/lazy/other name like that, and said they would send children away/kick children out of house, which were derived from the Parent Child Conflict Tactics Scale.36 Mothers answering ≥3 times for any question were defined as abuse.
Cumulative social index
Two cumulative risk variables were created, one indicating chronicity of cumulative risk and the other indicating chronicity and timing of cumulative risk, as defined in previous analyses.12
Dichotomous variables were created for each social factor. A score of 1 for each item indicated presence of specific social risk factor in specific year. The risk score at age 1 was created by summing the six dichotomous variables (including maternal depression, substance use, and IPV, housing and food insecurity, and paternal incarceration), possibly ranging 0–6. The risk score at age 3 was created by summing the eight dichotomous variables (including the six factors above plus child neglect and abuse), possibly ranging 0–8. The final risk score was created by summing the score at year 1 and 3, categorized as none, 1, 2–3, and ≥4 risk factors. Higher scores indicate higher level of cumulative social risk exposure.
To additionally assess both timing and chronicity of social risk exposure, risk scores of each year were dichotomized. Children experiencing ≥2 risk factors in each year were defined as experiencing high social risk in specific year. Sensitivity analyses were conducted defining the high cumulative risk threshold. A final four-level high cumulative risk variable was then created and characterized as: high risk in both year 1 and 3, year 3 only, year 1 only, and neither year 1 nor 3.
Covariates
Information on race/ethnicity (African American, Hispanic, White/other), maternal education (less than high school, high school or equivalent, college/some college), and low birth weight (LBW) was collected at baseline. Maternal marital status (married/cohabitating or not), public assistance receipt (yes, no), and maternal BMI were collected at year 3.
Statistical Methods
Linear mixed models (LMM) with random intercepts and slopes were used to examine the association between the sum of cumulative social risk score at year 1 and 3 (categorized as 0, 1, 2–3, and ≥4) on BMIp trajectories across age 3, 5, and 9 years.12,37 A second model examined timing of exposure by examining the impact of high social risk at year 1 or 3 (categorized as risk score ≥2 in both year 1 and 3, year 1 only, year 3 only, and neither year) on BMIp trajectories across ages 3, 5, and 9 years.12,37 All analyses were stratified by sex and adjusted for race/ethnicity, public assistance, LBW, maternal education, marital status, and maternal BMI,12 using SAS 9.4. Multiple imputations were conducted to impute missing data38 among the sample (N = 3809). Five imputations were conducted and combined for analyses.39
We also conducted a series of sensitivity analyses. First, the impact of individual stressors and individual cumulative risk score at year 1 and 3 on BMIp trajectories was also examined, respectively (Supplementary Tables S2 and S3). Sensitivity analyses were also conducted using different characterization of cumulative social risk and using only six risk factors at age 3 excluding child abuse and neglect to create the social risk score (Supplementary Tables S4–S6).
Results
Table 1 shows distribution of demographic characteristics, BMIp, and social risk score. Mean BMIp was 62.19, 65.0, and 69.0 across three waves. Statistically significant sex differences were observed in the distribution of cumulative social risk indicators.
Table 1.
Demographic Characteristics, BMI Percentile, and Social Risk Factors: Fragile Families and Child Wellbeing Study (N = 3809)
| Total sample | Girls | Boys | ||
|---|---|---|---|---|
| Characteristic | (N = 3809) | (n = 1825) | (n = 1984) | p-Value |
| Race/ethnicity—n (%) | 0.054 | |||
| White/other | 888 (23.32) | 417 (22.86) | 471 (23.74) | |
| Hispanic | 1014 (26.62) | 500 (27.39) | 514 (25.91) | |
| African American | 1907 (50.07) | 908 (49.75) | 999 (50.35) | |
| Mother's highest education—n (%) | 0.892 | |||
| College or some college | 1292 (33.93) | 620 (33.98) | 672 (33.88) | |
| High school or equivalent | 1002 (26.31) | 477 (26.15) | 525 (26.45) | |
| Less than high school | 1515 (39.76) | 728 (39.87) | 787 (39.67) | |
| Maternal marital status: married or cohabitating—n (%) | 1919 (50.38) | 927 (50.81) | 992 (49.99) | 0.261 |
| Receipt of public assistance—n (%) | 1551 (40.72) | 742 (40.64) | 809 (40.8) | 0.822 |
| Low birth weight—n (%) | 369 (9.68) | 193 (10.59) | 175 (8.84) | <0.001 |
| Maternal BMI—kg/m2 (±SE) | 29.56 (±0.05) | 29.82 (±0.08) | 29.33 (±0.07) | <0.001 |
| Mean BMIp at age 3 years (±SE) | 62.19 (±0.20) | 62.14 (±0.30) | 62.23 (±0.28) | 0.834 |
| Mean BMIp at age 5 years (±SE) | 65.00 (±0.19) | 65.07 (±0.28) | 64.39 (±0.26) | 0.072 |
| Mean BMIp at age 9 years (±SE) | 69.00 (±0.20) | 69.16 (±0.30) | 69.18 (±0.27) | 0.961 |
| Obesity at age 3 years—n (%) | 495 (12.99) | 230 (12.62) | 264 (13.33) | 0.150 |
| Obesity at age 5 years—n (%) | 456 (11.98) | 232 (12.72) | 224 (11.29) | 0.002 |
| Obesity at age 9 years—n (%) | 873 (22.93) | 441 (24.18) | 432 (21.78) | <0.001 |
| Cumulative social risk | 0.037 | |||
| Cumulative social risk (0) | 856 (22.48) | 420 (23.04) | 436 (21.98) | |
| Cumulative social risk (1) | 1148 (30.14) | 560 (30.67) | 588 (29.65) | |
| Cumulative social risk (2–3) | 1224 (32.13) | 574 (31.45) | 650 (32.75) | |
| Cumulative social risk (≥4) | 581 (15.25) | 271 (14.84) | 310 (15.63) | |
| High cumulative social risk (≥2 risk factors) | <0.001 | |||
| Both age 1 and 3 years | 368 (9.67) | 173 (9.49) | 195 (9.84) | |
| Age 3 years only | 856 (22.46) | 377 (20.65) | 479 (24.13) | |
| Age 1 year only | 234 (6.15) | 123 (6.73) | 111 (5.61) | |
| Neither age 1 nor 3 years | 2351 (61.72) | 1152 (63.13) | 1199 (60.41) |
The statistically significant results at an α = 0.05 level are in bold.
BMIp, BMI percentile; SE, standard error.
Results of LMM examining the association between total cumulative risk score at year 1 and 3 (categorized as none, 1, 2–3, and ≥4 factors) and BMIp showed that girls experiencing four social factors had statistically significant lower growth rate of BMIp across three waves [β1 = −1.77 (95% confidence interval, CI: −3.39 to −0.15)] compared to girls experiencing no social factors (Table 2). The BMIp trajectories among boys were relatively close and were not statistically significantly different.
Table 2.
Linear Mixed Model of BMI Percentile over Age 3, 5, and 9 Years, According to Sum of Social Risk Score at Age 1 and 3 Years
| Total sample (%) | Initial BMIpa (β0j) (95% CI)c | Growth in BMIpb (β1j) (95% CI)c | |
|---|---|---|---|
| Girls (n = 1825) | |||
| Cumulative social risk | |||
| Cumulative social risk (0) | 420 (23.04) | Ref. | Ref. |
| Cumulative social risk (1) | 560 (30.67) | −0.12 (−3.99 to 3.75) | −0.34 (−1.84 to 1.16) |
| Cumulative social risk (2–3) | 574 (31.45) | −0.16 (−4.03 to 3.70) | 0.30 (−1.06 to 1.67) |
| Cumulative social risk (≥4) | 271 (14.84) | 0.77 (−3.67 to 5.21) | −1.77 (−3.39 to −0.15) |
| Boys (n = 1984) | |||
| Cumulative social risk | |||
| Cumulative social risk (0) | 436 (21.98) | Ref. | Ref. |
| Cumulative social risk (1) | 588 (29.65) | 0.45 (−2.71 to 3.60) | −0.25 (−1.43 to 0.92) |
| Cumulative social risk (2–3) | 650 (32.75) | 0.12 (−3.51 to 3.75) | −0.86 (−2.09 to 0.37) |
| Cumulative social risk (≥4) | 310 (15.63) | −1.17 (−6.30 to 3.96) | −0.79 (−2.55 to 0.97) |
The statistically significant results at an α = 0.05 level are in bold.
BMIp at age 3 years.
In the unit of 2 years.
Adjusted for race/ethnicity, maternal education, maternal marital status, receipt of public assistance, low birth weight, maternal BMI.
CI, confidence interval.
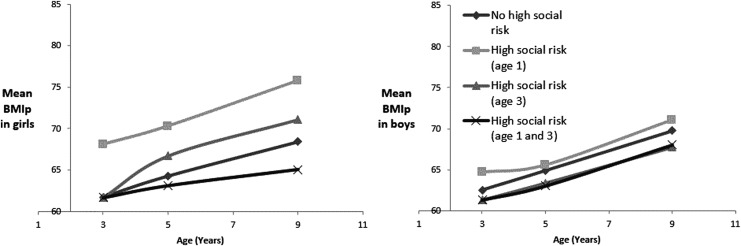
In unadjusted analyses, girls experiencing high cumulative risk at both ages 1 and 3 had consistently lower BMIp; girls experiencing high cumulative risk at only age 1 had higher initial BMIp that remained high (Fig. 1). We noted no differences in BMIp trajectories by cumulative social risk for boys. Similar associations were noted in adjusted analyses; girls experiencing high cumulative risk (≥2 factors) at age 1 or 3 only had higher initial BMIp [β0 = 5.70 (95% CI: 0.15–11.26) and 1.37 (95% CI: −2.25 to 4.99), respectively], and girls experiencing high social risk at age 1 or 3 only had nonsignificantly greater growth rate of BMIp [β1 = 0.39 (95% CI: −0.86 to 1.63) and 0.32 (95% CI: −0.86 to 1.63)], compared with girls experiencing low social risk at either age, compared to those experiencing high cumulative risk at neither age 1 nor 3 (Table 3). No significant associations were found among boys.
Figure 1.
Unadjusted mean BMI percentile at age 3, 5, and 9 years, by high cumulative social risk at age 1 and 3 years among girls.
Table 3.
Linear Mixed Model of BMI Percentile over Age 3, 5, and 9 Years, According to High Cumulative Social Risk (≥2 Social Factors) at Age 1 and/or 3 Years
| Total sample (%) | Initial BMIpa (β0j) (95% CI)c | Growth in BMIpb (β1j) (95% CI)c | |
|---|---|---|---|
| Girls (n = 1825) | |||
| High cumulative social risk (≥2) | |||
| Both age 1 and 3 years | 173 (9.49) | 0.89 (−3.71 to 5.48) | −1.24 (−2.93 to 0.46) |
| Age 3 years only | 377 (20.65) | 1.37 (−2.25 to 4.99) | 0.39 (−0.86 to 1.63) |
| Age 1 year only | 123 (6.73) | 5.70 (0.15–11.26) | 0.32 (−1.57 to 2.22) |
| Neither age 1 nor 3 years | 1152 (63.13) | Ref. | Ref. |
| Boys (n = 1984) | |||
| High cumulative social risk (≥2) | |||
| Both age 1 and 3 years | 195 (9.84) | −1.11 (−5.71 to 3.50) | −0.17 (−1.81 to 1.47) |
| Age 3 years only | 479 (24.13) | −1.20 (−5.48 to 3.09) | −0.50 (−1.91 to 0.92) |
| Age 1 year only | 111 (5.61) | 1.33 (−4.96 to 7.61) | −0.30 (−2.57 to 1.97) |
| Neither age 1 nor 3 years | 1199 (60.41) | Ref. | Ref. |
The statistically significant results at an α = 0.05 level are in bold.
BMIp at age 3 years.
In the unit of 2 years.
Adjusted for sex, race/ethnicity, maternal education, maternal marital status, receipt of public assistance, low birth weight, maternal BMI.
Discussion
In this longitudinal analysis of cumulative social stressors on BMIp, we note a significant association between timing of cumulative stress and BMIp, as well as an association between chronicity of cumulative stress and growth of BMIp that is differential by sex.
In these analyses we note that girls experiencing high cumulative social stress at age 1 or 3 only had relatively higher initial BMIp at age 3 and more rapid increase in BMIp through age 9, respectively, compared to girls experiencing low or no social stressor. These findings are consistent with other studies which have shown an association between psychological and social stressors and childhood obesity and with our previous analyses showing that exposure to high number of social stressors is associated with obesity among girls at age 5.12 However, when examining chronicity, the mean BMIp of girls experiencing high cumulative social stress at both ages 1 and 3 was similar to that of girls experiencing none or a low number of stressors. Analyses of high cumulative social risk (≥4 factors) irrespective of timing of exposure showed a significant slower growth rate of BMIp compared to girls not exposed. It is possible that chronic exposure to high cumulative social stress in early childhood has a differential effect on BMIp. While much of the literature has focused on the obesogenic effects of stress, for some, stress causes a decrease in appetite resulting in potential weight loss and a lower risk of obesity development.40–43 In a recent cross-sectional study of a nationally representative sample of young adults, we note that perceived stress is associated with lower BMI and lower waist circumference among men.44 Stress can suppress or alter appetite hormones; furthermore, in animal studies the stress-eating response is altered by the type of food available.45–47 Alternatively, the lack of an association among this group could be due to the categorization of social stressors which does not account for the severity of the individual stressors and weighs each stressor equally (e.g., IPV is weighted the same as parental incarceration) which could potentially obscure association.
We also note no significant differences in BMIp trajectories among boys, which is consistent with the result of previous studies noting more influences of social environment among girls.12,48 Traditionally, sex differential results among young children may be explained by the prevalent hypothesis of differential sex-specific coping strategies, as females are found to be more likely to turn to consumption of high-density foods or more sedentary lifestyles compared to males in response to stress.14,49,50 However, the role of sex is still not well examined in susceptibility to early-onset obesity. Future studies may examine potential mediation or interaction effect of prenatal factors and parenting behaviors (such as maternal diet and metabolic disorders) linked to fat accumulation on child obesity, to further explain sex differences in obesity development in early childhood in response to stress.49–51 For example, studies have shown that maternal exposure to stress during pregnancy is associated with a series of sex-specific neurodevelopmental changes, as well as stress-specific epigenetic programming and consequently weight in a sex-specific manner, such as sex-specific expression of obesity-related genes (e.g., 44 of the loci), genes specifically expressed on the X chromosome, and sex-specific sensitivities to metabolic hormones.52–54 Particularly, females seem more susceptible to early-life programming in utero and during neonatal period and therefore development of metabolic disease such as obesity, according to a recent review.53
Moreover, the different patterns of BMIp increase between girls experiencing high social risk at age 1 only vs. 3 only suggest that timing of exposure of cumulative social risk matters for increase in BMIp, implying different mechanisms of weight gain and obesity development by age that may require tailored interventions.4 For example, the association between high social risk at age 1 and higher initial BMIp might be attributable to prenatal factors such as maternal lifestyle and weight. Prenatal exposures have been associated with obesity in infants and adolescents.11,55 In contrast, the association between high social risk at age 3 and more rapid growth of BMIp might be attributable to either postnatal factors or environmental factors such as lifestyle and diet of children. Given that behaviors and/or physiology are more modifiable and norms developed early often lay the foundation for future trajectories of health,28 future studies should examine differential mechanisms of stress-related obesity development at different ages which could inform intervention.
Our findings make several contributions to the literature. First, most of the previous studies sought to examine associations between early social adversity and BMIp in later childhood or adolescence, while our study examined the association between early social risk and earlier onset BMIp increase. Second, while our previous study demonstrated that timing matters with regard to association between cumulative social risk and obesity status at age 5, the current study notes that timing of exposure may have a long-term impact on obesity development by affecting BMIp increase in childhood.
However, there are several limitations. First, each social risk factor was considered to have the same association with child BMIp and thus contributed equally to the cumulative social risk score. The cumulative risk index at age 3 further considered child abuse and neglect on the basis of the six risk factors assessed at age 1, due to the fact that child abuse and neglect were not measured at year 3 in FFCWS. Sensitivity analyses were also conducted where child abuse and neglect were removed as risk factors, and no significant differences were noted compared to our previous findings. Second, maternal substance use and food insecurity were assessed based on small number of survey questions rather than standardized instruments, which may cause potential bias. Finally, although this study emphasized the importance of chronicity and timing of cumulative social risk exposure in weight trajectories, we are unable to examine potential mechanisms of the observed association. Despite these limitations, our findings have important implications for early interventions of obesity development, especially among children living in socially disadvantaged contexts. This study further strengthens previous evidence regarding association between social adversity and early-onset obesity by applying a longitudinal design, noting that exposure to high cumulative social adversity in early childhood may have a long-term impact on later obesity development by either increasing the risk of obesity at an earlier age or increasing growth rate of BMIp in childhood.
In summary, we note that girls were at higher risk of higher BMIp in response to social adversity at specific points in time during childhood but of lower BMIp growth in response to cumulative social adversity. Future studies should target the underlying mechanisms of effect of cumulative social risk in different contexts, including sex, timing, and chronicity of exposure, to inform effective intervention design to prevent early-onset obesity.
Supplementary Material
Acknowledgments
Supported by NIH R01HL12765 (S.F.S.). The Fragile Families and Child Wellbeing Study was supported by R01HD36916 from the National Institute of Child Health and Human Development.
Author Disclosure Statement
No competing financial interests exist.
References
- 1. Must A, Spadano J, Coakley EH, et al. . The disease burden associated with overweight and obesity. JAMA 1999;282:1523–1529 [DOI] [PubMed] [Google Scholar]
- 2. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014;311:806–814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Singh GK, Siahpush M, Kogan MD. Rising social inequalities in US childhood obesity, 2003–2007. Ann Epidemiol 2010;20:40–52 [DOI] [PubMed] [Google Scholar]
- 4. Ekelund U, Ong K, Linné Y, et al. . Upward weight percentile crossing in infancy and early childhood independently predicts fat mass in young adults: The Stockholm Weight Development Study (SWEDES). Am J Clin Nutr 2006;83:324–330 [DOI] [PubMed] [Google Scholar]
- 5. Cole TJ. Children grow and horses race: Is the adiposity rebound a critical period for later obesity? BMC Pediatr 2004;4:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Taveras EM, Rifas-Shiman SL, Sherry B, et al. . Crossing growth percentiles in infancy and risk of obesity in childhood. Arch Pediatr Adolesc Med 2011;165:993–998 [DOI] [PubMed] [Google Scholar]
- 7. Rolland-Cachera MF, Deheeger M, Maillot M, Bellisle F. Early adiposity rebound: Causes and consequences for obesity in children and adults. Int J Obes (Lond) 2006;30(Suppl 4):S11–S17 [DOI] [PubMed] [Google Scholar]
- 8. Wickrama KK, O'Neal CW, Lee TK. Early community context, genes, and youth body mass index trajectories: An investigation of gene-community interplay over early life course. J Adolesc Health 2013;53:328–334 [DOI] [PubMed] [Google Scholar]
- 9. Cecil-Karb R, Grogan-Kaylor A. Childhood body mass index in community context: Neighborhood safety, television viewing, and growth trajectories of BMI. Health Soc Work 2009;34:169–177 [DOI] [PubMed] [Google Scholar]
- 10. Wells NM, Evans GW, Beavis A, Ong AD. Early childhood poverty, cumulative risk exposure, and body mass index trajectories through young adulthood. Am J Public Health 2010;100:2507–2512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Huang DY, Lanza HI, Anglin MD. Trajectory of adolescent obesity: Exploring the impact of prenatal to childhood experiences. J Child Fam Stud 2014;23:1090–1101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Suglia SF, Duarte CS, Chambers EC, Boynton-Jarrett R. Cumulative social risk and obesity in early childhood. Pediatrics 2012;129:e1173–e1179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Elovainio M, Pulkki-Råback L, Hakulinen C, et al. . Psychosocial environment in childhood and body mass index growth over 32 years. Prev Med 2017;97:50–55 [DOI] [PubMed] [Google Scholar]
- 14. Torres SJ, Nowson CA. Relationship between stress, eating behavior, and obesity. Nutrition 2007;23:887–894 [DOI] [PubMed] [Google Scholar]
- 15. Dallman MF. Stress-induced obesity and the emotional nervous system. Trends Endocrinol Metab 2010;21:159–165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Adam TC, Epel ES. Stress, eating and the reward system. Physiol Behav 2007;91:449–458 [DOI] [PubMed] [Google Scholar]
- 17. Boynton-Jarrett R, Fargnoli J, Suglia SF, et al. . Association between maternal intimate partner violence and incident obesity in preschool-aged children: Results from the fragile families and child well-being Study. Arch Pediatr Adolesc Med 2010;164:540–546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Taylor CA, Guterman NB, Lee SJ, Rathouz PJ. Intimate partner violence, maternal stress, nativity, and risk for maternal maltreatment of young children. Am J Public Health 2009;99:175–183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lissau I, Sørensen TI. Parental neglect during childhood and increased risk of obesity in young adulthood. Lancet 1994;343:324–327 [DOI] [PubMed] [Google Scholar]
- 20. Garasky S, Stewart SD, Gundersen C, et al. . Family stressors and child obesity. Soc Sci Res 2009;38:755–766 [DOI] [PubMed] [Google Scholar]
- 21. Lohman BJ, Stewart S, Gundersen C, et al. . Adolescent overweight and obesity: Links to food insecurity and individual, maternal, and family stressors. J Adolesc Health 2009;45:230–237 [DOI] [PubMed] [Google Scholar]
- 22. Kursmark M, Weitzman M. Recent findings concerning childhood food insecurity. Curr Opin Clin Nutr Metab Care 2009;12:310–316 [DOI] [PubMed] [Google Scholar]
- 23. Sarlio-Lähteenkorva S, Lahelma E. Food insecurity is associated with past and present economic disadvantage and body mass index. J Nutr 2001;131:2880–2884 [DOI] [PubMed] [Google Scholar]
- 24. Kral TV, Chittams J, Moore RH. Relationship between food insecurity, child weight status, and parent-reported child eating and snacking behaviors. J Spec Pediatr Nurs 2017;22:e12177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Elsenburg LK, van Wijk KJE, Liefbroer AC, Smidt N. Accumulation of adverse childhood events and overweight in children: A systematic review and meta-analysis. Obesity (Silver Spring) 2017;25:820–832 [DOI] [PubMed] [Google Scholar]
- 26. Ekelund U, Ong K, Linné Y, et al. . Upward weight percentile crossing in infancy and early childhood independently predicts fat mass in young adults: The Stockholm Weight Development Study (SWEDES). Am J Clin Nutr 2006;83:324–330 [DOI] [PubMed] [Google Scholar]
- 27. Lawlor DA, Chaturvedi N. Treatment and prevention of obesity—are there critical periods for intervention? Int J Epidemiol 2006;35:3–9 [DOI] [PubMed] [Google Scholar]
- 28. Ben-Shlomo Y, Kuh D. A life course approach to chronic disease epidemiology: Conceptual models, empirical challenges and interdisciplinary perspectives. Int J Epidemiol 2002;31:285–293 [PubMed] [Google Scholar]
- 29. Reichman NE, Teitler JO, Garfinkel I, McLanahan SS. Fragile families: Sample and design. Child Youth Serv Rev 2001;23:303–326 [Google Scholar]
- 30. Herriot RA, Kasprzyk D. Survey of Income and Program Participation. 1984 [Google Scholar]
- 31. Meyers MK, Garfinkel I. Social indicators and the study of inequality. Econ Policy Rev 1999;5 [Google Scholar]
- 32. Lloyd S. The effects of domestic violence on women's employment. Law Policy 1997;19:139–167 [Google Scholar]
- 33. Sweet JA, Bumpass LL, Call V. The Design and Content of the National Survey of Families and Households. University of Wisconsin, Center for Demography and Ecology Madison, 1988 [Google Scholar]
- 34. Kessler RC, Andrews G, Mroczek D, et al. . The World Health Organization composite international diagnostic interview short‐form (CIDI‐SF). Int J Methods Psychiatr Res 1998;7:171–185 [Google Scholar]
- 35. Kessler RC, Wittchen HU, Abelson JM, et al. . Methodological studies of the Composite International Diagnostic Interview (CIDI) in the US national comorbidity survey (NCS) 1998;7:33–55 [Google Scholar]
- 36. Straus MA, Hamby SL, Finkelhor D, et al. . Identification of child maltreatment with the Parent–Child Conflict Tactics Scales: Development and psychometric data for a national sample of American parents. Child Abuse Negl 1998;22:249–270 [DOI] [PubMed] [Google Scholar]
- 37. Singer JD. Using SAS PROC MIXED to fit multilevel models, hierarchical models, and individual growth models. J Educ Behav Stat 1998;23:323–355 [Google Scholar]
- 38. Allison PD. Missing Data, vol. 136 Sage Publications, 2001 [Google Scholar]
- 39. Rubin DB, Schenker N. Multiple imputation in health-care databases: An overview and some applications. Stat Med 1991;10:585–598 [DOI] [PubMed] [Google Scholar]
- 40. Kivimäki M, Head J, Ferrie JE, et al. . Work stress, weight gain and weight loss: Evidence for bidirectional effects of job strain on body mass index in the Whitehall II study. Int J Obes (Lond) 2006;30:982–987 [DOI] [PubMed] [Google Scholar]
- 41. Chen Y, Qian L. Association between lifetime stress and obesity in Canadians. Prev Med 2012;55:464–467 [DOI] [PubMed] [Google Scholar]
- 42. Kuo LE, Czarnecka M, Kitlinska JB, et al. . Chronic stress, combined with a high-fat/high-sugar diet, shifts sympathetic signaling toward neuropeptide Y and leads to obesity and the metabolic syndrome. Ann N Y Acad Sci 2008;1148:232–237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Dallman MF, Akana SF, Laugero KD, et al. . A spoonful of sugar: Feedback signals of energy stores and corticosterone regulate responses to chronic stress. Physiol Behav 2003;79:3–12 [DOI] [PubMed] [Google Scholar]
- 44. Suglia SF, Pamplin JR, Forde AT, Shelton RC. Sex differences in the association between perceived stress and adiposity in a nationally representative sample. Ann Epidemiol 2017;27:626–631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Diane A, Victoriano M, Fromentin G, et al. . Acute stress modifies food choice in Wistar male and female rats. Appetite 2008;50:397–407 [DOI] [PubMed] [Google Scholar]
- 46. Yau YH, Potenza MN. Stress and eating behaviors. Minerva Endocrinol 2013;38:255–267 [PMC free article] [PubMed] [Google Scholar]
- 47. Zeeni N, Daher C, Fromentin G, et al. . A cafeteria diet modifies the response to chronic variable stress in rats. Stress 2013;16:211–219 [DOI] [PubMed] [Google Scholar]
- 48. Singh GK, Siahpush M, Kogan MD. Neighborhood socioeconomic conditions, built environments, and childhood obesity. Health Aff (Millwood) 2010;29:503–512 [DOI] [PubMed] [Google Scholar]
- 49. Shimanoe C, Hara M, Nishida Y, et al. . Perceived stress and coping strategies in relation to body mass index: Cross-sectional study of 12,045 Japanese men and women. PLoS One 2015;10:e0118105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Nicdao EG, Hong S, Takeuchi DT. Prevalence and correlates of eating disorders among Asian Americans: Results from the National Latino and Asian American Study. Int J Eat Disord 2007;40(Suppl):S22–S26 [DOI] [PubMed] [Google Scholar]
- 51. Bale TL, Baram TZ, Brown AS, et al. . Early life programming and neurodevelopmental disorders. Biol Psychiatry 2010;68:314–319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Schulz KM, Pearson JN, Neeley EW, et al. . Maternal stress during pregnancy causes sex-specific alterations in offspring memory performance, social interactions, indices of anxiety, and body mass. Physiol Behav 2011;104:340–347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Dearden L, Bouret SG, Ozanne SE. Sex and gender differences in developmental programming of metabolism. Mol Metab 2018;15:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Bronson SL, Chan JC, Bale TL. Sex-specific neurodevelopmental programming by placental insulin receptors on stress reactivity and sensorimotor gating. Biol Psychiatry 2017;82:127–138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Patel N, Godfrey KM, Pasupathy D, et al. . Infant adiposity following a randomised controlled trial of a behavioural intervention in obese pregnancy. Int J Obes 2017;41:1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Blissett J, Haycraft E, Farrow C. Inducing preschool children's emotional eating: Relations with parental feeding practices. Am J Clin Nutr 2010;92:359–365 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.