Abstract
Osteochondroma (osteocartilaginous exostosis) is one of the most common benign tumors of bone but is rare in the craniofacial region. Only a few cases of osteochondroma of the coronoid process have been reported in the literature, since the time of its discovery (osteochondroma of a coronoid process) by Jacob in 1899. We present a case of osteochondroma of the left coronoid process in a 16-year-old female patient. Contrary to the literature, our patient had no limited mouth opening despite a close approximation of left hyperplastic coronoid process with zygomatic arch, making it a unique case among similar cases. Plain radiography can be used for this hyperplastic condition but due to its inherent distortion and being only two-dimensional (2D) it has a limited diagnostic advantage. Cone beam computed tomography (CBCT) was employed for necessary diagnostic information. We managed our patient with an intraoral coronoidectomy.
Keywords: Osteochondroma , Coronoid process , Cone beam computed tomography
Introduction
Osteochondroma is one of the most common benign tumors of the skeleton. It has a typical cartilage-capped hyperplastic growth, which is usually mushroom shaped and is a common tumor in the axial skeleton, usually in the metaphysis of long bones like femur and tibia.[1] It is normally seen in the bones that develop through endochondral ossification,[2] the fact that shows its frequency in the designated areas. Most maxillofacial bones go through a developmental process of intramembranous ossification and thus a rare site for the occurrence of osteochondroma, although it can occur in mandibular condyle or coronoid process,[1] and only a handful of cases have been reported in the literature affecting the latter two sites.
Von langenback in 1853 defined hyperplasia of the coronoid process of the mandible for the first time, but a fusion of hyperplastic coronoid process with zygomatic bone, a case of osteochondroma was first reported by French Anatomist, Oscar Jacob in 1899.[3] Jacob described a pseudo arthrosis joint between the coronoid process of the mandible and medial aspect of zygomatic bone, a case of osteochondroma and hence the condition has retained the eponym of Jacob’s disease.[4] The osteochondroma of coronoid process develops slowly with major presenting signs of a painless decreased mouth opening and changes in the morphology of zygomatic bone.[5] Panoramic radiography being very useful to the dentist, a simple and cheap investigation for the patients, allows a good outline of jaws and adjacent tissue, could be used for investigation of morphological changes in coronoid process,[6] although the interpretation can prove a difficult task owing to the superimposition of various structures in the region of posterior maxilla. Cone beam computed tomography (CBCT) being affordable, having less radiation and same diagnostic benefit when compared to multidetector computed tomography (MDCT), was used for diagnosis and surgical planning in this case. Intraoral Coronoidectomy was used for the resection of the tumor mass in our patient.
Case Report
A 16-year-old female patient reported to our department, Oral Medicine and Radiology with a chief complaint of swelling on the left side of the face. The patient’s medical anamnesis was non-contributory. There was no history of any trauma, congenital bone disorder and there was no defect in any other musculoskeletal system. Clinical examination revealed a diffuse swelling of around 3 centimetres (cm) by 3 centimetres (cm) in the region of left zygoma in closed mouth position (Figure 1A). The swelling exaggerated upon opening of the mouth (Figure 1B) and reached back to its original size in closed mouth position. There was no pain or deviation during opening and closing of mouth and the interincisal distance was 43 mm in maximum opening position. Audible click was felt over the left temporomandibular joint region and increased pressure was detected over left zygoma during the opening of the mouth. Intraoral examination revealed good oral hygiene with no significant findings (Figure 1C and 1D).
Figure1.

A: Swelling over left zygoma in closed mouth position, B: Marked facial asymmetry due to outward movement of zygoma in open mouth position, C: Upper dental arch with no significant findings, D: Lower dental arch with signs of good oral hygiene
Panoramic radiograph showed increased radiopacity with an altered morphology of the left coronoid process as compared to right side (Figure 2). As panoramic radiograph lacked clarity and did not reveal the exact extension and shape of the hyperplastic left coronoid process, a CBCT scan was used for descriptive diagnosis. After taking informed consent for exposure, the patient was scanned using CBCT Planmeca Promax 3D Mid (Planmeca Finland) machine at 90kVp, 8mA, 13.772 seconds’ scan time, 20.2cm height and 17.5cm diameter scan volume. Planmeca Romexis viewer software 4.3.0.R was employed for generation of volumetric and study data. The images obtained from CBCT were reconstructed in multiplanar image mode. Axial section of CBCT showed a close approximation of enlarged coronoid process with medial aspect of zygomatic arch on the left side (Figure 3A). Zygomatic arch has remodelled itself in Figure 3A to a position more outward as compared to the unaffected right side, and this remodelling has given rise to facial asymmetry in the form of swelling over the zygoma region clinically. CBCT coronal section revealed the enlarged coronoid process just short of impinging with medial surface of zygomatic arch on the left side (Figure 3B). Outward pushing of zygomatic bone on the left side as compared to that of right can be appreciated in this section as well. CBCT sagittal section of the left coronoid process clearly showed abnormal enlargement and extension of the left coronoid process in an anterior direction (Figure 3C). Three-dimensional (3D) reconstruction showed distinct bone like mass on left coronoid process (Figure 4A and C) and a normal morphology of right coronoid process (Figure 4B).
Figure2.

Panoramic radiograph revealing a change in the morphology of left coronoid process
Figure3.

a: CBCT axial section reveals bony enlargement continuous with the tip of the left coronoid process. b: CBCT coronal section showing extension of left coronoid mass in the inner surface of zygomatic arch. c: Sagittal section of CBCT showing exophytic growth of left coronoid process
Figure4.

A: 3D CBCT reconstruction shows enlarged left coronoid process projecting high up, impinging on inner surface of zygomatic arch. B: 3D sagittal reconstruction reveals normal right coronoid process, C: 3D sagittal reconstruction reveals distinct bone like mass approximating on inner surface of zygomatic arch on left side
A provisional diagnosis of the osteochondroma of left coronoid process was given, and the patient was planned for surgical excision of the tumor mass (Figure 5A). Intra-oral coronoidectomy of the left side was carried out (Figures 5B, C and D). The resected specimen (Figure 5E) approximately 3.0X1.0 centimetres in size was sent for histopathological examination. The specimen after decalcification showed zones of fibrous tissue, proliferating chondrocytes, and hyperplastic chondroblasts (Figure 6) suggestive of osteochondroma. The patient is under follow up and showed uneventful recovery after 6 months follow up (Figure 7A and B). The post-operative CBCT images and 3D reconstruction shows successful resection of the left coronoid process (Figure 8 and Figure 9).
Figure5.
A: Patient prepared for surgical procedure, B: Intraoperative procedure of resection of bony enlargement of left coronoid process, C: Post resection picture of surgical site, D: Closure of surgical site using 3-0 Vicryl sutures, E: The gross surgical specimen around 3.0 X 1.0 cms, which was white in colour, smooth surfaced and hard in consistency
Figure6.
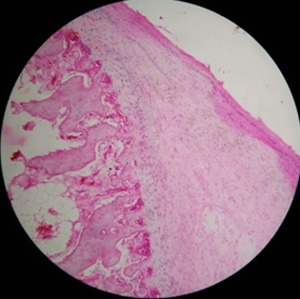
Histopathological examination confirmed osteochondroma. The tumor consists of zones of fibrous tissue, proliferating chondrocytes, hyperplastic chondroblasts, and endochondral ossification underneath the cartilage
Figure7.

A: Post-operative picture in closed mouth position showing improvement in left zygomatic arch expansion. B: Post-operative picture in open mouth position showing symmetrical facial appearance
Figure8.

A: Post-operative CBCT axial section showing no more extension of left coronoid process, B: Post-operative CBCT coronal section shows absence of exophytic growth on the inner side of left zygomatic arch, C: Post-operative CBCT sagittal section reveals successful resection of tumour mass on left coronoid process
Figure9.

A: Post-operative 3D CBCT reconstruction shows successful resection of left enlarged coronoid process, B: 3D sagittal reconstruction reveals normal right coronoid process, C: Post-operative 3D CBCT sagittal reconstruction shows reduced height of left coronoid process after successful resection of tumour mass
Discussion
Osteochondroma, an osteocartilaginous exostosis, one of the most common skeletal tumors occurs as a nonhereditary, solitary lesion in 85% of cases.[7] It constitutes about 35.5% and 8.5% of benign bone tumors and all bone tumors overall respectively and when it occurs in the coronoid process has a slight predilection for males, and favouring left coronoid process.[8] It can occur in the form of multiple lesions when it is known as multiple hereditary exostosis and inherited as an autosomal dominant pattern.[9] Solitary osteochondroma is usually seen in the axial and appendicular skeleton. In rare instances, it may occur at the base of the skull, maxillary sinus, mandible, and zygomatic arch when affecting the craniofacial region.[7] The tumor is comparatively rare all over the body, more so in the head and neck region, specifically on the mandibular coronoid process.[1] Osteochondroma of the coronoid process of the mandible was first reported by Oscar Jacob in 1899. It can occur unilaterally or bilaterally, with a mean age at the time of diagnosis shown as 30 years (age range: 3-73years), and further investigations have shown a propensity of 77% in the age range of 10-40 years, falling in the increased risk category.[7] The condition is asymptomatic in the earlier stages, often with a complaint of progressively decreasing mouth opening over an extended period followed by pressure in the region of attachment of coronoid process to the medial surface of the zygomatic arch and often with a deviated opening path of the mandible to the affected side.[1] The various etiological factors that have been put forward for osteochondroma of coronoid process range from high temporomandibular joint activity, trauma, familial and genetic predisposition.[4] The patient in this case report had no complaint of any pain supporting the literature but had no compromised mouth opening that is contrary to the existing literature. Our patient had an unobstructed mouth opening measuring 43mm. The zygomatic arch has remodelled itself in this case extensively to make room for anteriorly ex tending hyperplastic coronoid process. Due to the lack of constant contact between the two implicated surfaces (enlarged coronoid process and the inner surface of zygomatic arch) our patient had no restricted mouth opening.
The panoramic radiographs if used alone can lead to difficulty in diagnosing the morphological changes in the region of the coronoid process and zygomatic arch and 3D imaging modalities like computed tomography (CT) can be used as an alternative investigation, providing the exact shape of an enlarged coronoid process and adjoining displaced bones.[10] 3D imaging can be an invaluable tool for devising a proper treatment plan, but can expose patients to high radiation dose and should be used with caution, particularly in young patients. Its use should be restricted to patients, who have huge morphological alterations, which are not discernible by other means of investigations with less radiation exposure.[11] Osteochondroma of coronoid is usually noticed initially during routine radiographic investigations or palpation of the affected area and to confirm doubts, CT with 3D reconstruction is recommended.[1] In the recent times, owing to less radiation exposure and cost efficiency of CBCT, it has been favoured for diagnosis in comparison with CT.[12] CBCT owing to its less radiation dosage has replaced multidetector CT for image acquisition in craniofacial radiology and can be used as a routine imaging modality.[10] Although we could infer increased radio-opacity over the left coronoid process on panoramic radiograph in our patient, suggesting of abnormal morphology yet it was not clear to assess the exact morphological extension of the bone, so we felt the need for further imaging to arise at a convincing diagnosis. CBCT being economical, less time consuming and on a par with CT for such cases, was used in present case. Utilizing multiplanar imaging and a detailed study of coronal, sagittal, and axial sections led us to the provisional diagnosis of osteochondroma of left coronoid process, which was later confirmed by the histopathological report. Histopathological differential diagnosis of osteochondroma includes benign osteoblastoma, osteoma, chondroblastoma, chondroma, and bony hyperplasia.[13]
The literature shows a variable number of surgical approaches for the resection of the osteochondroma of the coronoid process, employing both intraoral as well as extraoral techniques.[5,14-15] CBCT provided us with an estimate of the size of the lesion that was suitable for an intra oral approach. The patient’s normal mouth opening also helped us to approach the lesion intraorally and this way the excessive amounts of scaring and a risk to neighbouring neurovascular structures that may be associated with any extraoral approach was avoided. The recurrence rate after complete resection of osteochondroma of coronoid process is rare around 2%.[16] The patient is on regular follow-up and showed no signs of any abnormality at one year of a follow-up appointment.
Conclusion
Osteochondroma of coronoid process of mandible consists of a pseudo-joint between hyperplastic coronoid process and the inner surface of the zygomatic bone. Osteochondroma should be considered when patients present with progressively limited mouth opening with facial asymmetry. A rare case of osteochondroma is presented with no limitation in mouth opening. Pre-operative cone beam computed tomography (CBCT) helped us with the diagnosis of this case, although the final diagnosis was made only after histopathological investigation. CBCT can be an indispensable radiographic investigation when designing surgery for such cases. We recommend an intra-oral approach for the resection of osteochondroma of coronoid process.
Footnotes
Conflict of Interest: The authors disclose no potential conflicts of interest.
References
- 1.Stringer DE, Chatelain KB, Tandon R. Surgical Treatment of Jacob's Disease: A Case Report Involving an Osteochondromaof the Coronoid Process. Case Rep Surg. 2013; 2013: 253740. doi: 10.1155/2013/253740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tucker MR, Guilford WB, Howard CW. Coronoid process hyperplasia causing restricted opening and facial asymmetry. Oral Surg Oral Med Oral Pathol. 1984; 58: 130–132. doi: 10.1016/0030-4220(84)90124-5. [DOI] [PubMed] [Google Scholar]
- 3.Reddy NV, Rajan R, Rachalapally VK, Kallam SR. Jacob's disease: A rare case report. J NTR Univ Health Sci. 2014; 3: 202–205. [Google Scholar]
- 4.Aoki N, Okamura K, Niino D, Iwamoto O, Kusukawa J. Osteochondroma of the right coronoid process (Jacob disease): a case report. Cranio. 2013; 31: 66–69. doi: 10.1179/crn.2013.010. [DOI] [PubMed] [Google Scholar]
- 5.Roychoudhury A, Gupta YK, Parkash H, Karak AK. Jacob disease: report of a case and review of the literature. J Oral Maxillofac Surg. 2002; 60: 699–703. doi: 10.1053/joms.2002.33125. [DOI] [PubMed] [Google Scholar]
- 6.Gross M, Gavish A, Calderon S, Gazit The coronoid process as a cause of mandibular hypomobility--case reports. J Oral Rehabil. 1997; 24: 776–781. doi: 10.1046/j.1365-2842.1997.00556.x. [DOI] [PubMed] [Google Scholar]
- 7.Fan H, Lv X, Shi J, Hu J, Luo E. One-stage treatment to osteochondroma of the coronoid process and secondary facialasymmetry with coronoidectomy and reduction malarplasty: a case report and literature review. J Oral Maxillofac Surg. 2014; 72: 1870.e1–1870. doi: 10.1016/j.joms.2014.04.030. [DOI] [PubMed] [Google Scholar]
- 8.Ajila V, Hegde S, Gopakumar R, Babu GS. Imaging and histopathological features of Jacob's disease: a case study. Head Neck Pathol. 2012; 6: 51–53. doi: 10.1007/s12105-011-0324-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kitsoulis P, Galani V, Stefanaki K, Paraskevas G, Karatzias G, Agnantis NJ, et al. Osteochondromas: review of the clinical, radiological and pathological features. In Vivo. 2008; 22: 633–646. [PubMed] [Google Scholar]
- 10.Sawada K, Schulze D, Matsumoto K, Hirai S, Hashimoto K, Honda K. Osteochondroma of the coronoid process of the mandible. J Oral Sci. 2015; 57: 389–392. doi: 10.2334/josnusd.57.389. [DOI] [PubMed] [Google Scholar]
- 11.Costa YM, Porporatti AL, Stuginski-Barbosa J, Cassano DS, Bonjardim LR, Conti PC. Coronoid process hyperplasia: an unusual cause of mandibular hypomobility. Braz Dent J. 2012; 23: 252–255. doi: 10.1590/s0103-64402012000300012. [DOI] [PubMed] [Google Scholar]
- 12.Kim SM, Lee JH, Kim HJ, Huh JK. Mouth opening limitation caused by coronoid hyperplasia: a report of four cases. J Korean Assoc Oral Maxillofac Surg. 2014; 40: 301–307. doi: 10.5125/jkaoms.2014.40.6.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dandriyal R, Giri KY, Pant S, Alam S, Joshi A. Giant osteochondroma of the coronoid process. J Maxillofac Oral Surg. 2015; 14(Suppl 1): 412–416. doi: 10.1007/s12663-014-0650-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kerscher A, Piette E, Tideman H, Wu PC. Osteochondroma of the coronoid process of the mandible. Report of a case and review of the literature. Oral Surg Oral Med Oral Pathol 1993; 75: 559–564. doi: 10.1016/0030-4220(93)90224-r. [DOI] [PubMed] [Google Scholar]
- 15.Escuder i de la Torre O, Vert Klok E, Marí i Roig A, Mommaerts MY, Pericot i Ayats J. Jacob's disease: report of two cases and review of the literature. J Craniomaxillofac Surg. 2001; 29: 372–376. doi: 10.1054/jcms.2001.0247. [DOI] [PubMed] [Google Scholar]
- 16.Losa-Munoz PM, Burgueno-Garcia M, Gonzalez-Martin-Moro J, Sanchez-Burgos R. Osteochondroma of coronoid process: a rare etiology of jacob disease. Craniomaxillofac Trauma Reconstr. 2014; 7: 306–309. doi: 10.1055/s-0034-1378182. [DOI] [PMC free article] [PubMed] [Google Scholar]



