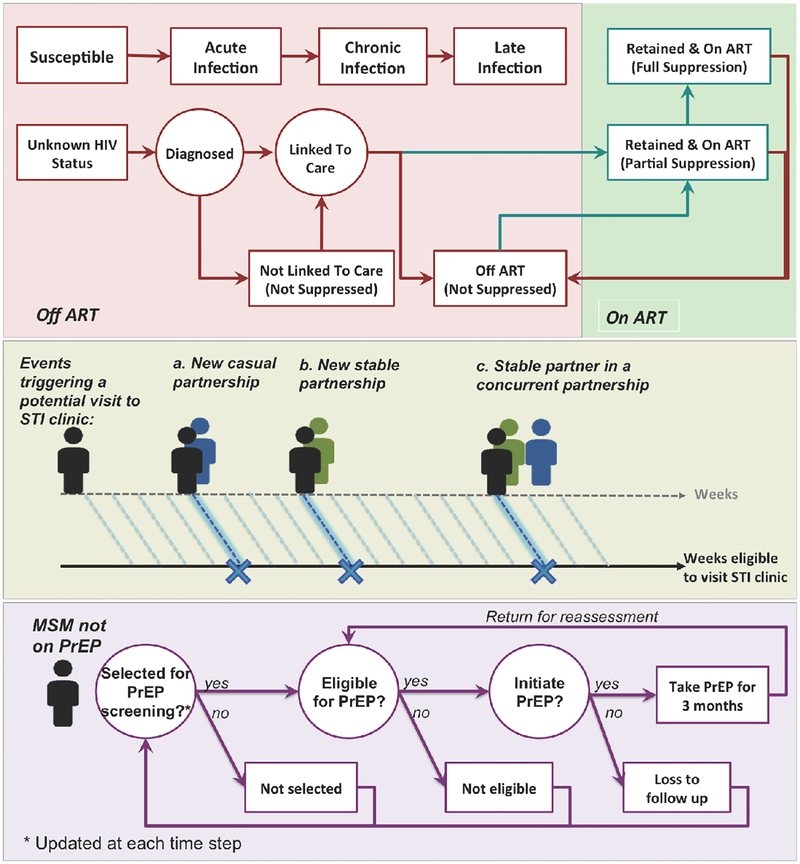
Figure 1: Simulation overview.
This figure illustrates the schematic simulation logic for modeling HIV natural history and the cascade of care (top panel), individuals’ presentation to STI clinics (middle panel) and PrEP procedure (bottom panel). Top Panel: HIV natural history is modeled through 3 main disease states associated with an increase in viral load (with parameters given in Table 1). The cascade of care – also evaluated on a weekly basis – represents processes of diagnosis, linkage to care, ART initiation, and retention in care. Middle panel: “Eligibility” for presenting to an STI clinic is evaluated at the end of each week: individuals have a defined probability of presenting to an STI clinic during any week in which they start a new partnership or their stable partner starts a concurrent partnership. Bottom panel: MSM are selected for PrEP assessment at the time of attending STI-clinics (strategy 1), or randomly from the community at large (strategy 2). The eligibility criteria for PrEP are set according to CDC guidelines. Eligible MSM who accept PrEP (according to PrEP “uptake”) initiate PrEP immediately and will experience a fixed level of protection against HIV transmission (“adherence”) while on PrEP.