Abstract
We have reported a case of right upper limb injury of shoulder and elbow who was managed with ultrasound-guided interscalene block during surgery and indwelling catheter for postoperative analgesia. He developed weakness in the contralateral upper limb in the postoperative period due to inadvertent spread of local anaesthetic in the cervical epidural space. No serious complication occurred due to timely intervention. The possible pathways of such unwanted epidural spread and methods to reduce such complications have been discussed.
Key words: Brachial plexus, interscalene block, regional anaesthesia, ultrasound-guided blocks
INTRODUCTION
Interscalene block (ISB) is a frequently used regional technique for shoulder surgery, and interscalene catheter helps achieve extended pain relief in the postoperative period. The use of ultrasound for ISB has shown significantly reduced time of onset and total volume of local anaesthetics in comparison to nerve localisation by nerve stimulators.[1] As the injection site of ISB is located in close proximity to the anatomical structures of the spinal canal, spread of local anaesthetics could potentially cause adverse events, including epidural spread, total spinal anaesthesia and death.[2,3,4]
We report a case where inadvertent epidural spread occurred after successful ultrasound-guided ISB receiving postoperative analgesia through interscalene catheter resulting in neurologic symptoms on the contralateral side. A possible pathway of epidural spread of local anaesthetic from the interscalene area is also discussed in this report.
CASE
A 45-year-old male patient, body mass index 27.6 kg/m2, sustained complex injury of the right shoulder, right elbow and contusion of left shoulder after road traffic accident. Preanaesthetic checkup was done; there was no coexisting comorbidity, head injury was ruled out and informed consent was taken. Reconstructive surgery of the right shoulder with elbow fixation was decided. As the surgeon expected a long and complex surgery (>4 h duration), right-sided ISB with catheter was planned. In the operation theatre, after connecting noninvasive monitors (electrocardiography, noninvasive blood pressure and oximeter), right-sided ISB was given using high-frequency ultrasound probe (6–13 MHz; SonoSite® Turbo-M) with an in-plane technique (lateral to medial). After due aseptic precautions and adequate sedation (intravenous fentanyl 50 μg and midazolam 1 mg), ISB was given with 20 mL of 0.75% ropivacaine using 18G Tuohy needle (Contiplex® Tuohy Set; B-Braun Medical Inc., Bethlehem, PA, USA), and a 20G catheter was inserted through Tuohy needle (5 cm beyond the tip and fixed at 7 cm mark at skin) to be used for supplemental intraoperative anaesthesia and postoperative analgesia [Figure 1a and b]. Block effect was excellent, intraoperative sedation was provided by infusion of dexmedetomidine 4–12 μg/h and surgery and anaesthesia were uneventful. The surgery lasted for 256 min, but no intraoperative supplement was required. The patient was shifted to high-dependency unit where continuous monitoring of vitals and pain by numeric rating scale (NRS; 0 = no pain, 10 = severe pain) was done as per standard hospital protocol. In the immediate postoperative period, the patient complained of moderate to severe pain (NRS = 6–7) in the left shoulder (nonoperated side but injured during road traffic accident (RTA) which was treated with paracetamol 1 g + tramadol 50 mg infusion over 15 min. Postoperative analgesia was continued with intravenous injection paracetamol 1 g + tramadol 50 mg 8 hourly and infusion of ropivacaine 0.2% at 4 mL/h through interscalene catheter. The patient had excellent pain relief during rest and during movement (NRS = 3–4/10). After 12 h of local anaesthetic infusion through interscalene catheter, the patient noticed tingling and numbness in the left hand and observed that the pain in the nonoperated shoulder has decreased to a significant level. Thinking this effect to his benefit, he did not notify anyone about this; however, in the next 6 h when numbness was gradually increasing to weakness (inability to hold the glass tightly), he informed. Catheter migration was suspected, infusion was stopped and close observation was done. After 4 h, numbness and weakness disappeared gradually. Consent for fluoroscopy was taken, and the next day, 5 mL of water-soluble nonionic contrast (Omnipaque-300) was injected through catheter under fluoroscopy. Initial injection showed spread of contrast within the brachial plexus sheath (thus catheter migration was ruled out); however, when 10 mL of saline was injected further, spread of contrast to the cervical epidural spacewas noticed [Figure 1c]. The catheter was removed and further postoperative analgesia was managed with intravenous paracetamol (1 g) + tramadol (50 mg) along with diclophenac sodium (75 mg) 8–12 hourly. Further course was uneventful. The patient was discharged after fifth day of surgery with oral analgesics.
Figure 1.
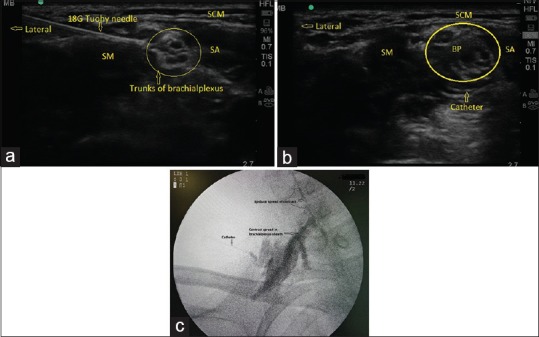
(a) Technique of ISB, 18G Tuohy needle near brachial plexus under high-frequency ultrasound probe and in-plane approach. (b) Catheter is clearly visualised near the lower end of brachial plexus; (c) Contrast spread within the brachial plexus sheath and cervical epidural space (arrows). SA: scalene anterior muscle; SM: scalene medius muscle; BP: brachial plexus; SCM: sternocleidomastoid muscle; SA: scalene anterior muscle; SM: scalene medius muscle
DISCUSSION
In the present case, the local anaesthetic drug inadvertently spread to cervical epidural and resulted in bilateral analgesia and neurologic symptoms in the contralateral limb. Case reports on these complications have been published previously.[5] Although ultrasound provides excellent visualisation of target structures in ISB and therefore enables physicians to place injection needles with enormous accuracy,[6] even then epidural spread can occur. Then the question arises, is there a critical volume for local anaesthetic above which complications such as epidural spread and consequently contralateral blockade results.[7] A recently published study has showed that the phenomenon of epidural spread can be reproduced in cadavers and it was positively correlated to injection volumes exceeding 10 mL.[8] Moreover, a trend toward cranial spread of the contrast agent in all investigated specimens along the course of the nerve roots toward the spinal cord was observed. The volume is not the sole factor, as in another cadaveric study by Orebaugh et al., cranial epidural spread was detectable following injection of dye into the nerve roots of the brachial plexus.[9] The real mechanism of this spread is not known, however; at times the dural sheath may extend along the nerve root(s) and unintended neuraxial spread of local anaesthetic through a dural sleeve may occur and cause a complication after ISB.[3] A recent study has also shown that ISB given outside the sheath of brachial plexus is safer than given inside the sheath.[10] However, this fact is debatable as Krishnan et al. have found no difference when ISB catheter was placed within the plexus and outside of plexus.[11] In our case, both the factors (large volume 20 mL initial volume and injection near the nerve roots) [Figure 1a] are possible causes, however; there was a big time gap for symptoms of epidural spread. We think initial epidural spread (large volume factor) was masked by the long surgery time (256 min) and, due to low-dose infusion, there was a delayed (cumulative) effect on the nerves resulting in sensory and motor blockade.[12] Bilateral block can occur when the catheter inadvertently enters into the cervical extradural space as described in a case report where ISB was performed using landmark-based technique.[13] In our case, this was not a possibility because the tip of the catheter was nicely visualised during block [Figure 1b]. There was no respiratory distress at any point in the present case, perhaps because small volume was infused at a slower rate (4 mL/h) so that drug could diffuse. Such complication can further be minimised by bolus-only administration. In one study, 0.2% ropivacaine bolus-only has provided a similar analgesic effect with a lower total volume of local anaesthetic and decreased motor weakness compared with combined infusion.[14]
To summarise, we report a case of combined shoulder and elbow surgery managed with ISB with catheter and who developed postoperative neurologic symptoms in the contralateral upper limb due to inadvertent spread of local anaesthetic in the epidural space. The possible causes were higher volume of local anaesthetic and proximity of needle and subsequent catheter with the nerve roots. Timely detection of symptoms prevented serious consequences.
CONCLUSION
ISB is effective in providing pain relief after shoulder and elbow surgery. Inadvertent spread of local anaesthetic in the epidural spread can occur and may result in neurological complications. These complications can be prevented by lower doses of anaesthetic drug and keeping needle and catheter tips in a safe distance from nerve roots while performing ISB. Early recognition by continuous monitoring and prompt management is necessary to avoid serious consequences.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Fredrickson MJ, Ball CM, Dalgleish AJ. A prospective randomized comparison of ultrasound guidance versus neurostimulation for interscalene catheter placement. Reg Anesth Pain Med. 2009;34:5904. doi: 10.1097/aap.0b013e3181ada622. [DOI] [PubMed] [Google Scholar]
- 2.Kumar A, Battit GE, Froese AB, Long MC. Bilateral cervical and thoracic epidural blockade complicating interscalene brachial plexus block: Report of two cases. Anesthesiology. 1971;35:6502. doi: 10.1097/00000542-197112000-00022. [DOI] [PubMed] [Google Scholar]
- 3.Passannante AN. Spinal anesthesia and permanent neurologic deficit after interscalene block. Anesth Analg. 1996;82:873–4. doi: 10.1097/00000539-199604000-00036. [DOI] [PubMed] [Google Scholar]
- 4.Yanovski B, Gaitini L, Volodarski D, Ben-David B. Catastrophic complication of an interscalene catheter for continuous peripheral nerve block analgesia. Anaesthesia. 2012;67:1166–9. doi: 10.1111/j.1365-2044.2012.07222.x. [DOI] [PubMed] [Google Scholar]
- 5.Lombard TP, Couper JL. Bilateral spread of analgesia following interscalene brachial plexus block. Anesthesiology. 1983;58:4723. doi: 10.1097/00000542-198305000-00016. [DOI] [PubMed] [Google Scholar]
- 6.Fredrickson MJ, Ball CM, Dalgleish AJ, Stewart AW, Short TG. A prospective randomized comparison of ultrasound and neurostimulation as needle end points for interscalene catheter placement. Anesth Analg. 2009;108:1695700. doi: 10.1213/ane.0b013e31819c29b8. [DOI] [PubMed] [Google Scholar]
- 7.Stundner O, Meissnitzer M, Brummett CM, Moser S, Forstner R, Kokofer A, et al. Comparison of tissue distribution, phrenic nerve involvement, and epidural spreadin standard vs. low volume ultrasound guided interscalene plexus block using contrast magnetic resonance imaging: A randomized, controlled trial. Br J Anaesth. 2016;116:40512. doi: 10.1093/bja/aev550. [DOI] [PubMed] [Google Scholar]
- 8.Fritsch G, Hudelmaier M, Danninger T, Brummett C, Bock M, McCoy M. Bilateral loss of neural function after interscalene plexus blockade may be caused by epidural spread of local anesthetics: A cadaveric study. Reg Anesth Pain Med. 2013;38:648. doi: 10.1097/AAP.0b013e318277a870. [DOI] [PubMed] [Google Scholar]
- 9.Orebaugh SL, McFadden K, Skorupan H, Bigeleisen PE. Subepineurial injection in ultrasound guidedinterscalene needle tip placement. Reg Anesth Pain Med. 2010;35:4504. doi: 10.1097/AAP.0b013e3181e859f0. [DOI] [PubMed] [Google Scholar]
- 10.Maga J, Missair A, Visan A, Kaplan L, Gutierrez JF, Jain AR, et al. Comparison of outside versus inside brachial plexus sheath injection for ultrasound-guided interscalene nerve blocks. J Ultrasound Med. 2016;35:279–85. doi: 10.7863/ultra.15.01059. [DOI] [PubMed] [Google Scholar]
- 11.Krishnan S, Milam A, Shukr M, Ghoddoussi F, Haki J, Terry A, et al. Perioperative pain control with continuous interscalene catheters: A comparison of intra plexus versus periplexus catheter placement. MEJ Anesth. 2017;24:13–9. [Google Scholar]
- 12.Capogna G. Maintenance of labor analgesia. In: Capogna G, editor. Epidural labor analgesia – Childbirth without pain. Switzerland: Springer International Publishing; 2015. pp. 89–101. chapter 8. [Google Scholar]
- 13.Cook LB. Unsuspected extradural catheterization in an interscalene block. Br J Anaesth. 1991;67:473–5. doi: 10.1093/bja/67.4.473. [DOI] [PubMed] [Google Scholar]
- 14.Byeon GJ, Shin SW, Yoon JU, Kim EJ, Baek SH, Ri HS. Infusion methods for continuous interscalene brachial plexus block for postoperative pain control after arthroscopic rotator cuff repair. Korean J Pain. 2015;28:210–6. doi: 10.3344/kjp.2015.28.3.210. [DOI] [PMC free article] [PubMed] [Google Scholar]


