Abstract
Introduction
Disagreement and conflict are inevitable among members of clinical teams, as well as with patients and families during the course of medical care. Despite the importance of physicians needing to negotiate and resolve conflicts, best practices for teaching these skills have not been established in a clinical setting.
Methods
We developed teaching tools based on a conflict resolution model from the business world, emphasizing team dynamics and employing a structured, hierarchical approach to conflict resolution that preserves interpersonal relationships. We employed lessons from diplomacy and improvisational theatre to underscore nonverbal cues that improve communication during conflict. We prepared instructions for teaching conflict management and conflict resolution styles, small-group negotiations, case-based clinical scenarios, personal reflection, and facilitated debrief. The tools are customizable based on audience and available instructional time.
Results
We implemented this resource for over 2 years with 20 pediatric residents and over 150 educators and fellows at national meetings. Participants reported that the topic was timely and important and identified the conflict resolution hierarchy, attention to conflict resolution styles, use of case-based discussion, and focus on nonverbal communication as effective and valuable elements.
Discussion
This resource has been refined over five cycles of presentation and feedback with learners and educators. Our participants identified themes of conflicts in clinical settings that informed the case scenarios presented here, including interdisciplinary conflicts, ethical conflicts, and conflicts among members of the educational hierarchy. These tools are designed to meet established national educational priorities related to communication and professionalism across the educational continuum.
Keywords: Professionalism, Negotiation, Conflict Resolution, Milestones, Nonverbal Communication
Educational Objectives
By the end of this activity, learners will be able to:
-
1.
Identify sources of conflict that may impact performance of medical team members and interfere with attainment of core competencies by medical learners.
-
2.
Recognize team dynamics that can lead to conflict.
-
3.
Employ a structured approach to conflict resolution that emphasizes professionalism and preservation of relationships.
-
4.
Utilize nonverbal communication to maximize cooperation during times of disagreement or conflict.
Introduction
Effective communication and workplace productivity are negatively impacted in the presence of conflict. Conflicts in medical settings include those among members of an interdisciplinary team,1,2 among members of newly formed collaborative groups,3–5 and among team members at different levels of the educational hierarchy (e.g., fellows, residents, interns, and students).6 High-acuity settings, such as the intensive care unit7 and operating room,8 are recognized as sites in which conflict may become more heated due to the pressures of urgency and morbidity encountered there.
Conflict resolution skills are recognized in the evolving priorities of educators. Education in conflict resolution skills was recommended in a 2003 report on improving teaching of professionalism commissioned by the Association of American Medical Colleges.9 More recently, the Accreditation Council for Graduate Medical Education has emphasized using standardized milestones for development of key subcompetencies in graduate medical training. Each specialty or subspecialty has established key milestones for considering its trainees ready to practice independently. For example, of 21 milestone-based subcompetencies required of residents in general pediatrics, eight of them across four of the six core competencies (e.g., systems-based practice, practice-based learning and improvement, professionalism, and interpersonal communication skills) include references to conflict resolution skills.10,11 These skills, reflected in the milestones, include meeting the needs of others, recognizing differing priorities of care team members and patients, collaborating on multidisciplinary medical teams, responding to conversational feedback, being sensitive to emotions and nonverbal communication cues, and exhibiting professionalism in interpersonal interactions.
Despite the recognition of the significance of conflict in the medical setting and the need for developing skills to address it, there is an overall paucity of structured tools to teach these practical skills to medical trainees. Several conflict resolution strategies have been described in medical literature,4,6,8 often based on characteristics and conflict resolution styles originated by Thomas and Kilmann.12 However, these resources tend to be descriptive of conflict resolution strategies (i.e., brief mnemonic devices) without providing detailed tools for teaching how to employ them. Two recent resources in MedEdPORTAL offer some tools for teaching conflict resolution. One is based in personal wellness and focuses on using structured cases to explore gender biases that affect nurse-physician interactions in the emergency department.13 The other uses simulation to emphasize the conflicts that arise from the power differential between members of interprofessional teams.14
With a documented need for making more teaching tools for conflict resolution available in the medical literature, we developed our resource using a model first described in 1972 by Beckhard15 and subsequently refined in the world of business management.5,16 This approach emphasizes, in descending order of priority, the establishment of shared goals, defined roles, effective procedures and processes, and interpersonal interactions. It is commonly referred to as the GRPI (goals, roles, processes, and interpersonal skills) model.
-
•Goals:
-
○Are goals SMART (specific, measurable, attainable, relevant, time-bound)?
-
○Are all goals agreed upon by all members of the team?
-
○Does everyone feel a sense of purpose?
-
○
-
•Roles:
-
○Doss each person have defined responsibilities and authority?
-
○Does each person understand, agree with, and feel satisfied with those responsibilities?
-
○Does each person understand what everyone else does?
-
○
-
•Processes and procedures:
-
○Is there clear communication between team members?
-
○Who has decision-making authority? How are group decisions made?
-
○What is the mechanism for dispute management?
-
○
-
•Interpersonal interactions:
-
○Do individuals trust each other? Are all contributions valued?
-
○Do individuals support each other? Is constructive feedback offered?
-
○Is there genuine friendliness in words and gestures among individuals?
-
○
In order to maximize practice of conflict resolution skills and practical skill development through experimentation and reflection, our instructional methods use Kolb's experiential learning cycle as a cognitive framework.17 The full workshop structure includes two iterations of a brief didactic presentation, a case-based discussion encouraging active experimentation with conflict resolution skills, and a reflection with debrief. After the initial educational experience, learners are instructed to perform self-reflection independently following their own concrete experiences and then participate in facilitated feedback to complete the experiential cycle. Our resource adds to the available content in MedEdPORTAL by broadening from audiences of student learners14 to all medical trainees and from conflicts primarily related to gender biases13 to conflicts encountered in a wide array of clinical, educational, and ethical settings. Furthermore, we have incorporated a memorable strategy for approaching conflict, an emphasis on nonverbal communication, and instructions for longitudinal self-reflection.
Within this resource, we provide all of the necessary materials to teach a structured approach to conflict resolution focusing on preservation of interpersonal relationships and awareness of personal differences in conflict resolution styles. We also provide concrete training in nonverbal communication, which has been acknowledged as important in conflict resolution13 but for which there is also a lack of teaching tools in medical education. This component of the resource draws on lessons derived from international diplomacy and improvisational theatre to make these tools practical and memorable. This resource has been tested and refined with residents, fellows, and undergraduate and graduate medical educators through multiple iterations.
Methods
Each component of the resource is described below. We used the bulk of educational time for interactive learning opportunities; therefore, the didactic component was brief. For an example of how to create an interactive workshop experience from these components, which was our strategy for teaching these skills, see the Conflict Resolution Workshop section below.
Didactic Presentation
To provide the framework for conflict resolution, we used the slide set (Appendix A) covering team dynamics (slide 2), conflict resolution hierarchy (slides 3–5), conflict resolution styles (slides 6–7), and instructions for personal reflection (slide 8). Throughout the didactic presentation, we often paused to relate personal experiences that illustrated the key points, which led to a variable duration of 15–30 minutes for this presentation. We have added facilitator talking points to the notes section under each slide to assist with leading these discussions.
While describing the slides on team dynamics, we presented the developmental phases that multidisciplinary and learner-based medical teams might encounter.3,5 We emphasized the storming phase of team development, during which conflict is most likely, allowing participants to begin planning how to recognize and minimize the disagreements that might arise in practice. The conflict resolution hierarchy was based on the GRPI model described in the business literature (see above).5,15,18 During this section of the didactic presentation, we also distributed and referenced the GRPI side of the pocket card (Appendix B). Using this model, we encouraged individuals to approach conflict situations in a structured fashion, working from the most likely sources of conflict (e.g., incomplete, inappropriate, or mismatched goals) to the least likely source of conflict (i.e., personal incompatibility).
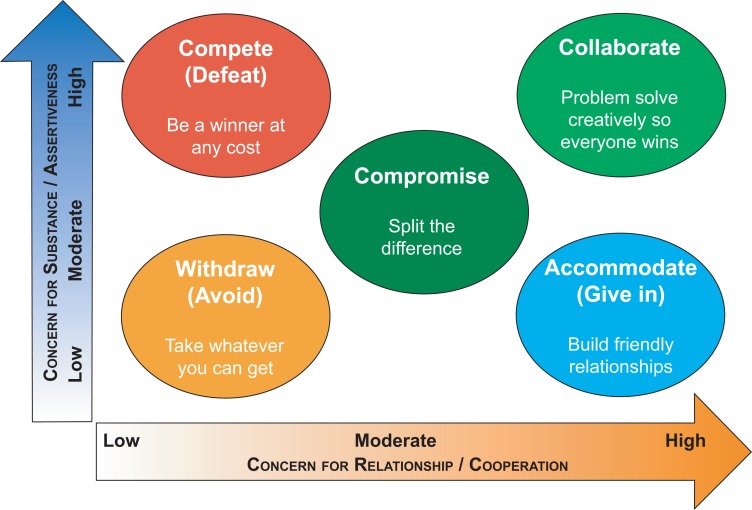
We then presented the conflict resolution styles slides, which combined the key features of styles originally defined by Thomas and Kilmann12 with additions described by others4,6 and are summarized in the Figure. We also referenced the styles side of the pocket card (Appendix B). The goal of this didactic presentation was to make learners aware of the different overall styles and to help them recognize that in any given conflict, they may prioritize their own needs and concern for substance (i.e., assertiveness), another's needs and the quality of the relationship (i.e., cooperation), neither, or both. We emphasized to our learners that one's conflict resolution style may vary among distinct situations and relationships.
Figure. Conflict resolution styles. Adapted from the Thomas-Kilmann Conflict Mode Instrument.
Small-Group GRPI Brainstorm
We spent 5–15 minutes on this exercise, with variability depending on the number of participants. We used slide 4 of the didactic presentation (Appendix A) to provide instructions to learners. This exercise familiarized participants with the types of conflicts in medical settings that fit within the GRPI hierarchy. Following the didactic introduction to GRPI and referencing the pocket card (Appendix B), we asked participants in small groups of three to eight to brainstorm at least one example of a conflict in a medical setting that could be attributed to a problem in goals, one in roles, one in processes, and one in interpersonal interactions. We told them to keep their examples brief. Some groups considered more than one example per category. We instructed the groups to have a scribe/reporter take notes or to use flip charts to document their examples.
After about 5 minutes to brainstorm, we brought the large group back together to share examples. We went through each small group's goals example first, each roles example next, and so on. Some groups identified an example conflict that appeared to cross over to multiple parts of GRPI, and we discussed how they should categorize it at the highest level of the hierarchy (e.g., if a conflict had interpersonal components but also undefined roles, it was considered a roles problem).
At the conclusion of the discussion, we encouraged participants to think of their disagreements and conflicts in these terms moving forward so they could identify how to approach a solution. We frequently reminded them that conflicts due purely to interpersonal incompatibility are rare (see also slide 5 in Appendix A, which illustrates the decreasing frequency of key sources of conflict). We used slide 8 in the didactic presentation (Appendix A) to summarize the personal reflection exercise, in which we gave learners a few minutes to reflect individually after the small-group exercises.
Small-Group Conflict Exercise
Our purpose in this exercise was for learners in small groups to examine a conflict scenario, attempt to negotiate a resolution, and reflect on their approaches to conflict prior to a large-group discussion of conflict resolution strategies. We have conducted this exercise multiple times with multiple audiences and summarize our approaches as follows. The exercise took 20–30 minutes to complete: 10–15 minutes for small-group discussion, 5–10 minutes for groups to report, and 5 minutes for reflection.
Based on learner and educator feedback, we developed clinical scenarios that could be used for conflict resolution discussions (Appendix C). The approach we used in developing scenarios is summarized below and can be used in the preparation of new scenarios.
First, we identified a topic. We found that the ideal topic could be presented in an open-ended and neutral way, leave much open to interpretation, and reliably provoke disagreement among different small-group members. We considered items in the recent literature or news, as well as issues that arose locally. We utilized topics that did not have an obvious or correct answer, on which team members would likely disagree intellectually, culturally, or emotionally.
We created conflict scenarios from topic areas that were either medical or nonmedical. We chose topics such that all participants would have baseline familiarity with them. Ethical dilemmas were especially appropriate. We frequently used derivations of the previously published case of a family requesting a white doctor19 and the issue of state-sanctioned medical euthanasia in Belgium20 as starting points for discussion. We have provided detailed example scenarios in clinical, educational, and ethical settings in Appendix C.
Other general topics we have used for conflict scenarios are euthanasia, medically necessary blood transfusion in children whose families are Jehovah's Witnesses, medical futility hospital policies and laws, decisions to resuscitate or not resuscitate preterm neonates at the margins of viability, and the discharging or barring of vaccine-refusing families from pediatric practices.
For nonmedical topics to promote conflict, we chose timely political and social topics, such as upcoming political election candidates or issues, and recent referenda or legal decisions (e.g., relating to same-sex marriage, abortion, contraception, affirmative action, and gun control).
After selecting the topic for discussion, we neutrally phrased it as an open-ended question or task, as illustrated in the scenarios shown in Appendix C. Some other questions we have used with learners include the following:
-
•
Your team has been asked to outline a hospital policy regarding resuscitation of extremely preterm infants following a neonatologist's recent choice to aggressively resuscitate a 22-week preterm boy who subsequently lived for 16 hours before dying of pulmonary hemorrhage.
-
•
A pregnant 41-year-old woman carrying a fetus with trisomy 21 has told a member of your practice that she plans to have an elective abortion because of the possible disabilities he will face. What is your team's response to her plan?
-
•
How do you feel about the candidates for an upcoming general election?
-
•
Describe the qualities most important for the next Supreme Court justice.
Once the topic was selected and the question written, the small-group exercise was conducted as follows. We divided our participants into small groups of three to eight people and then provided the discussion task/question either as a handout or projected as a slide. Groups were given 10–15 minutes for discussion, during which they had to produce a written response to the task/question. The response had to be drafted by consensus, meaning that every member of the group agreed completely with the response. We emphasized this definition of consensus to ensure that there would be opportunity for disagreement during the discussions.
The intent of this exercise was to provoke disagreement or conflict between small-group members. It was possible, and occurred frequently, that some groups did not reach a consensus response in the allotted time. Sometimes, groups chose to reinterpret the task/question or redefine its terms in order to reach a stronger agreement. Some groups also chose to assign roles to members (e.g., leader, recorder, timekeeper).
Following the small-group discussion, the large group reconvened, and we facilitated a debrief on the exercise. Each group read out its consensus response to the task/question. We then asked members of the groups to describe the steps by which they had reached, or had not reached, consensus. Questions we asked included these:
-
•
How did each group start the discussion?
-
•
Did each member state an opening opinion/position?
-
•
Was there an effort made to define, or redefine, the problem?
-
•
What roles did different group members play?
-
•
In hindsight, were there roles left unfilled?
-
•
What difficulties did each group encounter during the discussion?
-
•
Did the group identify a process for reaching agreement?
This exercise concluded with 5 minutes for individuals to reflect on the experience. We used slide 8 from Appendix A to guide group discussion after reflection. Topics we considered during reflection included the following:
-
•
What frustrations did you experience personally while having this discussion?
-
•
Were there arguments?
-
•
To what extent did you represent your beliefs?
-
•
To what extent did you make compromises?
-
•
To what extent did you get angry?
-
•
To what extent did you listen to others?
Note that these were personal responses and were optional to share with the large group.
Exercises in Nonverbal Communication
Overall, our workshops included 20–30 minutes to conduct the interactive nonverbal communication exercises illustrated on the slides in Appendix D. We have added facilitator talking points to the notes section under each slide to assist with leading these discussions. The introductory slide (slide 2) described different categories of nonverbal communication, including those relating to behavior, body language, and speech modulation. The following slides (slides 3–11) contained photographs of diplomats, and participants were instructed to critique the quality and tone of the interactions based on nonverbal cues. For example, learners were invited to infer the attitudes of the diplomats from how they were seated or positioned, their facial expressions, and their eye contact. We spent 2–3 minutes per photograph allowing the participants to brainstorm the communication exhibited.
For each presentation, we selected the photographs that seemed best for our learner audience to critique. We first showed slide 3 of the set, giving instructions on how to evaluate the nonverbal emotions and cues on display in the photographs. We have located additional images for critique easily using online image searches for diplomacy photos. We have obtained further ideas for critiquing nonverbal communication in government, popular culture, and other venues using online resources.21
We then performed the improvisational theatre exercise in nonverbal communication described in slides 12–13. We started with small groups of up to 10 participants and instructed them to count to 20. We provided the following rules:
-
•
Individuals could only speak using numbers during the exercise.
-
•
No one person could say more than a single number in a row (i.e., they had to take turns).
-
•
If a participant said anything other than a number, repeated a number, skipped a number, or talked at the same time as someone else, the group had to start over at one.
The goal of the exercise was to teach the group members to use nonverbal cues to anticipate their turn to count. We reminded participants that this exercise was as much about silence in communication as about effectively reaching the objective.
This task was not difficult for groups that knew each other well. Often, group members discovered that they could raise a hand or wave prior to counting the next number. This allowed them to achieve the objective rapidly. To make the exercise more difficult, we then combined several small groups to form a larger group. We also asked everyone to close their eyes and start again. Eventually, group members used a clap or other sound to indicate that they were next to count. This was one way to achieve the objective without visual cues.
The final nonverbal communication exercise we employed (slides 14–19) was a series of tongue twisters. We chose one or two of the tongue twisters depending on the available time. The purpose of the tongue twisters was to emphasize precision in language rather than speed. We encouraged participants to read the tongue twisters out loud as a large group, slowly, with precise articulation of consonant sounds. The deliberate speed required to speak these tongue twisters seemed slow, but we suggested that this pace better approximated the speech rate needed to have difficult clinical conversations without being misunderstood.
Conflict Resolution Workshop
We combined the above didactic, small-group, and reflective exercises into a single workshop of 120–180 minutes, as shown in Table 1.
Table 1. Sample Workshop Agenda.
| Time | Topic | Appendix |
|---|---|---|
| 5 min. | Introduction, review of goals and objectives. | |
| 10–15 min. | Small-group conflict resolution case discussion one. Participants are given a challenging and emotional topic on which to negotiate and come to a consensus conclusion. | C |
| 15 min. | Small groups report and debrief. Groups report their consensus decision and review the challenges that faced them in approaching the topic. | |
| 5–15 min. | Team dynamics and conflict resolution hierarchy large-group didactic. Discussion of group dynamics that lead to conflict, presentation of a structured approach to conflict resolution. | A, B |
| 10 min. | Small-group GRPI brainstorm. Groups identify at least one conflict situation or theme that faces physicians or learners, attributable to problems with GRPI (at least one example for each). Scribe versus flip chart and report. | B |
| 10 min. | Small groups report out their GRPI themes. Large group discusses types of conflict participants have experienced in medicine. | |
| 10 min. | Conflict resolution styles large-group didactic. | A, B |
| 5–15 min. | Break. | |
| 10–20 min. | Small-group conflict resolution case discussion two. Select a different case, intended to be more emotionally/ethically challenging. Participants are advised to try to use GRPI during discussion. If time allows, use the last 5 minutes for individual self-reflection. | B, C |
| 10 min. | Small groups report and debrief. Groups report their consensus decision and review the challenges that faced them in approaching the topic. Reflect on whether the workshop tools were used and whether they were successful. What questions still remain? | |
| 5 min. | Nonverbal communication overview. | D |
| 10–15 min. | Group critique of nonverbal cues in diplomacy. Images of diplomatic discussions are critiqued based on nonverbal features. Brainstorm for 3 minutes per image, for three to five images. | D |
| 5–15 min. | Small-group nonverbal cues exercise. An exercise from improvisational theatre requires participants to observe each other and communicate without speech to accomplish an objective. Consider adding one or more tongue twisters depending on time. | D |
| 10–15 min. | Large-group debrief and discussion of personal approaches and barriers to conflict resolution education. | |
| 5 min. | Wrap-up and workshop evaluation. Hand out personal self-reflection form, give participants several weeks to complete, and set a future date to come back together to discuss the conflicts they have experienced. | E, F |
Abbreviation: GRPI, goals, roles, processes, and interpersonal skills.
Learner Self-Reflection
Following our workshop, we gave residents an assignment to reflect on the lessons learned, apply their skills in their own clinical experiences, and identify further areas for self-improvement over time. We provided our learners with the self-reflection worksheet (Appendix E). We asked them to explore a single personal experience with conflict during their clinical encounters and to reflect on their skill in communication. We gave our learners 6 weeks to complete the activity, collected the worksheets, and then reconvened the full group at a future session to discuss their collective experiences and lessons learned.
Before reconvening to discuss the reflections, we collected and reviewed the learner responses to identify common themes. We then brought the group together for the follow-up discussion, budgeting 20–30 minutes for this. We discussed areas for improvement in conflict resolution among the group, particularly those relevant to the themes identified in self-reflection. We asked learners to share their individual conflict situations with each other. We then opened the discussion to the themes and self-critiques that arose from review of the self-reflections. We asked the group to consider and discuss the following questions:
-
•
Have you been attentive to using a structured approach to conflict resolution in clinical settings?
-
•
Has this approach been helpful?
-
•
How could we better prepare you to approach conflict situations more skillfully?
Learner Self-Assessment
We have considered multiple tools available for assessment of the conflict resolution styles introduced in the didactic presentation (Appendix A)12,22,23 but have not endorsed any specific assessment tool or commercial product. We did encourage our learners to independently review these materials to gain a sense of their basic approach to conflict, if desired. They were informed during our workshop that recognizing one's own baseline style and the descriptions of the other styles may be helpful in adjusting to specific conflict situations. We also noted that an individual's approach to conflict and disagreement may change based on the relationships in and substance of specific conflicts.
Evaluation of the Educational Experience
After each didactic presentation, group exercise, and workshop, we distributed the evaluation form (Appendix F) and asked the participants to evaluate the quality of the educational content and facilitators.
Results
We conducted the workshop integrating didactic, small-group activities, and nonverbal communication exercises with two classes of 10 first-year residents in pediatrics. In their second year, one resident class participated in the workshop a second time. We also presented the workshop to educators in undergraduate and graduate medical education on three occasions in 2016–2017. One group of 16 (15 educators, one fellow) participated in the workshop at the Southern Regional Meeting (SRM) of the Academic Pediatric Association in 2016, and another group of 32 (30 educators, two fellows) participated at the Pediatric Academic Societies meeting in 2016. This latter workshop was part of the meeting core curriculum, as well as part of the meeting tracks in quality improvement/patient safety, education, and leadership/career development. Following refinement of the workshop content after these presentations, we presented this material to 120 pediatric residency and fellowship program directors, coordinators, and chief residents at the Association of Pediatric Program Directors spring meeting in 2017.
Following each workshop experience, participants completed the evaluation form (Appendix F). We asked participants (learners and educators) to rate their agreement with five statements on a 5-point Likert scale (1 = strongly disagree, 5 = strongly agree). Respondent numbers, questions asked, and mean Likert-scale responses are shown in Tables 2, 3, and 4.
Strengths of the Teaching Tools
In addition to the Likert-scale responses, we asked participants to share as free responses their evaluation of which parts of the workshop were most effective and helpful, areas of uncertainty on the topic, and suggestions for improving the content or delivery of the workshop.
We combined the free responses to two evaluation questions, “What did you learn today that you plan to apply in the clinical or educational setting?” and “What was the most valuable aspect of this session?” We conducted an informal analysis of themes from the participant answers to these two questions. Responses encountered more than once (with the number of instances of the responses given in parentheses) included these:
-
•
GRPI conflict resolution hierarchy (73 educators, five first-year residents, three second-year residents).
-
•
Small-group exercises (13 educators, two first-year residents, two second-year residents).
-
•
Nonverbal communication content (11 educators).
-
•
Cases for discussion (10 educators).
-
•
Attention to conflict resolution styles (seven educators).
-
•
Didactic presentation (four educators).
-
•
Good review/improvement from previous year (two second-year residents).
Opportunities for Improvement of the Teaching Tools
In order to identify areas to improve this content, we reviewed for any corrective comments in the free responses to two evaluation questions, “What is still unclear?” and “How can we improve this session?” We conducted a similar informal analysis of themes from participant answers. Responses encountered more than once (with the number of instances of the responses given in parentheses) included the following:
-
•
More clinical case scenarios and examples of conflict, including professionalism conflicts (15 educators, eight first-year residents).
-
•
More direction for small-group exercises (five educators).
-
•
How to set goals during a discussion or meeting (four educators).
-
•
Video examples or demonstrations of conflicts for group critique (four educators).
-
•
Handouts to be given early in workshop (four educators at SRM session).
-
•
Examples of conflict when a power differential exists, such as with a trainee and attending physician (three educators).
-
•
How to follow up after a conflict (three educators).
-
•
Too repetitive in second year (three second-year residents).
-
•
How to work with emotional responses in conflict situations (two educators).
We modified the content of these teaching materials with each iteration of the workshop based on the above responses, including adding additional case scenarios (Appendix C) and adjusting the small-group exercise instructions.
Themes Identified in Resident Self-Reflection
Both years that we ran the workshop with our residents, we conducted the self-reflection exercise described above. We distributed a worksheet (Appendix E) to residents at the conclusion of the workshop and gave them 6 weeks to complete it. Themes that residents reported (i.e., sources of conflict exhibited by multiple respondents, followed by examples) in their conflict situation examples included the following:
-
•
Lack of effective communication (e.g., between subspecialists and primary inpatient team, among members of a critical care team, between care team and parents of patient).
-
•
Learner-to-attending physician conflicts (e.g., attending physician dictating care plan that contradicts resident's understanding of the evidence without offering an explanation; attending physicians in conflict, with resident feeling stuck in the middle or disempowered to join the conversation; resident feeling blamed for a decision made by another provider).
-
•
Lack of agreement on priorities of workflow (e.g., resident expected to discharge and admit patients simultaneously, resident expected to discharge patient he/she has never met).
-
•
Angry parent/patient.
Approaches that the residents reported using during their conflicts included GRPI and reflective listening. However, some residents indicated they “did not approach the conflict well” or that they “should have taken more time to discuss with attending” physician.
We added these themes to the sample conflict cases (Appendix C) that we discuss when teaching learners at our institution.
Discussion
This resource was developed for medical trainees following an assessment of the available literature and peer-reviewed teaching tools for conflict resolution. Although we found ample recognition of the importance of conflict resolution skills and national educational recommendations that included increased attention to these skills, there remained a paucity of published practical tools for teaching conflict resolution in the medical setting.
Our conflict resolution materials are derived from materials found in the business literature, augmented with medical examples of conflict and team dynamics as well as nonverbal communication training materials that utilize lessons learned from improvisational theatre and diplomacy. Following five iterations of presenting these materials to learners and educators, this resource represents refinements made based on reflective critique after each iteration.
Lessons Learned
Both learners and educators reported these tools to be timely, helpful, and useful. Evaluations lauded the GRPI approach to conflict resolution, focus on team dynamics, small-group interactive exercises, attention to conflict resolution styles, and attention to nonverbal communication as key benefits of participation. The workshop agenda has been modified over time to increasingly emphasize these components most valued by learners and educators.
Educators at three national workshops suggested that we add more clinical case scenarios of conflicts to our small-group exercises and resources. This recommendation was echoed in the residents' responses to the self-reflection exercise, in which they identified key themes of conflict within the learner-educator hierarchy and in emotionally stressful clinical situations. These themes have been described in the literature as well.6,7 In response, we have expanded the number and breadth of conflict scenarios to incorporate these conflict themes into the workshop (Appendix C). The topics represented now include clinical, educational, and ethical challenges.
Our second-year resident learners were less enthusiastic about the workshop when they experienced it for the second time a year later, as evidenced by their lower Likert-scale responses (Table 2). The sample size of this group was admittedly small, but nevertheless, their most frequent comment on the evaluation was that the content was repetitive during their second time participating. In response to this finding, our advanced communication curriculum now offers the conflict resolution workshop only for first-year residents, and we utilize small-group discussion combined with self-reflection on sources of conflict and approaches to conflict resolution with our senior residents. We are also exploring opportunities to involve senior residents as mentors to interns in developing conflict resolution skills during ward rotations.
Table 2. Children's Hospital of San Antonio Workshop Evaluationa.
| Pediatric Residents | ||
|---|---|---|
| Question | First Year (n = 19) | Second Year (n = 9) |
| Workshop met objectives | 4.7 | 4.3 |
| Handouts were helpful | 4.2 | 3.9 |
| Didactics were clear and informative | 4.6 | 4.1 |
| Small-group exercises were beneficial | 4.6 | 4.1 |
| I will apply information learned today | 4.7 | 4.1 |
Using a 5-point Likert scale, where 5 = strongly agree.
For the SRM workshop presentation, we trialed withholding the teaching handouts until the conclusion of the workshop due to a concern that they would prove distracting when we were encouraging small-group participation. The evaluation results did not support the efficacy of this choice (see Table 3 and Results, above). We now provide handouts (pocket cards, scenario descriptions, references) early in the workshop experience for both learners and educators. For the Association of Pediatric Program Directors workshop, we provided handouts electronically in advance, and this approach appeared successful (Table 4).
Table 3. Faculty Educators Workshop Evaluationa.
| Question | Southern Regional Meeting of Academic Pediatric Association (n = 16) | Pediatric Academic Societies (n = 24) |
|---|---|---|
| Workshop met objectives | 4.6 | 4.7 |
| Handouts were helpful | 4.1 | 4.5 |
| Didactics were clear and informative | 4.7 | 4.6 |
| Small-group exercises were beneficial | 4.3 | 4.5 |
| I will apply information learned today | 4.6 | 4.6 |
Using a 5-point Likert scale, where 5 = strongly agree.
Table 4. Pediatric Educators Workshop Evaluationa.
| Question | Association of Pediatric Program Directors (n = 43) |
|---|---|
| Workshop met objectives | 4.8 |
| Handouts were helpful | 4.7 |
| Didactics were clear and informative | 4.8 |
| Small-group exercises were beneficial | 4.7 |
| I will apply information learned today | 4.8 |
Using a 5-point Likert scale, where 5 = strongly agree.
In response to evaluation by educators at our workshops, the most recent addition to the workshop content and pedagogy was drawing explicit attention to training subcompetencies and milestone language relevant to conflict resolution.10 This approach is intended to engage educators in appreciating the significance and depth of this content in educating residents and fellows as communicators. It also identifies discrete qualities to observe when evaluating trainee communication skills.
Limitations
Our resource has been implemented with 20 resident learners at our home institution, a relatively small number limited by the size of the annual resident class of 10. We also shared this content with a broader audience of medical educators, and feedback from all groups has shaped the iterative modifications to the teaching tools. The evaluation of these materials has been largely perception based, and impact on clinical performance is at this time inferential. Looking to the future, we anticipate development of a validated assessment tool for conflict resolution skills in medical settings, which will allow us to identify individual learners' strengths and areas for improvement.
Educators planning to implement these resources will require a means to project the didactic slide sets (e.g., computer, projector, screen). Use of the conflict scenarios, pocket card, reflection, and evaluation will likely require a printer or photocopier. We anticipate that this equipment requirement is modest and that most medical educators should be able to utilize our materials.
We envision this resource being part of a longitudinal approach focused on developing physician communication skills as a step toward key professionalism and medical practice competencies. Ultimately, patient care quality and satisfaction should benefit from physicians' effective communication skills.
Appendices
A. Didactic.pptx
B. Pocket Card.pdf
C. Scenarios.docx
D. Nonverbal Slides.pptx
E. Reflection.docx
F. Evaluation.docx
All appendices are peer reviewed as integral parts of the Original Publication.
Disclosures
None to report.
Funding/Support
Adam D. Wolfe was a 2015–2016 recipient of the Texas Children's Hospital Educational Scholarship Award, a competitive intramural grant that provided funds to support development, implementation, and evaluation of the curriculum described here.
Prior Presentations
Wolfe AD, Denniston SF. Conflict resolution: lessons from business, diplomacy, and theatre. Workshop presented at: Southern Regional Meeting of the Academic Pediatric Association; February 2016; New Orleans, LA.
Wolfe AD, Denniston SF. Conflict resolution: lessons from business, diplomacy, and theatre. Workshop presented at: Pediatric Academic Societies Annual Meeting; April 2016; Baltimore, MD.
Wolfe AD, Hoang K, Denniston SF. Teaching conflict resolution on the road to milestone attainment: lessons from business, diplomacy, and theatre. Workshop presented at: Association of Pediatric Program Directors Annual Spring Meeting; April 2017; Anaheim, CA.
Ethical Approval
Reported as not applicable.
References
- 1.Brown J, Lewis L, Ellis K, Stewart M, Freeman TR, Kasperski MJ. Conflict on interprofessional primary health care teams—can it be resolved? J Interprof Care. 2011;25(1):4–10. https://doi.org/10.3109/13561820.2010.497750 [DOI] [PubMed] [Google Scholar]
- 2.Lifchez SD, Cooney CM, Redett RJ III. The Standardized Professional Encounter: a new model to assess professionalism and communication skills. J Grad Med Educ. 2015;7(2):230–233. https://doi.org/10.4300/JGME-D-14-00275.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tuckman BW. Developmental sequence in small groups. Psychol Bull. 1965;63(6):384–399. https://doi.org/10.1037/h0022100 [DOI] [PubMed] [Google Scholar]
- 4.Saltman DC, O’Dea NA, Kidd MR. Conflict management: a primer for doctors in training. Postgrad Med J. 2006;82(963):9–12. https://doi.org/10.1136/pgmj.2005.034306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Raue S, Tang S-H, Weiland C, Wenzlik C. The GRPI model—an approach for team development [white paper draft]. Systemic Excellence Group website. http://www.segroup.de/library/public/Paper_Raue_Tang_Weiland_Wenzlik_The_GRPI_Model.pdf Updated February 18, 2013.
- 6.Mallidi J. How to handle conflict with poise?: a fellow's perspective. J Am Coll Cardiol. 2015;65(1):98–100. https://doi.org/10.1016/j.jacc.2014.11.012 [DOI] [PubMed] [Google Scholar]
- 7.Paquette ET, Kolaitis IN. Intensive care, intense conflict: a balanced approach. J Clin Ethics. 2015;26(4):346–349. [PubMed] [Google Scholar]
- 8.Lee L, Berger DH, Awad SS, Brandt ML, Martinez G, Brunicardi FC. Conflict resolution: practical principles for surgeons. World J Surg. 2008;32(11):2331–2335. https://doi.org/10.1007/s00268-008-9702-x [DOI] [PubMed] [Google Scholar]
- 9.Inui TS. A Flag in the Wind: Educating for Professionalism in Medicine. Washington, DC: Association of American Medical Colleges; 2003. [Google Scholar]
- 10.The Pediatrics Milestone Project: a joint initiative of the Accreditation Council for Graduate Medical Education and the American Board of Pediatrics. Accreditation Council for Graduate Medical Education website. http://www.acgme.org/acgmeweb/Portals/0/PDFs/Milestones/PediatricsMilestones.pdf Published 2013. Accessed May 19, 2015.
- 11.Bogetz AL, Rassbach CE, Chan T, Blankenburg RL. Exploring the educational value of patient feedback: a qualitative analysis of pediatric residents’ perspectives. Acad Pediatr. 2017;17(1):4–8. https://doi.org/10.1016/j.acap.2016.10.020 [DOI] [PubMed] [Google Scholar]
- 12.Thomas KW, Kilmann RH. The Thomas-Kilmann Conflict Mode Instrument. Tuxedo, NY: XICOM; 1974. [Google Scholar]
- 13.Welch J, Jimenez H, Allen S. Teamwork & conflict management workshop. MedEdPORTAL. 2013;9:9605 https://doi.org/10.15766/mep_2374-8265.9605 [Google Scholar]
- 14.Shrader S, Zaudke J. Crucial conversations and conflict resolution interprofessional simulation. MedEdPORTAL. 2015;11:10063 https://doi.org/10.15766/mep_2374-8265.10063 [Google Scholar]
- 15.Beckhard R. Optimizing team-building efforts. J Contemp Bus. 1972;1(3):23–32. [Google Scholar]
- 16.Tichy NM. Managing Strategic Change: Technical, Political, and Cultural Dynamics. New York, NY: Wiley; 1983. [Google Scholar]
- 17.Kolb DA. Experiential Learning: Experience as the Source of Learning and Development. Englewood Cliffs, NJ: Prentice-Hall; 1983. [Google Scholar]
- 18.Tichy NM, Cohen E. The Leadership Engine: How Winning Companies Build Leaders at Every Level. New York, NY: Harper Collins; 1998. [Google Scholar]
- 19.Reynolds KL, Cowden JD, Brosco JP, Lantos JD. When a family requests a white doctor. Pediatrics. 2015;136(2):381–386. https://doi.org/10.1542/peds.2014-2092 [DOI] [PubMed] [Google Scholar]
- 20.Aviv R. The death treatment. New Yorker. June 22, 2015:56–65. https://www.newyorker.com/magazine/2015/06/22/the-death-treatment
- 21.Body Language Success & Emotional Intelligence website. http://www.bodylanguagesuccess.com Accessed January 13, 2017.
- 22.Conflict Resolution Questionnaire. University of Arizona website. http://academic.engr.arizona.edu/vjohnson/ConflictManagementQuestionnaire/ConflictManagementQuestionnaire.asp Accessed October 26, 2017.
- 23.Conflict Resolution Style Inventory. Rice University Wellbeing & Counseling Center website. http://co1.qualtrics.com/SE/?SID=SV_aVIkbcK1potoRyB&Q_JFE=0& Accessed October 26, 2017.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A. Didactic.pptx
B. Pocket Card.pdf
C. Scenarios.docx
D. Nonverbal Slides.pptx
E. Reflection.docx
F. Evaluation.docx
All appendices are peer reviewed as integral parts of the Original Publication.