Abstract
Introduction
Ischemic priapism is a urologic emergency managed by both urologic and nonurologic providers in the community. Given ischemic priapism's rare occurrence and the time-sensitive nature of treatment, effective provider education on management of this entity is imperative. We sought to develop a low-cost effective simulation model and curriculum to enhance trainee education.
Methods
A comprehensive didactic curriculum based on national urologic guidelines was developed, along with a low-cost, easily reproducible priapism simulator using hot dogs and Red Vines candy. The simulators cost $1.25 each, and assembly took 10 minutes. All materials were reviewed by three urology faculty members. The curriculum was piloted with two andrology fellowship–trained urology faculty among eight urology residents (PGY2-PGY4/U1-U2) and one medical student. Participants provided feedback regarding the overall course as well as the face and content validity of the simulator.
Results
Cognitive test scores significantly improved on average by 15.0% (p = .002), and confidence improved from baseline somewhat or very much among 88.9% of participants after completion of the curriculum. The task trainer was rated easy to use (average score: 4.78 out of 5), and 77.8% of participants though it was somewhat or very useful for training (average score: 4.00 out of 5). Additionally, 77.8% recommended its incorporation into resident training (average score: 4.00 out of 5).
Discussion
This simulation curriculum is effective, inexpensive, and easily reproducible, making it ideal for groups with limited resources. Expanding access to simulation-based curricula on priapism management may improve education of both urologic and nonurologic trainees.
Keywords: Simulation, Urology, Emergency Medicine, Priapism, Urologic Emergencies, Corporal Aspiration, Corporal Irrigation
Educational Objectives
By the end of this session, learners will be able to:
-
1.
Identify the differences in diagnostic physical exam findings and laboratory studies that differentiate ischemic and nonischemic priapism in the acute setting.
-
2.
Describe the differences in management approach to ischemic and nonischemic priapism in the acute setting.
-
3.
Identify underlying modifiable risk factors for acute ischemic priapism.
-
4.
Identify long-term sequelae of acute ischemic priapism.
-
5.
Demonstrate appropriate patient counseling on acute ischemic priapism and obtain informed consent for bedside interventions.
-
6.
Demonstrate effective stepwise bedside management of acute ischemic priapism, using a performance checklist for assessment.
-
7.
Effectively identify when bedside intervention is unlikely to be successful and when urologic consultation and surgical intervention are warranted in the management of acute ischemic priapism.
Introduction
Priapism is a urologic emergency defined as a persistent penile erection lasting more than 4 hours beyond or unrelated to sexual stimulation.1 It may be ischemic or nonischemic. The overall incidence of priapism has been estimated to range from 0.80 to 1.50 per 100,000 males each year in international cohorts and as high as 5.34 per 100,000 males annually within the United States.2–5 These patients frequently present to the emergency department and need urgent assessment and intervention in order to avoid long-term sequelae of erectile dysfunction. Though urologic consultation is often requested for these patients, the emergency medicine (EM) physician may ultimately be the primary provider for such patients in communities where urology assistance is not timely or available. Thus, it is imperative that both urologic and nonurologic providers are appropriately educated and comfortable with the acute management of this entity.
Although familiarity among urology trainees with this entity is critical, the educational experiences of EM trainees and the attitudes of such nonurology providers towards a primarily urologic entity are not well defined. Thus, we performed an initial educational needs assessment of EM residents, program directors, and associate program directors at Accreditation Council for Graduate Medical Education–accredited EM residency programs. Respondents included 227 residents from 37 unique programs and 91 program directors and assistant program directors from 73 unique programs.6 Over 75% of resident respondents deemed education on priapism management essential or very important, but 36% deemed their existing curricula insufficient to prepare them for independent management of this entity. Even more notable was that 17% of senior residents (PGY3 and PGY4) reported feeling not at all confident in their ability to independently manage priapism. Though 80% of programs reported having a formal priapism curriculum and 43% of program directors deemed simulation to be the most effective singular method to teach residents about priapism management, only 20% of programs with priapism curricula incorporated simulation.
Prior surgical education research has demonstrated the transferability of procedural skills obtained from simulation-based learning, and there are already several well-established cadaveric, animal, virtual-reality, and benchtop-based simulation models for specific urologic procedures.7,8 Yet there are no commercially available priapism task trainers. Review of the EM and urology literature further revealed a paucity of well-established training models for this entity. Indeed, only one published article could be found on PubMed on this subject to date. The described model allowed learners to practice corporal aspiration and irrigation but cost $70 to $120 to construct and required about 45 minutes of assembly time for a single unit.9 Though there are several simulation-based curricula found in MedEdPORTAL, including a novel suprapubic catheter task trainer10 and a low-fidelity abdominal hysterectomy trainer,11 there are no prior publications within MedEdPORTAL regarding simulation models for priapism.
To address this need, we sought to develop a simulation-based curriculum utilizing a novel task trainer for acute ischemic priapism management. Given the similar impact of low-fidelity simulator models and more sophisticated cadaver models on inexperienced learners, we decided to develop a low-fidelity task trainer in order to prioritize a low-cost model that could be easily reproducible among large cohorts of novice learners.12 This would include junior urology residents as well as EM residents. The primary goals were to improve learner knowledge and confidence in performing bedside corporal aspiration, irrigation, and injection in the management of acute ischemic priapism.
Methods
A 30-minute didactic lecture was developed based on current American Urological Association guidelines on priapism management, with an emphasis on the pathophysiology, diagnosis, and stepwise management of acute ischemic priapism (Appendix A).1 This was reviewed by two andrology fellowship–trained urology faculty, as well as a third faculty member with expertise in simulation-based curriculum development, to ensure that the content was comprehensive and appropriate for learners at the beginner level.
To accompany this lecture, a low-fidelity task trainer model was created utilizing two hot dogs, Red Vines candy, and tape. The model was constructed by wrapping the tape around two hot-dog corpora cavernosa and one Red Vines–candy urethra that was ventrally oriented between the two hot dogs (Appendix B). The model demonstrated the relevant anatomic features pertinent to intracorporal aspiration, irrigation, and injection and was designed to be manipulated by learners in order to practice all three maneuvers. Each learner was assigned one model, and the models were not reusable between educational sessions.
The target audience for this curriculum included junior urology trainees and all levels of EM trainees (PGY1, PGY2, PGY3, and PGY4), as they were expected to have limited to no experience with priapism management. Junior urology trainees were defined as those in their first or second year of urology training (U1 or U2) and included PGY2/U1, PGY3/U2, and PGY4/U2 research residents who were not clinically active. Prerequisite knowledge for the curriculum included medical school training and knowledge of basic penile anatomy, as well as basic knowledge of the pathophysiology of priapism. Prerequisite skills included understanding and ability to maintain basic sterile technique, as well as familiarity with local anesthetic injection. We hypothesized that the curriculum might also be applicable to senior-level medical students interested in urology, as they would potentially also have the prerequisite knowledge and skills, although they were not the primary intended audience for this curriculum.
We performed a prospective pilot study of the simulation curriculum in the University of Washington WWAMI Institute for Simulation in Healthcare (WISH) Center during three planned educational sessions for urology residents. The study was granted approval by the University of Washington Institutional Review Board. Urology residents were chosen for this pilot because they were more likely to have clinical exposure to priapism, which provided a comparable standard for evaluation of the task trainer. Moreover, we believed that demonstrating an added educational value among a more experienced and knowledgeable cohort of learners would be the most rigorous demonstration of the curriculum's value.
The educational sessions were 80 minutes long and led by one of two andrology fellowship–trained urologists who were familiar with the didactic lecture and task trainer. A separate observer was present at all three sessions to ensure consistency in the format of each session. Three students attended each session. A 10-minute cognitive pretest (Appendix C) was administered at the start of the session. The 30-minute didactic lecture (Appendix A) was then presented in an interactive lecture format by the course facilitators, following which a 10-minute cognitive posttest (Appendix C) was administered. Next, a 30-minute simulation session utilizing the task trainer was facilitated by the instructors. This simulation session included opportunities for learners to review the relevant anatomy, identify safe locations for intracorporal needle placement, and practice intracorporal aspiration, irrigation, and injection. Additional materials were provided along with the task trainer to allow practice of these maneuvers, as outlined in Appendix B. All trainees were expected to demonstrate appropriate counseling, informed consent (Appendix D), and stepwise bedside management for acute ischemic priapism by the end of the session. The suggested steps for simulation and clinical practice are listed in Appendix E. Immediate feedback was provided to each learner by the facilitator based on a standard simulation checklist (Appendix F).
Upon completion of the course, all learners filled out an anonymous course evaluation (Appendix G). This evaluation asked learners about their level of training and prior experience with managing priapism. Using a Likert scale, it also solicited specific opinions about the utility of the curriculum, its effect on perceived confidence in priapism management, and the utility of the task trainer. Self-confidence was deemed a relevant metric for curriculum evaluation because such bedside procedures for priapism management may be performed independently by trainees with minimal attending supervision. An additional feedback form regarding the fidelity and perceived utility of the task trainer was also completed by all learners (Appendix H). This form queried learners using a Likert scale on the ease of use, anatomic accuracy, realism, and performance of the task trainer as a simulation tool, as well as the potential for educational or credentialing use of the task trainer. As the learners in this pilot study were already largely experienced in priapism management in the clinical setting, their assessment of these constructs for the task trainer was deemed relevant.
Mean and standard deviation were determined for the evaluation scores from the entire cohort. All pre- and posttests were scored by a single blinded evaluator. A two-tailed Student paired t test was used to evaluate the change in cognitive test scores for each learner following the simulation curriculum.
Results
Eight junior-level urology residents (three PGY2/U1, three PGY3/U2, and two PGY4/U2) and one fourth-year visiting medical student on a urology subinternship completed the pilot curriculum. All eligible junior residents within the urology residency program participated. All but two participants had previously managed a case of priapism in clinical practice. The pilot sessions were held during the first quarter of the year.
The cost of 10 task trainer models for these educational sessions was $1.25 each. About 10 minutes was required to complete the setup. Assessment of individual learners was done in real time by the instructors using the simulation checklist (Appendix F), with all participants satisfactorily completing the module.
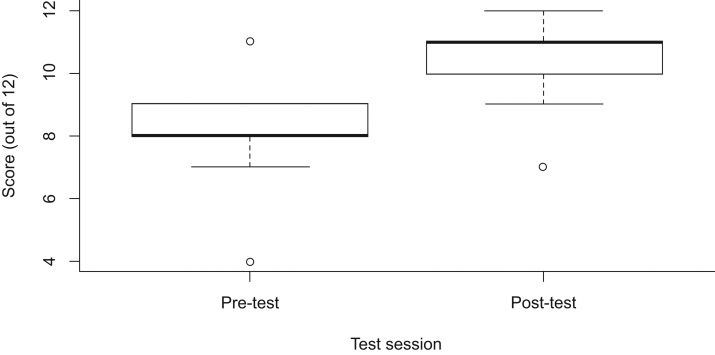
All learners completed the cognitive pre- and posttests, as well as the course evaluation and task trainer feedback forms. Prior to beginning the educational session, average cognitive pretest scores were 8.3 out of 12. Upon completion of the didactic component, average cognitive posttest scores were 10.2 out of 12. The mean cognitive posttest score significantly improved by 15.0% compared to pretest scores (p = .002). No learner scored worse on the cognitive posttest, and 77.8% of learners demonstrated improvement on the cognitive posttest (Figure).
Figure. Boxplot of cognitive pre- and posttest scores before and after the simulation curriculum. Boxes represent the interquartile range for each test, with the lower edge of the box representing the 25th percentile and the upper edge of the box representing the 75th percentile; error bars represent the maximum and minimum values for each test. Dark lines within each box represent the median value for each group. Open circles represent outliers. Cognitive posttest scores improved by 15% on average from pretest baseline (p = .002). Average pretest score was 8.3 out of 12, and average posttest score was 10.2.
On average, participants rated the didactic portion 3.78 out of 4 and the simulation portion 3.11 out of 4 with regard to usefulness in education. The overall course improved confidence in managing acute ischemic priapism either somewhat or very much from baseline among 88.9% of participants, with an average rating of 3.44 out of 4. Specific feedback comments indicated that those trainees who were PGY3/U2 or PGY4/U2 found the curriculum less useful, as many of them had already managed patients with acute ischemic priapism in clinical training.
The simulator also appeared to have reasonable scores for fidelity and perceived utility. On average, the simulator was rated 4.78 out of 5 for ease of use and 4.00 out of 5 for demonstration of relevant anatomic structures. Average rating for adequate simulation of the stepwise management of acute ischemic priapism was 3.40 out of 5. Of participants, 77.8% recommended the simulator's incorporation into resident training (average rating: 4.00 out of 5), and the same proportion felt this to be appropriate training before performing actual corporal aspiration, irrigation, or injection on a real patient (average rating: 4.00 out of 5).
Discussion
The task trainer and accompanying didactic accomplished our initial goals of a low-cost simulation-based educational curriculum that could be easily reproduced and adapted for urologic and nonurologic trainees at other institutions, as it cost significantly less per model than what has been described in the literature ($1.25 vs. $70-$120) and required about a quarter of the assembly time.9 Moreover, even among a cohort of junior urology residents, most of whom had already had prior clinical experience with priapism management, over 75% demonstrated improvement in cognitive test scores following completion of the curriculum, and nearly 90% improved their confidence in managing this entity. Over 75% felt that the task trainer was appropriate training prior to a real patient interaction, and the same proportion recommended its incorporation into resident training.
Though sophisticated simulators are available for a variety of urologic procedures, there remain no published task trainers for acute ischemic priapism, with most trainees receiving trial-by-fire learning in actual clinical patient encounters. This may be particularly stressful for providers who have not had such clinical experience but find themselves the primary providers for these patients. One potential solution to this lies in simulation. While there has been a call for greater adoption of simulation-based education, one of the significant barriers remains the high cost of simulation platforms and the paucity of well-validated, low-cost, low-fidelity trainers.8 This is particularly notable, given prior evidence that low-fidelity task trainers appear to perform similarly to higher fidelity models among less experienced learners.12 Our curriculum and task trainer address this need and may be potentially adapted and used across a wide spectrum of training settings. The affordability of the task trainer, as well as the minimal setup time and low time commitment (80 minutes) of the entire educational session, may facilitate its utilization and scale to larger cohorts of trainees, particularly in training settings that are more resource limited.
One significant challenge in developing the task trainer was balancing the need for cost containment and scalability with the desire for a higher fidelity model to maximize educational impact. We therefore anticipated that our model would potentially have more limited evidence for face or content validity than a higher fidelity model; this was indeed reflected in the feedback scores. Regardless, the cohort of learners with whom we piloted our curriculum demonstrated an overall improvement in self-reported confidence in priapism management compared to baseline and felt the simulation to be useful, suggesting that this lower fidelity task trainer was an effective educational tool.
Another challenge was generating didactic content general enough to be relevant for EM and other nonurologic trainees but sufficiently advanced to be useful to urology trainees who may have more prior knowledge and experience in priapism management. In order to maintain the generalizability of this resource, we intentionally focused more on the general principles of priapism management in the didactic session, while keeping the didactic guideline-based and highlighting more subtle nuances that might be considered more useful to urology learners. Aditionally, we intentionally designed the didactic to be presented in an interactive format in order to allow tailoring of the didactic discussion to the background and experience level of the individual learners. The overall improvement in cognitive posttest scores suggests that this approach was successful, as even experienced urology trainees demonstrated improvement in test scores after completion of the session.
A limitation of the study is that all participating residents were recruited from a urology residency training program at a single institution. This limits the generalizability of these results, particularly to residents of other training programs, such as EM, who were identified as potential learners for this curriculum. Moreover, the small total sample size of the study and small-group sizes for each session may have introduced bias into the results, in that there was limited anonymity in the evaluated responses of the learners. To mitigate this effect, all responses were anonymous and scored in aggregate upon completion of all educational sessions by a blinded reviewer. Despite these limitations, we were able to demonstrate a positive effect of the simulation curriculum on cognitive test scores and self-confidence even among urology residents who had prior knowledge and experience with priapism management. Among a cohort of less experienced trainees, such as those in other training programs, we hypothesize that an even greater improvement in both domains would be expected. Future opportunities to pilot this curriculum among a cohort of EM residents would further demonstrate its utility and generalizability to the full range of the target audience.
We believe that this low-cost simulation-based curriculum could be easily incorporated into educational curricula in a variety of training settings and would be valuable to both urologic and nonurologic trainees. Though low-fidelity simulators alone are insufficient to substitute for clinical learning, use of such task trainers among inexperienced trainees may optimize preparedness for clinical care by improving knowledge and confidence in priapism management. Future work is warranted to further evaluate the impact of this curriculum among EM trainees and validate the utility of this model in a larger range of training settings.
Appendices
A. Priapism Didactic Presentation.pptx
B. Simulation Setup.docx
C. Pre- and Posttest.docx
D. Guide for Informed Consent.docx
E. Stepwise Bedside Management of Acute Ischemic Priapism.docx
F. Simulation Checklist.docx
G. Curriculum Evaluation.docx
H. Simulation Evaluation Tool.docx
All appendices are peer reviewed as integral parts of the Original Publication.
Disclosures
None to report.
Funding/Support
None to report.
Prior Presentations
Some data included in this Educational Summary Report were submitted as an abstract to the American Urological Association and to the Council of Emergency Medicine Annual Meeting but have not yet been published.
Ethical Approval
University of Washington Human Subjects Division approved this study.
References
- 1.Montague DK, Jarow J, Broderick GA, et al. ; and Members of the Erectile Dysfunction Guideline Update Panel. American Urological Association guideline on the management of priapism. J Urol. 2003;170(4, pt 1):1318–1324. https://doi.org/10.1097/01.ju.0000087608.07371.ca [DOI] [PubMed] [Google Scholar]
- 2.Kulmala RV, Lehtonen TA, Tammela TLJ. Priapism, its incidence and seasonal distribution in Finland. Scand J Urol Nephrol. 1995;29(1):93–96. https://doi.org/10.3109/00365599509180545 [DOI] [PubMed] [Google Scholar]
- 3.Eland IA, van der Lei J, Stricker BHC, Sturkenboom MJCM. Incidence of priapism in the general population. Urology. 2001;57(5):970–972. https://doi.org/10.1016/S0090-4295(01)00941-4 [DOI] [PubMed] [Google Scholar]
- 4.Earle CM, Stuckey BGA, Ching HL, Wisniewski ZS. The incidence and management of priapism in Western Australia: a 16 year audit. Int J Impot Res. 2003;15:272–276. https://doi.org/10.1038/sj.ijir.3901018 [DOI] [PubMed] [Google Scholar]
- 5.Roghmann F, Becker A, Sammon JD, et al. Incidence of priapism in emergency departments in the United States. J Urol. 2013;190(4):1275–1280. https://doi.org/10.1016/j.juro.2013.03.118 [DOI] [PubMed] [Google Scholar]
- 6.Dai JC, Franzen DS, Lendvay TS, Walsh TJ. Experiences and attitudes toward priapism education in emergency medicine residency. Poster presented at: Council of Emergency Medicine Residency Directors 2018 Academic Assembly, Advances in Education Research and Innovations Forum; April 22–25, 2018; San Antonio, TX.
- 7.Dawe SR, Pena GN, Windsor JA, et al. Systematic review of skills transfer after surgical simulation-based training. Br J Surg. 2014;101(9):1063–1076. https://doi.org/10.1002/bjs.9482 [DOI] [PubMed] [Google Scholar]
- 8.Aydin A, Shafi AMA, Khan MS, Dasgupta P, Ahmed K. Current status of simulation and training models in urological surgery: a systematic review. J Urol. 2016;196(2):312–320. https://doi.org/10.1016/j.juro.2016.01.131 [DOI] [PubMed] [Google Scholar]
- 9.Ruest AS, Getto LP, Fredette JM, Cherico A, Papas MA, Nomura JT. A novel task trainer for penile corpus cavernosa aspiration [Research Forum abstract 327]. Ann Emerg Med. 2016;68(4)(suppl):S126 https://doi.org/10.1016/j.annemergmed.2016.08.343 [DOI] [PubMed] [Google Scholar]
- 10.Lendvay T, Hidalgo-Tamola J, Sherman M, Kim S. Percutaneous suprapubic tube catheter placement. MedEdPORTAL. 2010;6:8000 https://doi.org/10.15766/mep_2374-8265.8000 [Google Scholar]
- 11.Stickrath E, Alston M. A novel abdominal hysterectomy simulator and its impact on obstetrics and gynecology residents' surgical confidence. MedEdPORTAL. 2017;13:10636 https://doi.org/10.15766/mep_2374-8265.10636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Anastakis DJ, Regehr G, Reznick RK, et al. Assessment of technical skills transfer from the bench training model to the human model. Am J Surg. 1999;177(2):167–170. https://doi.org/10.1016/S0002-9610(98)00327-4 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A. Priapism Didactic Presentation.pptx
B. Simulation Setup.docx
C. Pre- and Posttest.docx
D. Guide for Informed Consent.docx
E. Stepwise Bedside Management of Acute Ischemic Priapism.docx
F. Simulation Checklist.docx
G. Curriculum Evaluation.docx
H. Simulation Evaluation Tool.docx
All appendices are peer reviewed as integral parts of the Original Publication.