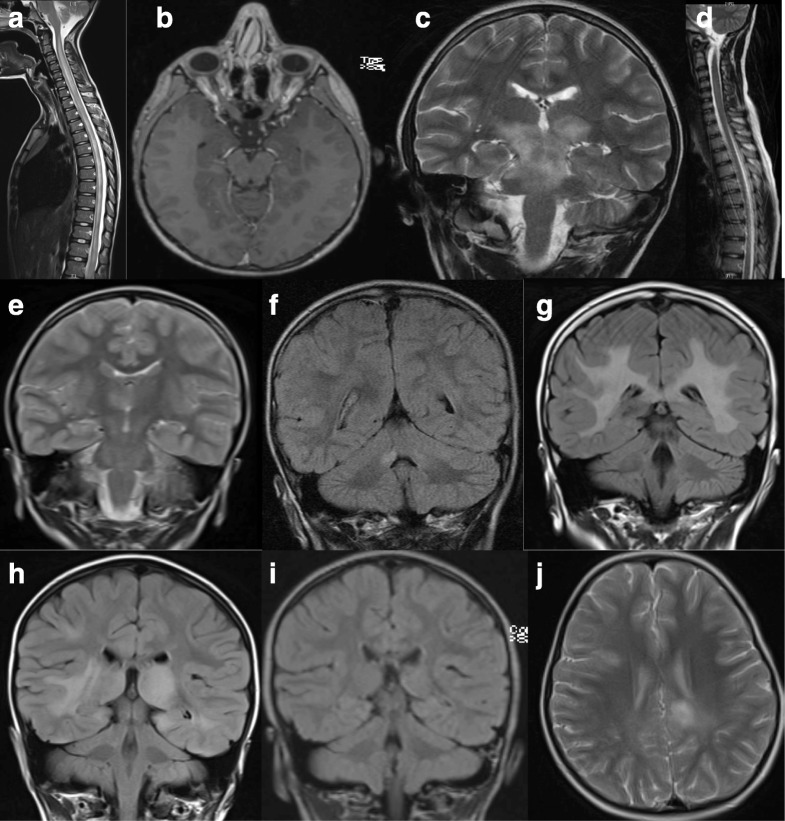
Fig. 1.
MRI findings in children with MOG-Ab-associated disease. A 10-year-old boy presented with encephalopathy, limb weakness (but able to walk), bilateral optic neuritis with only light perception, and urinary incontinence. MRI revealed longitudinally extensive transverse myelitis (a) and bilateral optic neuritis with enhancement (b). He relapsed 4 months later with headaches, fever, and encephalopathy. MRI revealed confluent lesions involving the pons, midbrain, and the superior cerebellar peduncles (c) as well as the left frontal opercular cortex. The previous spinal lesion has significantly improved (d). A 4-year-old girl presented with encephalopathy, seizures, and lethargy progressed to weakness of her right arm and bilateral 6th nerve palsies. MRI demonstrated a focus of signal change in the right thalamus (e). She relapsed 4 months later with brainstem cerebellar syndrome and lesions in both middle cerebellar peduncles (f) as well as a new lesion in the left side of the midbrain (not shown). At 4 years of age, she presented with bilateral optic neuritis. MRI showed diffuse bilateral white matter signal abnormality involving the cortical and subcortical regions extending inferiorly along the cerebral peduncles, pons, and right middle cerebellar peduncle, as well as swelling and signal abnormality of the corpus callosum (g). She had a further episode of bilateral optic neuritis 1 year later. A 4-year-old girl presented with encephalopathy, headache, and lethargy and MRI findings revealed diffuse bilateral and asymmetric signal abnormalities of the basal ganglia and thalamus with similar non-enhancing disease of the cortex, subcortical and deep white matter of both hemispheres (h). Repeat imaging 3 months later demonstrated near complete resolution of all lesions, concurrent with clinical recovery. She relapsed 15 months later with new onset headaches, encephalopathy characterized by behavioral change with hallucinations and confusion, and MRI evidence of new cortical and juxtacortical T2 lesions (j).