Abstract
Background.
African American (AA) women perform low levels of physical activity (PA) and are disproportionally burdened by cardiometabolic disease conditions when compared to White women and the U.S. population as a whole. These disparities emphasize the need for innovative and effective interventions to increase PA and reduce cardiometabolic disease risk among AA women. Recent evidence suggests that mobile health (mHealth) interventions have the potential to increase PA and reduce cardiometabolic disease risk factors. Few studies have examined the efficacy of mHealth PA interventions among racial/ethnic minorities, including AA women. This represents a missed opportunity given the reported success of technology-delivered PA interventions in predominately White populations and the high use of technology among AA women.
Objective.
To describe the design, theoretical rationale, and cultural relevance of Smart Walk, a culturally sensitive smartphone-delivered PA intervention for AA women.
Design and Methods.
Smart Walk is an 8-month, randomized controlled pilot trial designed to increase PA and reduce cardiometabolic disease risk among AA women. Sixty physically inactive AA women with obesity will be assigned to receive either a culturally relevant intervention designed to increase PA (by targeting leisure-time, household chore/task-related, and occupational PA) or a culturally relevant wellness attention-matched control condition. Outcomes will be assessed at baseline, 4 months, and 8 months, and include feasibility and acceptability of the PA intervention and evaluation of effects on PA and cardiometabolic risk factors.
Summary.
Smart Walk represents a culturally relevant, theory-based approach to promote PA and reduce cardiometabolic disease risk in AA women.
Keywords: eHealth, mHealth, exercise, minority health, cardiometabolic health, interventions
1. INTRODUCTION
Cardiometabolic disease conditions are a major public health concern for African American (AA) women. National prevalence data indicate that 57% of AA women are obese (BMI>30 kg m2) [1], 48% have cardiovascular disease [2], and 15% have diagnosed diabetes mellitus (with type 2 diabetes accounting for 90-95% of all cases) [2]. The prevalence of these conditions are substantially higher than those observed in White women (of whom 33% are obese, 32% have cardiovascular disease, and 6% have diabetes) and the U.S. population as a whole (35% are obese, 35% have cardiovascular disease, and 10% have diabetes). Physical activity (PA) improves weight control [3, 4] and myriad risk factors implicated in cardiometabolic disease [5], including high blood pressure [6, 7], poor serum lipid profiles [7–9], insulin resistance [7, 10, 11], glucose intolerance [12, 13], elevated HbA1c [14, 15], low cardiorespiratory fitness [16–19], poor aortic pulse wave velocity [20–22], and pro-inflammation biomarkers (i.e., TNF-α, IL-β1) [19]. Despite its benefits, AA women engage in PA at levels well below national recommendations (i.e., 150 minutes/week of moderate-intensity PA, 75 minutes of vigorous PA, or an equivalent combination of durations and intensities [23, 24]). Recent self-report data from three national surveys (i.e., 2015 BRFSS, 2011-2014 NHANES, and 2014 NHIS) [25] indicated that only 27% to 40% of AA met national PA guidelines. Objectively-measured PA estimates from 2003-2004 NHANES [26] and other large cohort studies (i.e., REGARDS [27] and CARDIA [28]) reflect similar trends.
Emerging evidence suggests that mobile health (mHealth) interventions, defined as interventions delivered using mobile computing and communication technologies (i.e., mobile phones, smartphones, wearable sensors) [29, 30], have the potential to increase PA [30–34] and improve risk factors associated with cardiometabolic disease [34]. Few studies, however, have explored the efficacy of mHealth PA interventions among AA women. Another shortcoming in the PA promotion research among AA women is the lack of clear attention to cultural relevance. For example, a 2014 review of PA interventions targeting AAs [35] reported that only 7 of the 16 interventions reviewed were culturally tailored at a “deep structure” level, and only 5 of these 7 focused exclusively on AA women. Other reviews on this topic have reported similar outcomes [36, 37]. “Deep structure” cultural tailoring involves recognizing a group’s cultural values, social norms, beliefs, and behaviors, and leveraging these aspects to promote behavior change [38]. Culturally tailoring at a “deep” level is believed to enhance the acceptability and uptake of an intervention, which may lead to positive changes in targeted behaviors [38–40].
To address the low PA levels, high cardiometabolic disease burden, and shortcomings in the current PA promotion literature among AA women, we designed Smart Walk, a culturally relevant, theory-based smartphone-delivered intervention designed to increase PA and reduce cardiometabolic disease risk among AA women. The purpose of this report is to describe the study design, theoretical rationale, and cultural relevance of the Smart Walk intervention.
2. METHODS
This study is funded by the National Institute of Health/National Heart, Lung, and Blood Institute (NIH/NHLBI), awards K99HL129012 and R00HL129012, Smart Walk: A Physical Activity Program for African American Women. The study protocol was approved by the Arizona State University Institutional Review Board and is registered at www.clinicaltrials.gov (Identifier: NCT02823379).
2.1. Study Aim
The aim of this study is to conduct a preliminary evaluation of Smart Walk, an 8-month, culturally relevant, Social Cognitive Theory (SCT)-based smartphone-delivered PA intervention, to improve and maintain high PA levels and reduce cardiometabolic disease risk among obese AA women. Specifically, we will: a) establish the feasibility and acceptability of delivering a PA program via a smartphone application to physically inactive AA women with obesity, and b) assess the effects of Smart Walkto improve (baseline to 4 months) and maintain (5 to 8 months) PA and reduce cardiometabolic risk factors among obese AA women relative to an attention-matched control group. Feasibility, acceptability, and treatment receipt will be assessed by examining recruitment, retention, adherence, treatment acceptance, enactment of behavior change techniques presented in intervention, and data on participant utilization of a Smartphone application as recorded by analytic tracking software. Intervention effects on cardiometabolic risk factors in response to the PA intervention will be assessed by the following: waist circumference, BMI, cardiorespiratory fitness, blood pressure, serum lipid profiles, glucose intolerance, insulin resistance, aortic pulse wave velocity, and pro-inflammation biomarkers implicated in cardiovascular disease and type 2 diabetes (TNF-α, IL-β1). We hypothesize that the culturally relevant Smartphone-delivered PA program will lead to greater improvements in PA and critical health outcomes associated with cardiometabolic disease than an attention-matched control group.
2.2. Study Design
An 8-month, two-parallel arm, randomized controlled study design will be implemented. Participants will receive either a smartphone-delivered SCT-based culturally relevant PA promotion intervention or smartphone-delivered culturally relevant attention-matched wellness control condition. Months 1-4 will be the active intervention phase. Months 5-8 will consist of a no-contact maintenance period. During the 4-month maintenance period, participants will have access to their condition-specific smartphone applications and all previously delivered intervention materials, but no new content will be delivered. The final follow-up assessment will occur at 8 months to allow for evaluation of longer-term effects of the intervention on PA and cardiometabolic disease risk factors. The 4-month duration of the active intervention phase provides sufficient time for participants to increase their PA levels [41, 42] and experience subsequent improvements in cardiometabolic riskfactors [19, 43].
2.3. Setting
The setting of the study is the greater metropolitan area of Phoenix, Arizona, USA, where AAs account for 7% of the population [44]. State-level PA data from the 2015 Behavioral Risk Factors Surveillance Survey (BRFSS) show that 43% of AA women in Arizona achieve the national PA guidelines, which is substantially lower than rates among White and Hispanic women residing in the state (58% and 49%, respectively) [45]. Likewise, AAs of both genders in Arizona have higher rates of obesity, diabetes, hypertension, hyperlipidemia, and stroke than White residents [46]. Mortality rates for cardiovascular disease among AA women in Arizona are 27.6% and 34.7% higher than the rates for Hispanic and White women, respectively.
2.4. Sample
The study will recruit 60 AA women with obesity (BMI ≥ 30 kg m2), aged 24-49, who report performing less than 60 minutes of moderate-to-vigorous PA (MVPA) per week. The selected age range focuses tailoring of the intervention to the social, cultural, and behavioral characteristics of young to middle-aged adult AA women who, among all AA women, are the most likely to own smartphones [47]. Women are eligible to participate if they: a) self-identify as AA; b) are aged 24 to 49 years; c) have a BMI ≥30 kg m2 d) have insufficient levels of PA, defined as performing <60 minutes/week of MVPA according to the 2-item Exercise Vital Sign questionnaire, which has been previously validated against accelerometers for assessment of PA among AA women [48]; and e) have the ability to speak and read English. Exclusion criteria include: a) concurrent participation in another PA, nutrition, or weight loss program at time of enrollment or any time during the 8-month study; b) indication of a potential contraindication of exercise according to the 2015 Physical Activity Readiness Questionnaire (PAR-Q+) [49], unless a written permission from the potential participant’s primary care physician is provided; c) pregnant at time of screening or plans to become pregnant in the next 8 months; and d) plans to relocate out of the Phoenix metropolitan area in the next 12 months.
2.5. SMART WALK INTERVENTION
2.5.1. Behavioral Target
The overall behavioral goal of the intervention is for participants to perform at least 150 minutes per week of moderate-intensity aerobic PA, achieved through all daily activities, including household, occupational, and leisure-time activities. This goal coincides with the 2008 and 2018 national PA guidelines for aerobic PA for the reduction of chronic disease risk [23, 24]. Walking is emphasized as a primary activity to achieve this PA goal because it was identified as the preferred mode for AA women to achieve PA guidelines during our formative research [50]. Further, walking requires no specialized equipment and can be done in most locations. In addition to walking, intervention materials judiciously encourage participants to try other types of aerobic activities (i.e., group-based aerobic classes, bicycle riding, and recreational activities like hiking and gardening). These activities are included to expose participants to different types of aerobic PA that can be performed to meet the national PA guidelines and to encourage them to try activities they may not normally consider.
2.5.2. Intervention Model
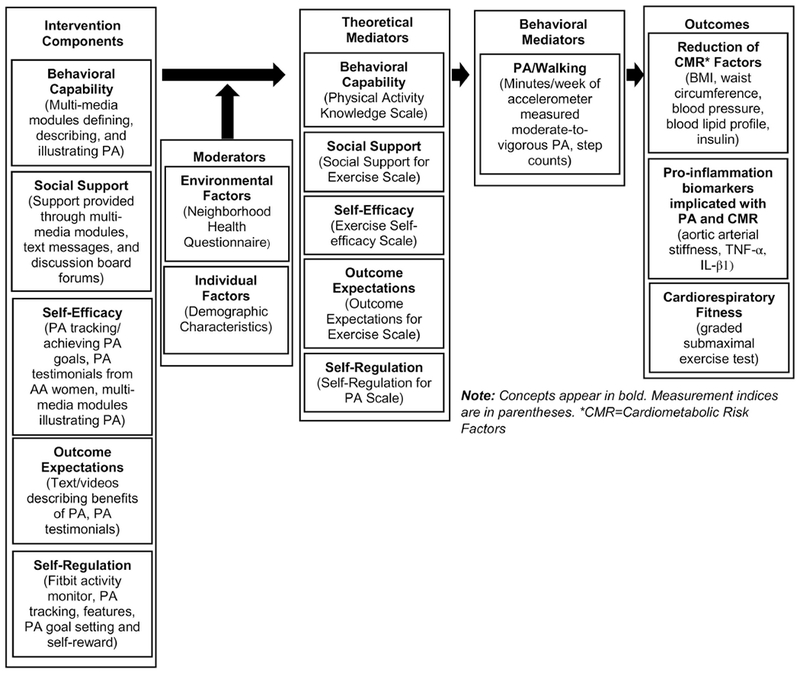
Figure 1 illustrates the intervention model guiding study activities. This model illustrates the hypothesized mechanisms through which the culturally relevant intervention leverages constructs of SCT to increase PA and reduce cardiometabolic disease risk. Two moderators, five theoretical mediators, one behavioral mediator, and one confounding variable are considered. Environmental factors of neighborhood safety, walking environment, aesthetics, traffic, and social cohesion and participant demographic characteristics are hypothesized to moderate the effects of the PA intervention. Hypothesized mediators include the five SCT constructs targeted by intervention activities and the level of PA engagement over the duration of the study. Dietary intake will serve as a potential covariate in outcome analyses. In-depth descriptions of the elements of the model are presented below.
Figure 1. Smart Walk intervention model.
2.5.3. Description of the Smart Walk Smartphone-delivered PA Program
The Smart Walk smartphone application includes four key features: 1) personal profile pages, 2) culturally relevant multi-media (i.e., text and video) PA promotion modules, 3) message/discussion boards, and 4) PA self-monitoring/tracking tools for participants to track their daily activity. In addition to the smartphone application-delivered content, participants will also receive three PA promotion text messages each week for the duration of the active 4-month intervention. Screenshots of these features are illustrated in Figures 2 and 3. An in-depth description of each of these components is presented below.
Figure 2. Screenshots of the Smart Walk smartphone application.
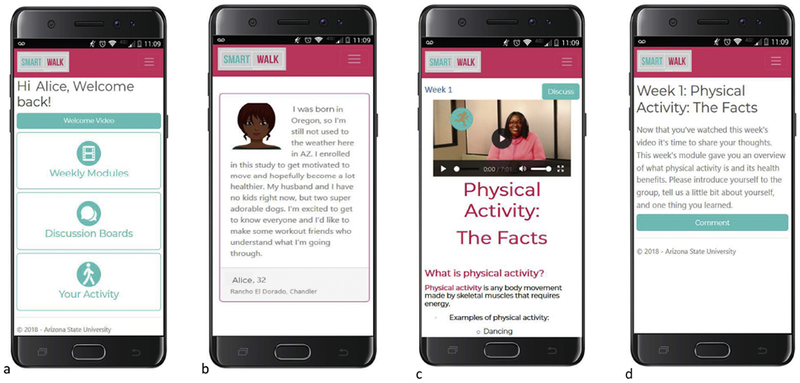
(a) Home screen. (b) Example personal profile page, (c) Example multi-media module, (d) Example discussion board prompt.
Figure 3. Screenshots of the Smart Walk PA tracker/self-monitoring tool.
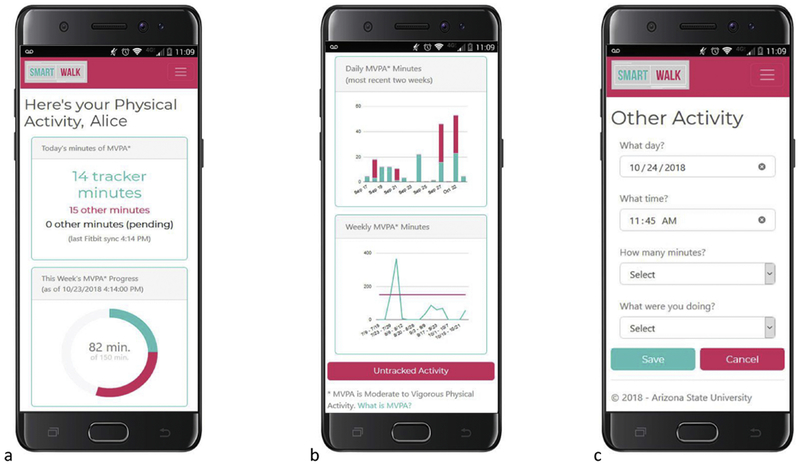
(a) Upper box: Illustration of how daily minutes of MVPA are displayed in the activity tracker; Lower box: Illustration of donut graph used to show progress towards the weekly goal of 150 minutes of at least moderate-intensity PA. (b) Upper graph: Illustration how daily minutes of MVPA are displayed over a period of 2 weeks; Lower graph: Illustration of weekly PA levels over a 4 week period, pink line represents 150 minutes of MVPA. (c) Illustration of how non-Fitbit measured MVPA is entered into the tracking feature.
Personal Profile Pages.
Each participant will have a personal profile page on the Smart Walkapp. This feature, similarto the profile pages on commercially available social media websites (i.e., Facebook, Twitter), allows participants to share select biographical information with other study participants. Fields available for participants to complete on this page include a) name, b) age, c) neighborhood/local area in which they reside, and d) brief biographical narrative (i.e., 250 characters or less). Participants can also uploaded an image or picture they would associated with their personal profile. All fields on the personal profile page are optional for participants to complete, with the exception of participant name (which can be their first name or an alias they would like to use for the study). This feature was designed to help foster a sense of community and personal connection among study participants.
Multi-media culturally-relevant PA promotion modules.
The primary delivery channel for the educational and behavioral components of the program is through weekly multimedia text and video modules delivered through the Smart Walk application. Each module consists of text- and image-based PA promotion materials written at < 8th grade reading level and is accompanied by a brief 3-7 min video, narrated by the study’s AA spokesperson, that further describes, and when applicable, demonstrates the information presented in the text-based materials. A screenshot of one of these modules is presented in Figure 2. These multi-media PA promotion materials were developed through an extensive review of the PA promotion literature [51, 52] and our formative research with AA women [50, 53]. During the first 3 months, new PA promotion modules will be delivered weekly. For month 4, new modules will be presented every two weeks and focus on maintenance of PA after the active intervention phase. Table 1 illustrates the module topics for the PA promotion program and corresponding SCT constructs targeted by each module (see section 2.5.4 for an in-depth description of the theoretical rationale for the program).
Table 1.
Weekly module topics by study group.
| Physical Activity Study Arm | Wellness Attention-match Control Arm | |||
|---|---|---|---|---|
| Week Number | Module Number | Module Topic | SCT Constructs Targeted | Module Topic |
| 1 | 1 | Introduction to the national PA guidelines and the health benefits of PA | • Behavioral capability • Outcome expectations • Self-regulation |
Sunscreen and Skin Care |
| 2 | 2 | Overview of PA-related health disparities among AA women and the importance of being a PA role model | • Outcome expectations • Self-regulation |
Hydration and Water Consumption |
| 3 | 3 | Time management and strategies for incorporating 30 minutes of PA into the day | • Self-efficacy • Self-regulation • Behavioral Capability |
Heat illness: causes, symptoms, and prevention |
| 4 | 4 | PA goal setting | • Self-efficacy • Self-regulation |
Discussing your health with your Doctor |
| 5 | 5 | Overcoming general barriers to PA | • Self-efficacy | Breast Cancer Prevention and Screening |
| 6 | 6 | Tips for increasing daily PA | • Self-regulation • Behavioral Capability |
Cervical Cancer Prevention and Screening |
| 7 | 7 | Overcoming hair care barriers to PA | • Behavioral capability • Self-regulation • Self-efficacy |
Hair Care |
| 8 | 8 | Creating a social support network for PA | • Social Support • Self-regulation |
Oral Health |
| 9 | 9 | Trying new types of activities | • Behavioral capability | Eye Health |
| 10 | 10 | Reducing sedentary time | • Behavioral capability | Sickle Cell Disease |
| 11 | 11 | Dietary behaviors to complement PA | • Behavioral capability | Stress Management |
| 12 | 12 | Muscle strengthening and stretching activities to complement aerobic PA | • Self-regulation | Preventing the Spread of the Cold/Flu |
| 13 | N/A | No weekly module | ||
| 14 | 13 | Dealing with setbacks. | • Self-efficacy • Outcome expectations |
Staying Healthy when Travelling |
| 15 | N/A | No weekly module | ||
| 16 | 14 | Review of previous modules and maintenance of PA after the active intervention phase | • Self-regulation • Behavioral Capability |
Review of Previous Modules |
Abbreviation: PA = physical activity.
Discussion/Message Boards.
Each of the weekly PA promotion modules is accompanied with a message board/discussion forum topic for participants to reflect on the information presented in the PA promotion modules, share their personal experiences about PA, and to give/receive social support for PA. The discussion board feature also includes a general “Community Board” forum, where participants share information and/or discuss topics that may not clearly align with the weekly module topics. Dialogue among participants during these discussions is a primary mechanism through which social support for PA is fostered among participants. To help facilitate discussions, push notifications will be sent to study participants when other participants post in the discussion boards. Example module discussion board topics include: “Why do you want to be physically active?” and “What are ways you add more physical activity into your day?” A screenshot of a discussion board forum is provided in Figure 2.
PA Self-monitoring/Goal Setting Feature.
The Smart Walk application includes an interactive self-monitoring and goal setting component. This feature provides a static weekly goal of 150 minutes per week of moderate-intensity aerobic PA or greater for participants to achieve and allows participants to track their activity on daily and weekly levels through interactive graphing functions (see Figure 3). Participants will be provided a Fitbit Alta HR activity monitor to wear throughout the study. The Fitbit Alta HR (Fitbit Inc., San Francisco CA) is a wrist-worn activity monitor that assesses heart rate, steps, distance travelled, and time and intensity of activity preformed. Data collected from the Fitbit integrates with the Smart Walk application to allow participants to view/track the minutes of MVPA performed during the study. The criterion used to define MVPA as measured by the Fitbit will be a walking cadence 100 steps/minute. This criterion was selected because it has been widely established as a cadence corresponding to at least moderate-intensity walking [54, 55]. All Fitbit devices will be registered to a research study account. At the baseline assessment, study staff will: a) disable commercial Fitbit software notifications/prompts when installing the Smart Walk application on participants’ mobile phones, and b) configure the wrist-worn Fitbit device display to show only time of day, daily distance travelled, and battery life. This steps are designed to minimize confounding factors introduced by the commercial Fitbit software and device display. Participants will be informed not to view the commercial Fitbit app or enable Fitbit notifications/prompts during the intervention and follow up phases. Study staff will periodically audit study Fitbit accounts and follow up study participants as needed to ensure compliance.
In addition to using the Fitbit to monitor PA levels, the Smart Walk activity tracker includes an option for participants to manually enter specific types of aerobic MVPA that are not accurately measured by the wrist-worn Fitbit device. To do this, participants select from a limited number of pre-defined activities and enter the duration of time they performed the specified activity. Activities included in the pre-defined list include: aerobics/Zumba, cycling, stationary bike, elliptical trainer, and rowing. Activities not included on the pre-defined list may still be entered by participants under a category labeled as “other”, but this option requires participants to specify the type of activity performed and a member of the study team to review and approve (or reject) the activity before it will included in the participant’s weekly MVPA totals. If the activity is rejected, the team member will enter a note explaining the decision, which will be visible to the user. When non-aerobic MVPA activities are entered, a member of the research team will contact the participant and discuss the reason why the activity does not constitute aerobic MVPA. Notably, participants are not able to manually enter walking or jogging activities into the activity tracker. Allowing this would disincentive participants from wearing the Fitbit activity monitor and introduce unnecessary self-report bias into the objective measurement of walking/jogging activities (which are what the primary MVPA targets of the intervention). The option to manually enter specific modes of MVPA was included because our pilot tests showed the several participants were engaging various forms of MVPA that were not being recorded by the Fitbit device (i.e., group cycling classes, exercising on the Elliptical cross-training machine). This resulted in a negative user experience and limited enthusiasm regarding the usability and functionality of the Smart Walk tracking feature.
Motivational Text Messages.
Participants will receive 3 PA-related text messages each week during the 4-month intervention phase. These antecedent messages will serve as an additional source of social support. These messages target SCT constructs of outcome expectations, self-efficacy, and behavioral capability by providing: (a) tips/strategies to increase PA throughout the day (behavioral capability, self-regulation), (b) strategies to overcome barriers to PA (self-efficacy, self-regulation), (c) health benefits of PA (outcome expectations), and (d) motivational quotes (self-efficacy). Message content and frequency are derived from previous work [50, 56, 57]. Example text messages include: “Commit to being fit. It’s never too late to achieve your physical activity goals.” and ‘“Each person must live their life as a model to others.” – Rosa Parks. “Be an active role model to those around you!”
2.5.4. Theoretical Rationale
Associations posited under Social Cognitive Theory (SCT) constitute the theoretical underpinning of the Smart Walk intervention. SCT is an interpersonal behavioral theory that explains behavior using a dynamic and reciprocal model in which intrapersonal factors (beliefs and attitudes), the social and physical environments, and behavioral factors interact [58]. SCT was selected as the theoretical approach for the intervention because it places a particular focus on how individuals can construct their social environments to facilitate engagement of a given behavior [59]. Given PA is largely influenced by an individual’s perceived control over their own behaviors, as well as their social environment, SCT provided a meaningful framework to underpin intervention activities. Additionally, SCT includes several evidence-based PA promotion constructs (i.e., self-regulation, self-efficacy, and social support) [60–62] that were deployed in the cultural tailoring of Smart Walk designed to address deeply-rooted aspects of AA culture (i.e., collectivism/ethic of care, racial pride/role modelling, experiential knowledge) [50].
Theoretical fidelity [63] of the intervention was informed through review of the literature and formative research with our intended population. This formative work [50] was conducted using focus group methodology and collected empirically-driven data from AA women on their perceptions, manifestations, and determinants of PA to explicate how constructs of SCT can be culturally tailored in design of the PA intervention. Based on this work, intervention activities were designed to leverage five SCT constructs: 1) behavioral capability—knowledge and skill to perform a given behavior, 2) social support—extent to which significant referents approve, encourage, and/or influence performance of a behavior, 3) self-efficacy—confidence in oneself to take action and overcome barriers, 4) outcome expectations—anticipated outcomes of a behavior, and 5) self-regulation—ability to manage one’s own social, cognitive, and motivational processes in order to perform a behavior to achieve a desired goal. Table 2 provides an overview of how the Smart Walk intervention leverages these theoretical constructs.
Table 2.
Overview of Social Cognitive Theory Constructsa addressed by the PA intervention.
| Theoretical Construct | Operational Definition | Critical Inputs Targeted by the PA Intervention | How intervention components leveraged the theoretical construct |
|---|---|---|---|
| Behavioral Capability | Knowledge and skill to perform a PA | • Knowledge • Skill |
• Multi-media modules provide information on: o The definitions of PA and exercise PA o Different types of PA (i.e., aerobic vs. muscle strengthening) o The national PA guidelines o Modes and types of PA that can be performed to achieve the guidelines (i.e., walking, cycling, dance, gym activities) o How to determine the intensity of PA performed |
| Social Support | Extent to which significant referents approve, encourage, and/or influence performance of PA | • Emotional Support (i.e., expressions of empathy, trust and caring) | • Multi-media modules and text messages provide participants with messages of encouragement and empowerment for PA • Discussion board prompts facilitate and encourage participants to give and receive emotional support for PA |
| • Appraisal Support (i.e., information for self-evaluation) | • Multiple media modules: o Emphasize PA is a form of self-care and that AA women are worthy of self-care activities o Encourage participants to personally reflect on reasons why they should be physically active |
||
| • Informational Support (i.e., advice suggestions information) | • Multi-media modules and text messages provide: o Advice and tips on how to increase daily PA levels o Talking points and negotiations strategies on how to facilitate social support for PA from family and friends |
||
| Self-efficacy | Confidence in oneself to take action and overcome barriers | • Mastery Experience (i.e., first-hand experience with performing a behavior) | • Participants track PA using the activity tracking feature; allowing participants to enact PA strategies encouraged by the intervention and track their increases/decreases in PA |
| • Social Modeling (i.e., seeing other similar to ourselves successfully perform a behavior) | • Multi-media modules: o Illustrate AA women engaging in various types of aerobic PA o Include testimonials from AA women describing how and why they are physically active |
||
| • Verbal Persuasion (i.e., verbal encouragement to engage in a behavior) | • Multi-media modules and text messages encourage women to be active by providing words of encouragement and empowerment for PA • Discussion board forum prompts provide an environment where participants can encourage each other to be physically active |
||
| • Emotional Arousal/ (i.e., improving emotional states by reducing stress/anxiety and by promoting positive emotions) | • Multi-media modules reinforce the notion that PA doesn’t have to be structured or difficult by encouraging walking and providing tips on how more walking can be incorporated into the day | ||
| Outcome Expectations | Anticipated outcomes of engaging in PA | • Beliefs about the likelihood and value of the benefits and consequences of engaging in a behavior | • Weekly video and text modules provide participants with the health and social outcomes associated with being physically activity, including: o Reduced risk for heart disease and type 2 diabetes o Weight maintenance o More energy to perform daily activities o Improved quality and quantity (i.e., years) of life o Being a good role model to others |
| Self-regulation | Ability to manage one’s own social, cognitive, and motivational processes in order to engage in PA to achieve a desired goal | • Self-monitoring | • Use of the Fitbit and PA self-monitoring feature to track daily and weekly PA |
| • Goal Setting | • Intervention materials encouraged to achieve the static goal of 150 minutes per week of MVPA • Week 4 Module Topic encourages participants to create short and long-term goals associated with PA performance |
||
| • Self-reward | • Week 4 module encourages participants to create self-rewards for achieving previously established PA goals. |
Theoretical construct definitions and descriptions of critical inputs were adapted from text by Glanz et al. and Hayden.
Behavioral capability is addressed by providing participants with information designed to enhance PA-related knowledge and skill. Specifically, the multi-media modules and text messages provide information on a) the national PA guidelines; b) modes and types of PA that can meet the guidelines; and c) ways in which participants can measure the intensity of their PA such as the “talk test” (i.e., at a moderate intensity, individuals should be able to talk but not sing; at a vigorous intensity, individuals should not be able to say more than a few words without pausing to take a breath), heart rate monitors, and the Smart Walk application’s activity tracker feature.
Social support is targeted by the intervention activities leveraging three types of support: emotional, appraisal, and information. Emotional support (i.e., expressions of empathy, trust, and caring) is addressed through: a) multi-media modules and text messages providing participants with messages of encouragement and empowerment of PA and b) discussion board prompts facilitating discussions among participants to give and receive support for PA. Appraisal support (information for self-evaluation) is provided by the weekly modules emphasizing that PA is a form of self-care and by encouraging participants to critically examine and reflect on reasons why they should be physically activity. Informational support (i.e., advice, suggestions, and information) is targeted by providing participants with tips on how to increase daily PA and by providing talking points and negotiations strategies on how to facilitate a social support for PA among family and friends.
Strategies employed to enhance self-efficacy for PA focus on mastery experiences, social modeling, verbal persuasion, and emotional arousal. Mastery experiences are facilitated by allowing participants to use the Fitbit monitor and app activity tracker to monitor their PA while enacting the behavioral strategies outlined in the intervention materials to increase daily PA (i.e., taking three 10-minute walking breaks during the day, taking family walks after dinner). Participants who enact these strategies will observe increases in moderate-intensity PA, thus providing participants with the experiences needed to enhance PA self-efficacy. Social modeling is addressed in the multimedia modules by including images of AA women of diverse body sizes, ages, skin color, and hairstyles engaging in PA engaging in various types of PA (i.e., walking, gardening, hiking, exercise videos) and by including video testimonials from AA women on how they successfully incorporate more PA into their daily lives. Women depicted in these images and videos were carefully selected to exemplify the heterogeneity of physical appearances and life experiences of AA women; thus, increasing the likelihood of participants being able to visually relate to the women depicted in the images. Verbal persuasion and emotional arousal are leveraged by: a) multi-media modules and text messages providing words of encouragement and empowerment for PA, b) discussion board forums providing a venue for participants to give and receive encouragement for PA to each other, and c) intervention materials conveying that moderate-intensity PA does not have be difficult, complex, or performed in a manner that is uncomfortable or painful (i.e., moderate-intensity PA can be performed by brisk walking versus taking a boot camp or other type of class that requires complex movements and higher-intensity PA).
Outcome expectations are addressed by modules and text messages illustrating the health and social benefits of being physically active. Example benefits described in the intervention materials include: reduced risk for chronic disease, increased daily energy, weight management, improved mobility and quality of life as one ages, and being a role model to other AA women.
Self-regulation is leveraged in Smart Walk through self-monitoring, goal setting, and self-reward. The activity tracking feature and Fitbit monitor allow participants to self-monitor their PA on a daily, weekly and monthly level. Goal setting is leveraged by intervention materials encouraging participants to achieve a static goal 150 minutes/week of at least moderate intensity PA and by encouraging participants to develop more personalized short-term (i.e., walking at least 30 minutes each day for 5 days a week) and long-term (i.e., completing a 5k walk/run within the next year) PA goals. Lastly, participants are encouraged to create self-rewards (e.g., buying a new pair of shoes) for achieving their PA goals.
2.5.5. Cultural Relevance of Smart Walk
The Smart Walk intervention was designed to address sociocultural norms, beliefs, and behaviors related to PA engagement among AA women. Elements designed to enhance the cultural relevance of the intervention were derived from our previous PA intervention research with AA women [57, 64, 65], an extensive review of the PA promotion literature [51, 52], and our formative research assessments with AA women [50]. Together, these activities helped us identify key areas of emphasis for cultural tailoring.
We follow Resnicow et al.’s [38] framework by classifying cultural considerations used in tailoring the intervention as being at either the “surface” or “deep structure” level. Surface level cultural tailoring is the most basic level and involves matching the characteristics and packaging of a health promotion to the overt social and behavioral characteristics of the intended population [38]. This level of cultural tailoring is designed to enhance the perceived relevance and acceptance of a health promotion intervention [38]. Deep structure cultural tailoring involves recognizing a group’s cultural values, social norms, beliefs, and behaviors and leveraging these characteristics to motivate behavior change [38]. This level of cultural tailoring is the most difficult because it requires in-depth knowledge of deeply-rooted cultural, social, psychological, and historical factors that can influence PA among AA women [38]. The text below articulates the design strategies used to enhance the cultural relevance of Smart Walk.
2.5.5.1. Surface level cultural tailoring.
Surface-level cultural tailoring of the Smart Walk intervention is achieved by: a) use of data and statistics to communicate the current low levels of PA and high prevalence of cardiometabolic disease conditions among AA women to participants, b) inclusion of images of AA women performing PA throughout the text-based PA promotion materials, and c) having a local AA community member serve as the study spokesperson in the video modules. Statistics used in the intervention materials to highlight the low PA levels of AA women and the high cardiometabolic disease prevalence include: “Only 36% of AA women meet the National Physical Activity Guidelines of 150 minutes per week of moderate-to-vigorous intensity aerobic activity” [66]. “4 out of 5 AA women are overweight or obese” [1], and “Almost half (49%) of AA women over the age of 20 have heart disease” [2]. Images included in the PA promotion materials illustrate local AA women of varying ages and physical appearances (i.e., skin color, hairstyle, and body shape) engaging in PA. The video vignettes include with oral and visual presentations PA promotion materials given by a spokesperson who is also a local AA community member. The spokesperson was selected to deliver the PA program because she possesses several underlying characteristics that will likely resonate with participants, including being a local resident of the community, having a history of struggling with being physically active, and trying to find a work and family life balance that allows her to be physically active.
2.5.5.2. Deep structure cultural tailoring.
Three areas of emphasis were selected for deep structure cultural tailoring efforts: a) collectivism/ethic of care, b) physical appearance norms (i.e., hair care/body shape concerns), and c) racial pride/role modeling. The text below briefly describes these concepts and illustrates how each is addressed in the design of the intervention.
Collectivism.
Social and behavioral characteristics of many AA women have them place the needs of others, particularly those of their family and other close kinship-type relationships, before their own. Although this phenomenon has been reported by women of all cultural and ethnic backgrounds, it appears to be more emphasized in the value system of AA women [67, 68]. This prioritization often results in AA women reporting lack of time and energy to perform PA [51, 52]. Moreover, there is a belief among someAA that engaging in PA is self-serving that takes away valuable time from familial and community responsibilities [69, 70]. Intervention messages were designed to leverage the collectivistic perspective of AA women by: a) acknowledging the importance of family and community responsibilities among AA women; b) emphasizing that improved health (i.e., lower risk for chronic disease conditions ) resulting from PA allows AA women to perform their familial, occupational, and social roles with more energy and vigor throughout their lifetimes; and c) empowering participants to view PA as an investment in their own health, as well as the health of their families, as opposed “taking time away” from their families.
Physical Appearance Norms and Concerns.
Intervention activities are designed to address two primary PA-related physical appearance concerns among AA women: 1) hairstyle preferences/hair care maintenance, and b) body shape preferences. Extant research shows that many AA women are hesitant to engage in PA because perspiration can negatively influence their hairstyles [51, 52]. While this issue has been predominately reported among women with relaxed or chemically straightened hairstyles, our recent qualitative work [53] underscored that hair concerns are a salient issue for many AA women regardless of hairstyle (i.e., natural styles, wigs, braids). The time and money AA women invest into their hairstyles further compounds this issue [51, 52], as styling can take several hours, and salon visits can cost women several hundred dollars. The topic of hair was selected as a deep structure element for cultural tailoring because an AA woman’s hairstyle is often accompanied by complex feelings regarding social status, pressures to live up to normative White standards of beauty, cultural appropriation, and empowerment [53, 71–73]. Thus, for many AA women, their hairstyles represent much more than just a physical feature of their appearance. To address PA-related hair care barriers and concerns, our intervention materials are designed to: a) empower participants to adopt protective (i.e., braids, twist, locks), short, or natural styles that more conducive to being physically active, b) demonstrate styling techniques that negate the effects of sweating while being active such as the use of hair wraps, ponytails, and products that reduce the effect of sweating on hair, and c) illustrate time management and PA planning strategies that can help maximize the time between salon visits and time spent on daily styling.
In reference to body shape preferences, social norms in the AA comm unity often promote the acceptance of a larger, more full-figured body shape [74–76]. These norms can limit some AA women’s willingness to engage in PA due to the perception that PA will result in unwanted weight loss [52]. Conversely, weight loss can be a strong motivator for some AA women to be physically active. To address these nuanced concerns, intervention messages are carefully designed to inform participants that: a) engaging in PA at the levels recommended by the study will not substantially change their body shape unless they also change their dietary habits [3, 4], and b) to emphasize the health benefits of PA independent of weight loss (i.e., reduced cardiometabolic disease risk, weight maintenance, improved sleep, increased energy/stamina). Together these messages encourage participants to be more active regardless of participants’ perceptions of weight loss as desirable or undesirable.
Racial Pride/Role Modeling.
The extant literature shows that AA women have a vested interest in the health and well-being of the AA community [50, 51, 77]. Due to this interest, many AA women are mindful about how their actions contribute to the integrity and strength of the AA community. This community-centered focus, while closely related to collectivism, has been characterized as a dimension of racial or cultural pride [77, 78] and is a critical phenomenon leveraged in the current PA intervention. To address these perspectives, intervention messages and activities are designed to: a) foster an online community among participants through module topics and discussion boards focusing on reducing PA-related health disparities among AA women; b) emphasize that by being physically active, participants are collectively part of the solution to reduce cardiometabolic health disparities in AA women, as opposed to contributing the problem; and c) underscore PA as a positive role modeling behavior that encourages other AAs, particularly AA women and children, to be physically active.
2.6. WELLNESS ATTENTION-MATCHED CONTROL CONDITION
Participants in the attention-matched control condition will receive a health promotion intervention focused on important health topics and behaviors unrelated to PA and cardiometabolic disease risk (i.e., breast and cervical cancer prevention and screenings, skin care, and cold and flu prevention). This intervention, named Smart Health, will be delivered using the same smartphone application platform (i.e., written with the same codebase) as the PA intervention and will be delivered at the same time points; however, the wellness (attention control) condition does not include the PA monitoring/tracking tool available to the PA intervention participants. Table 3 compares the major study components between the two study arms. The weekly health and wellness promotion modules are culturally tailored at the “surface” level by: a) including relevant health statistics for AA based on the topic of the week, b) having the sameAA spokesperson deliver the video content of program as the PA arm, and c) using the sameAA models in the images included in the electronic text sections of the study modules as the PA intervention arm. Table 1 provides an overview of the health topics covered in this study arm Figures 4 provide screenshots of the Smart Health smartphone application.
Table 3.
Comparison of intervention components between study groups for the 4-month active intervention phase of the study.
| Intervention Component | Physical Activity Study Arm | Wellness Attention-matched Study Arm |
|---|---|---|
| Smartphone applications features | X | X |
| Personal profile pages | X | X |
| Weekly multi-media text and video modules | X | X |
| Discussion board forum with weekly discussion prompts | X | X |
| Physical activity tracker | X | |
| Text messages delivered 3 times per week | X | X |
Figure 4. Screenshots of the Smart Health smartphone application.
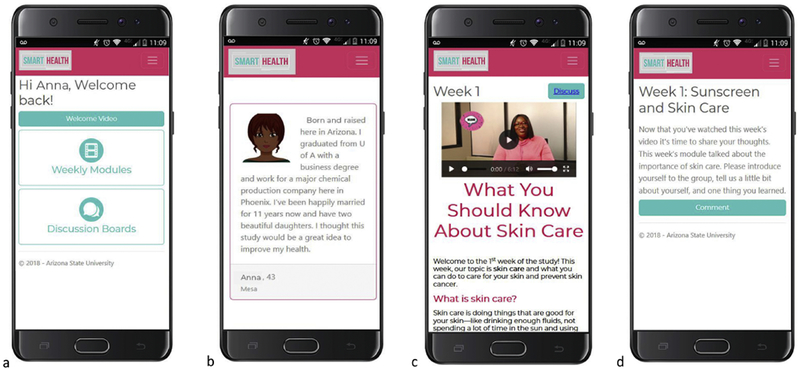
(a) Home screen. (b) Example personal profile page, (c) Example multi-media module, (d) Example discussion board prompt.
3. PROTOCOL
Figure 5 illustrates the study schema, participant flow, and outcome measures by assessment time point. Participant recruitment and enrollment begin Fall 2018.
Figure 5.
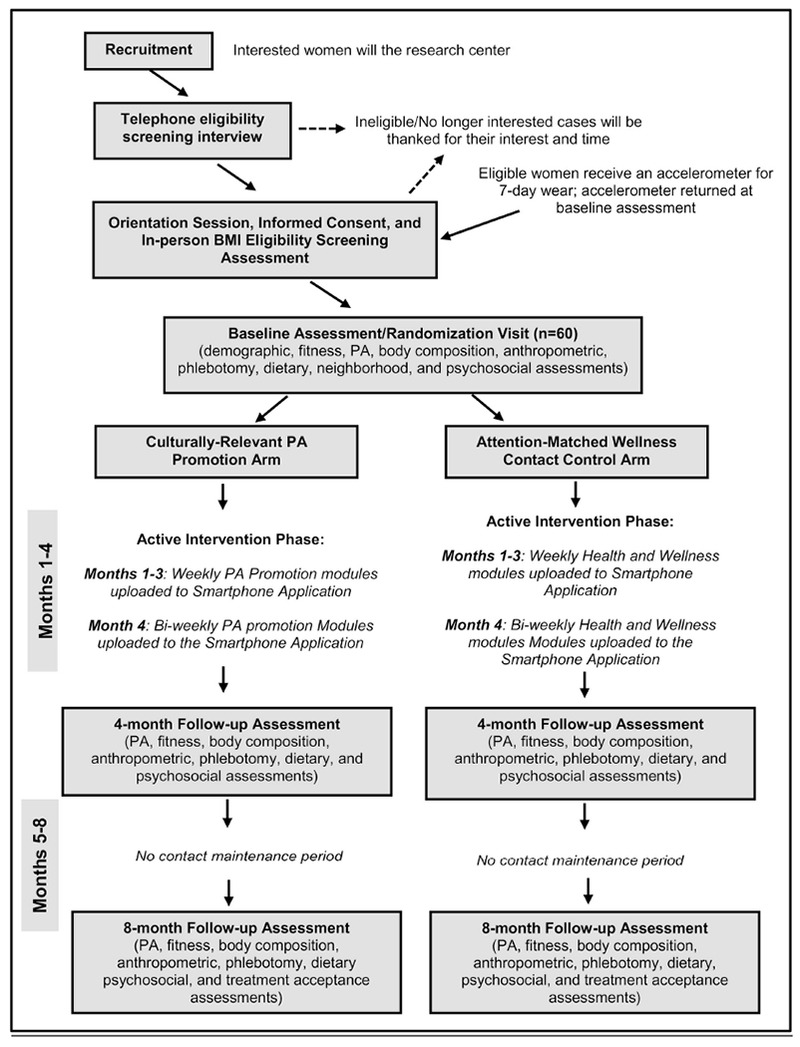
Study schema and participant flow diagrams.
3.1. Recruitment
Participants will be recruited using community-based strategies that have proven successful [50, 57], including recruitment via email distribution lists, placing fliers at community locations, and conducting in-person recruitment at AA-orientated social/organization such as AA sororities, churches, and related venues. Recruitment materials will advertise a “health and wellness” study for AA women and encourage interested individuals to contact study staff for more information.
3.2. Participant Enrollment and Study Assessment Protocol
Interested individuals will call the research center to learn more about the study. During this initial call with participants, study staff will explain that the purpose of the study is to evaluate two different health promotion interventions (i.e., the PA intervention and general health and wellness intervention) and briefly describe the topics covered in each intervention arm. Women who are interested in participating and agree to be randomized to either study arm will then complete an eligibility screening interview, including a telephone version of the Physical Activity Readiness Questionnaire (PAR-Q) [49], which asks about cardiovascular/musculoskeletal risk factors that contraindicate participation in PA. Endorsing any item on the PAR-Q is an exclusion criterion, unless the participant provides a physician’s note allowing her to participate in the study. Women eligible for participation after the telephone screening will be invited to attend an in-person orientation to learn more about the study.
At the orientation session, attendees will be given an in-depth overview of the two different treatment groups, the pros and cons of being randomized to each study group, all study assessment procedures, and expectations for participation (i.e., participants are expected to complete all study assessments and not withdraw from study prior to the end of the 8-month intervention period). Those still interested in participation after the orientation will provide informed consent. Next, study staff will measure each participant’s height and weight to verify eligibility based on BMI status. Eligible women will be given an ActiGraph GT9X Link accelerometer with instructions for wear for the next 7 days. To be considered a valid assessment, participants will need to wear the accelerometer for at least 10 hours per day on at least four days during the seven-day assessment period. Participants not meeting this valid wear time criteria will be given the opportunity to repeat the seven-day monitoring period. Non-wear time compliance during the second monitoring period will result in the participants being disinvited from participating in the study.
After wearing the accelerometer for the required monitoring period, participants will return the accelerometer at the baseline study assessment session and complete demographic, PA, cardiorespiratory fitness, anthropometric, psychosocial, neighborhood environment, and dietary intake assessments (see Section 4 for a description of study measures). Participants will have blood drawn for measurement of cardiometabolic disease biomarkers, and they will complete the aortic pulse wave velocity test. Following baseline assessments, block randomization using a computer-generated allocation number sequence will be used to assign participants to an intervention group. Study staff will assist participants with downloading and installing the appropriate smartphone application on their mobile phones. Follow-up data will be collected at months 4 and 8. Follow-up assessments will exactly parallel those conducted at baseline, with the exception of demographic and neighborhood characteristics, which will not be assessed at follow-up (see Figure 5). Each participant will receive $50 for each study assessment she completes, for a maximum total of $150 for completing all three assessments. At the end of the 8-month study, participants in the PA intervention group will be allowed to keep the Fitbit activity monitors, and to ensure equitable compensation across groups, participants in the wellness attention-matched control condition will also receive equivalent Fitbit devices at the completion of the study.
4. OUTCOME VARIABLES
4.1. Feasibility and Acceptability
Feasibility and acceptability of the interventions will be assessed by examining recruitment, retention, participant utilization of the smartphone application, and treatment acceptance of the intervention and attention control group. Metrics used to establish feasibility and acceptability for recruitment and retention will include accrual of our full sample within 4 months and retention of at least 80% of participants over the 8-month study period. Participant utilization of the smartphone application will be assessed by custom analytics build into the app. App usage data collected will be will be stored in a central database on a secure, university owned and managed server and will be used to determine the extent to which participants utilized the smartphone application and received intervention materials as intended (a measure of intervention “dose”). Specific data points (events) recorded include video play and pause, module display and scroll-to-bottom, and discussion post display and authorship, Treatment acceptance will be assessed by participant responses to the post-intervention treatment receipt survey [57, 64], scores on measures of psychosocial processes (i.e., self-efficacy, behavioral capability, self-regulation), and engagement in (accelerometer-measured) PA.
4.2. Physical Activity
4.2.1. Objectively Measured PA.
The ActiGraph GT9X Link activity monitor will be the primary PA measure in study. The GT9X Link uses a 3-axis accelerometer to objectively measure the rate of body movement. Participants will be asked to wear the activity monitor on the non-dominant wrist during 24 hours per day for 7 consecutive days. To be considered as a valid assessment (and subsequently included in data analyses), women will need to wear the accelerometer for at least 10 waking hours per day on at least 4 days during the 7-day assessment period. Non-wear time will be determined by algorithms developed by Choi et al. [79]. This wrist-worn accelerometer protocol was selected to correspond with current data collection procedures used by NHANES [80], thus allowing us to com pare the PA patterns in our sample to those of the entire U.S. population. Moreover, recent data from NHANES have shown that wear-time compliance is higher when accelerometers are worn on the wrist than when worn on the waist [80, 81]. Raw accelerometer data at 30 Hz will be collected by the GT9X Link activity monitors. Data will be analyzed using the latest scoring methods available.
4.2.2. Self-reported PA.
As a secondary PA measure, participants will complete the REGICOR Short Physical Activity Questionnaire [82]. This 10-item questionnaire collects information on leisure-time PA (including time spent in active transportation to work), occupational PA, and sedentary behavior. The REGICOR provides an estimation of leisure-time energy expenditure, as well as minutes per week of time spent in sedentary, light, moderate, and vigorous intensity activities. The REGICOR has high test-retest reliability for assessing moderate-to-vigorous PA (i.e., interclass correlations of .79 and .95 for moderate and vigorous intensity PA, respectively), is sensitive to assessing changes in PA over time, and has been validated against accelerometers as an accurate measure of PA [82].
4.3. Cardiometabolic Risk Markers
4.3.1. Body Weight and Anthropometries.
Participants will have their weight, height, and waist circumference measured in a private room while wearing light clothing but no shoes. Body weight will be measured with Tanita TBF-300A digital scale to the nearest 0.1 kg. Height measured with Seca 213 portable stadiometerto the nearest 0.1 cm. Waist circumference will be measured at the midpoint between rib and top of iliac crest to the nearest 0.1 cm at the end of participants’ normal expiration. BMI will be calculated as weight in kilograms divided by height in meters squared.
4.3.2. Cardiorespiratory Fitness.
A modified Balke treadmill protocol will be used to estimate peak oxygen uptake (VO2peak). This validated [83], well-tolerated protocol maintains a constant speed (3.0 mph for women) and begins at 2% grade. Workload will increase in grade by 1% every minute until termination of the test. Brachial blood pressure and resting heart rate will be measured while seated, prior to, and five minutes after, completion of the exercise test. During the test, heart rate will be measured continuously with a Polar™ heart rate monitor, ratings of perceived exertion (RPE)will be measured every minute, and blood pressure will be measured every four minutes. Metabolic responses to exercise will be assessed using an Oxycon mobile device (CareFusion) and breath-by-breath indirect calorimetry. To participate in the exercise test, participants must be classified as low-to-moderate risk for moderate-intensity walking according to 2013 American College of Sports Medicine (ACSM) screening criteria [84]. Criteria for test termination (also following ACSM guidelines) will include participant desire to stop; signs or symptoms of angina, poor perfusion, neurological symptoms, fatigue, shortness of breath, or claudication; a drop in systolic blood pressure ≥ 10 mm Hg with an increase in work rate or systolic blood pressure decreasing below the value obtained prior to testing; excessive rise in blood pressure (i.e., systolic blood pressure >250 mm HG or diastolic > 115 mm HG); or when the participant reaches VO2peak or 85% age-predicted maximal heart rate. Reason for stopping the test and any adverse events will be recorded. A warm-up and recovery period walk of 2.5 mph, 0% grade for 2 - 3 minutes will occur immediately before and after the test, respectively. VO2peakwill be estimated using the Foster equation [85].
4.3.3. Aortic Pulse Wave Velocity (PWV) Test.
Aortic PWV will be measured by a certified sonographer. This test is a measure of aortic stiffness and is a strong predictor of cardiovascular events and all-cause mortality [86, 87]. To begin this test, a blood pressure cuff will be placed around the participant’s thigh and the distance between the carotid and femoral arteries will be measured to the nearest centimeter. Next, the participant will be asked to rest in the supine position in a quiet, temperature-controlled room for 15 minutes. After this 15-minute rest period is complete, the aortic pulse wave velocity test will be conducted using the SphygmoCor XCEL system. The blood pressure cuff on the participant’s thigh will be inflated to sub-systolic pressure (<150 mmHg) that relates to brachial pressure to capture the femoral artery waveform. Using gentle pressure, the technician will place an applanation tonometer over the carotid artery. The SphygmoCor XCEL system then assesses the time it takes for the pulse takes to travel from the carotid artery to the femoral artery (i.e., transit time). The pulse wave velocity is automatically determined by the system by dividing the distance between the carotid and femoral arteries by the pulse transit time. Three measurements will be taken with the SphygmoCor device, with the 2 closest values being averaged to obtain PWV.
4.3.3. Disease Risk Biomarkers.
Venous blood will be collected by a certified phlebotomist after a 10-hour fast for the measurement of serum makers of cardiometabolic disease risk. Serum or plasma separated by centrifugation and stored at −80C. Fasting plasma glucose and serum lipid panel (TG, total cholesterol, LDL-C, HDL-C) will be measured using a Randox RX Daytona™ automated chemistry analyzer (GMI Inc, Ramsey, Minnesota). Serum insulin will be measured on a Wizard© automatic gamma counter (PerkinElmer Inc, Waltham, MA) using Millipore HI-14K radioimmunoassay analyzer (MilliporeSigma, Burlington, MA). Insulin sensitivity assessed by calculating homeostatic model assessment (HOMA) scores as: glucose (mg/dl) × insulin (μU/ml)/405. Tumor necrosis factor-alpha (TNF-α) and Interleukin 1 beta (IL-1 β) measured in serum using commercial ELISA kits (ALPCO; Pierce EH2IL1B).
4.4. Theoretical Mediators
4.4.1. Self-efficacy.
Self-efficacy for PA will be assessed by the Exercise Confidence Survey [88]. This 12-item survey has previously established validity [88] and reliability (Cronbach’s alphas = .71 to .85) among samples of AA women.
4.4.2. Social Support.
Social support for exercise will be evaluated using the Social Support for Exercise Survey [89]. This scale provides two separate outcomes for social support: one for family support (10-items) and the other for support from friends (10-items). The instrument has established validity [89] and has shown good reliability in our previous work with AA women (Cronbach’s alphas = .93 to .90 for family subscale; .79 and .92 for friends subscale) [57].
4.4.3. Self-regulation.
Self-regulation for PA will be assessed by the Self-Regulation Scale from the Health Beliefs Survey [90, 91]. This validated [90, 91], 10-item instrument has been used in previous research with AA women, showing fair to good (Cronbach’s alphas =.57 to .74) [57, 64, 65].
4.4.4. Outcome Expectations.
The Outcome Expectation Scale for Exercise (9-items) [92] will be used to evaluated outcome expectations for PA. This scale has been validated in AA populations [93] and has shown good reliability (Cronbach’s alphas =.80 to 0.83) in samples of AA women [57, 64].
4.4.5. Behavioral Capability.
Behavioral capability for PA will be assessed using a 6-item scale developed by the research team for the current study. This measure will be adapted from previous research [94, 95] and used to evaluate knowledge of National PA guidelines and the health benefits of PA.
4.5. Potential Moderators
4.5.1. Demographics:
Demographic characteristics of participants (age, education, income, ethnicity, number of children in household, marital/relationships status) will be assessed.
4.5.2. Neighborhood Health Questionnaire:
This 33-item instrument [96] assesses perceptions of one’s neighborhood on seven dimensions (walking environment, aesthetic quality, availability of healthy foods, safety, social cohesion, violence, and activities with neighbors). Subscales have shown good test-retest reliability (r=.60 to r=.88) and internal consistency (Cronbach’s alphas = .73 to .88) [96].
4.6. Additional Measures
4.6.1. Dietary Intake.
Dietary intake will be explored as a covariate in outcome analyses and will be assessed by the Arizona Food Frequency Questionnaire (AFFQ). This questionnaire proves a semi-quantitative measure of energy and nutrient intake. Reliability and validity of this instrument has previously established [97, 98].
5. Intervention Fidelity/Quality.
The smartphone application will be programmed to automatically deliver intervention materials on a standardized timeline. Study staff will monitor intervention delivery on a daily basis and ensure it does not deviate from the planned timeline. If an issue does arise, study staff will alert the PI who will work closely with the software engineer to quickly resolve the issue. Analytic tracking software will be used to ensure that participants wear the Fitbit activity monitor as prescribed. Should the research team observe a participant not wearing the Fitbit activity monitor for a period of 3 consecutive days or for a total of 4 out of 7 consecutive days, a member of the team will contact the participant in an attempt to identify and remedy the reason for non-wear compliance. Additionally, during the 4-month active intervention period, study staff will follow up with participants every two weeks via telephone or text to identify if they are having any issues with the Smart Walk/Smart Health app and help remedy issues that may arise. The PI will develop a manual outlining all study protocols. All members of the research team will complete formal training (led by PI) on study protocols and procedures. The PI will periodically audit data collection assessment sessions for protocol adherence.
6. Statistical Analyses
6.1. Sample Size Considerations
The primary aim of this study is to establish the acceptability and feasibility of the smartphone-delivered intervention. Accordingly, the analytic focus will be on deriving estimates of the magnitudes of intervention effects rather than on tests of statistical significance. Effect size estimates derived from the proposed study will be used to inform the design of subsequent large-scale trials. Thirty participants will be randomized to each study arm at baseline (N=60 total participants). Based on results of our previous work [57, 64] and statistical simulation studies (e.g., [99]), the projected sample size should be sufficient to address the study aims.
6.2. Data Analysis
Demographic and psychosocial variables will be summarized and compared across treatment arms (using t-tests for continuous measures and chi-square analyses for categorical variables). Wewill examine univariate statistics, bivariate associations among measured variables, and psychometric properties of multi-item self-report instruments. Where necessary, we will apply transformations (e.g., natural log) to normalize distributions of outcome variables. Wewill use generalized linear models to estimate the effect of treatment assignment on accelerometer-measured PA at 4 and 8-months, adjusting for baseline PA along with relevant background characteristics (e.g., age at baseline). Wewill use a parallel approach to estimate intervention effects on weight, aerobic fitness, waist circumference, blood pressure, lipid profiles, fasting blood glucose, aortic pulse wave velocity, pro-inflammation biomarkers implicated in cardiometabolicdisease risk(TNF-α, IL-β1), and each hypothesized mediator. We will explore associations between changes in PA and changes in the outcomes noted above as well as potential moderating effects (via Intervention [Smart Walk vs. Control] × Moderator interaction terms) of sociodemographic factors and neighborhood walkability. Data will be analyzed using an intent-to-treat approach. All randomized participants will be included in outcome analysis, regardless of non-compliance to study protocol, withdrawal, or any other issue that may arise after randomization. Where warranted, to minimize bias and loss of power due to missing data, wewill use multiple imputation methods [100] as implemented in PROC MIANALYZE under SAS 9.4.
7. SUMMARY
Smart Walk is a theory-driven, culturally relevant smartphone-delivered intervention designed to increase PA and reduce cardiometabolic disease risk among physically inactive AA women with obesity. A strength of Smart Walk includes attention directed to the deep structure cultural relevance of AA women’s lives with extensive detail paid to the fidelity of the theoretical constructs underpinning study activities. Together, these elements are designed to enhance the acceptance and salience of the intervention and are expected to increase the likelihood of it having a positive impact on PA behaviors of participants. Another critical element of the intervention is the delivery channel. Recent data from the Pew American Life Project show that 94% of AA adults own a cellular phone, with the majority (72%) owning a smartphone [47]. Thus, by using a smartphone application to deliver the intervention, we are leveraging an accessible communication technologies that are already in common use among AA women, further enhancing the likelihood of intervention acceptance. Moreover, this technology-mediated approach also helps overcome commonly reported barriers to participating in face-to-face behavior change interventions, including childcare issues, transportation problems, and work schedules [101, 102].
Novel methodological aspects of the intervention include using an objective PA measure (accelerometers) as the primary PA outcome and incorporating a 4-month, no-contact follow-up period to evaluate the longer-term effects of the intervention. Previous reviews of PA intervention research among AA women [35–37] have noted that the majority of research with AA women has relied on self-report measures of PA and single, immediate post-intervention assessments, thus precluding rigorous evaluation of longer-term maintenance of intervention effects on PA. The methodological enhancements implemented in this study will help advance intervention research focused on promoting PA among AA women. Additionally, few behavioral interventions [103] have explored the underlying mechanisms through which PA reduces cardiometabolic disease risk among AA women. This study will explore several pro-inflammation biomarkers (TNF-α, IL-β1) and physiological adaptations (estimated peak oxygen uptake, aortic pulse wave velocity) influenced by PA intervention and linked to cardiometabolic disease. Findings will have the potential to provide further insight on the physiological responses to PA among AA women that may contribute to cardiometabolic risk reduction.
Results of the Smart Walk intervention will help inform future research with AA women. Limited research has explored the use of mHealth interventions to promote PA among AA women. To our knowledge, this study will be one of the first to deliver a culturally relevant behavioral PA intervention exclusively through mHealth technology. Results will provide a basis of knowledge for researchers to use in future research and further enhance PA promotion efforts among AA women. Moreover, should results reflect favorable outcomes, the Smart Walk intervention can be easily expanded for testing in a large-scale, fully powered efficacy clinicaltrial.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- [1].Ogden CL, Carroll MD, Flegal KM, Prevalence of obesity in the United States, JAMA 312(2) (2014) 189–90. [DOI] [PubMed] [Google Scholar]
- [2].Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. , Heart disease and stroke statistics-2016 update: a report from the American Heart Association, Circulation 133(4) (2016) e38–e360. [DOI] [PubMed] [Google Scholar]
- [3].Swift DL, Johannsen NM, Lavie CJ, Earnest CP, Church TS, The role of exercise and physical activity in weight loss and maintenance, Prog Cardiovasc Dis 56(4) (2014) 441–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Chin SH, Kahathuduwa CN, Binks M, Physical activity and obesity: what we know and what we need to know, Obes Rev 17(12) (2016) 1226–1244. [DOI] [PubMed] [Google Scholar]
- [5].Gaesser GA, Angadi SS, Sawyer BJ, Exercise and diet, independent of weight loss, improve cardiometabolic risk profile in overweight and obese individuals, Phys Sportsmed 39(2) (2011) 87–97. [DOI] [PubMed] [Google Scholar]
- [6].Semlitsch T, Jeitler K, Hemkens LG, Horvath K, Nagele E, Schuermann C, et al. , Increasing physical activity for the treatment of hypertension: a systematic review and meta-analysis, Sports Med 43(10) (2013) 1009–23. [DOI] [PubMed] [Google Scholar]
- [7].Nystoriak MA, Bhatnagar A, Cardiovascular effects and benefits of exercise, Front Cardiovasc Med 5 (2018) 135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Orio F, Muscogiuri G, Ascione A, Marciano F, Volpe A, La Sala G, et al. , Effects of physical exercise on the female reproductive system, Minerva Endocrinol 38(3) (2013) 305–19. [PubMed] [Google Scholar]
- [9].Kelley GA, Kelley KS, Roberts S, Haskell W, Comparison of aerobic exercise, diet or both on lipids and lipoproteins in adults: a meta-analysis of randomized controlled trials, Clin Nutr 31(2) (2012) 156–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Eckardt K, Taube A, Eckel J, Obesity-associated insulin resistance in skeletal muscle: role of lipid accumulation and physical inactivity, Rev Endocr Metab Disord 12(3) (2011) 163–72. [DOI] [PubMed] [Google Scholar]
- [11].Venkatasamy VV, Pericherla S, Manthuruthil S, Mishra S, Hanno R, Effect of physical activity on insulin resistance, inflammation and oxidative stress in diabetes mellitus, J Clin Diagn Res 7(8) (2013) 1764–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Thomas GN, Jiang CQ, Taheri S, Xiao ZH, Tomlinson B, Cheung BM, et al. , A systematic review of lifestyle modification and glucose intolerance in the prevention of type 2 diabetes, Curr Diabetes Rev 6(6) (2010) 378–87. [DOI] [PubMed] [Google Scholar]
- [13].Jarvie JL, Whooley MA, Regan MC, Sin NL, Cohen BE, Effect of physical activity level on biomarkers of inflammation and insulin resistance over 5 years in outpatients with coronary heart disease (from the Heart and Soul Study), Am J Cardiol 114(8) (2014) 1192–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Gay JL, Buchner DM, Schmidt MD, Dose-response association of physical activity with HbA1c: intensity and bout length, Prev Med 86 (2016) 58–63. [DOI] [PubMed] [Google Scholar]
- [15].Zhang X, Imperatore G, Thomas W, Cheng YJ, Lobelo F, Norris K, et al. , Effect of lifestyle interventions on glucose regulation among adults without impaired glucose tolerance or diabetes: A systematic review and meta-analysis, Diabetes Res Clin Pract 123 (2017) 149–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Myers J, McAuley P, Lavie C, Despres JP, Arena R, Kokkinos P, Physical activity and cardiorespiratory fitness as major markers of cardiovascular risk: their independent and interwoven importance to health status, Prog Cardiovasc Dis (2014). [DOI] [PubMed] [Google Scholar]
- [17].Swift DL, Lavie CJ, Johannsen NM, Arena R, Earnest CP, O’Keefe JH, et al. , Physical activity, cardiorespiratory fitness, and exercise training in primary and secondary coronary prevention, Circ J 77(2) (2013) 281–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].DeFina LF, Haskell WL, Willis BL, Barlow CE, Finley CE, Levine BD, et al. , Physical activity versus cardiorespiratory fitness: two (partly) distinct components of cardiovascular health?, Prog Cardiovasc Dis (2014). [DOI] [PubMed] [Google Scholar]
- [19].Lin X, Zhang X, Guo J, Roberts CK, McKenzie S, Wu WC, et al. , Effects of exercise training on cardiorespiratory fitness and biomarkers of cardiometabolic health: a systematic review and meta-analysis of randomized controlled trials, J Am Heart Assoc 4(7) (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Green DJ, Eijsvogels T, Bouts YM, Maiorana AJ, Naylor LH, Scholten RR, et al. , Exercise training and artery function in humans: nonresponse and its relationship to cardiovascular risk factors, J Appl Physiol 117(4) (2014) 345–52. [DOI] [PubMed] [Google Scholar]
- [21].Jennersjo P, Ludvigsson J, Lanne T, Nystrom FH, Ernerudh J, Ostgren CJ, Pedometer-determined physical activity is linked to low systemic inflammation and low arterial stiffness in Type 2 diabetes, Diabet Med 29(9) (2012) 1119–25. [DOI] [PubMed] [Google Scholar]
- [22].Sardeli AV, Gaspari AF, Chacon-Mikahil MP, Acute, short-, and long-term effects of different types of exercise in central arterial stiffness: a systematic review and meta-analysis, J Sports Med Phys Fitness 58(6) (2018) 923–932. [DOI] [PubMed] [Google Scholar]
- [23].US Department of Health and Human Services, 2008 physical activity guidelines for Americans, US Department of Health and Human Services, Hyattsville, MD, 2008. [Google Scholar]
- [24].U.S. Department of health and Human Services, Physical Activity Guidelines for Americans, U.S. Department of Health and Human Services, Washington D.C., 2018. [Google Scholar]
- [25].Williams WM, Yore MM, Whitt-Glover MC, Estimating physical activity trends among blacks in the United States through examination of four national surveys, AIMS Public Health 5(2) (2018) 144–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M, Physical activity in the United States measured by accelerometer, Med Sci Sports Exerc 40(1) (2008) 181–8. [DOI] [PubMed] [Google Scholar]
- [27].Hooker SP, Hutto B, Zhu W, Blair SN, Colabianchi N, Vena JE, et al. , Accelerometer measured sedentary behavior and physical activity in white and black adults: The REGARDS study, J Sci Med Sport 19(4) (2016) 336–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Gabriel KP, Sidney S, Jacobs JDR, Whitaker KM, Carnethon MR, Lewis CE, et al. , 10-year changes in accelerometer-based physical activity and sedentary time during midlife: CARDIA Study, Am J Epidemiol (2018) kwy117–kwy117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Burke LE, Ma J, Azar KM, Bennett GG, Peterson ED, Zheng Y, et al. , Current science on consumer use of mobile health for cardiovascular disease prevention: a scientific statement from the American Heart Association, Circulation 132(12) (2015) 1157–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Muller AM, Alley S, Schoeppe S, Vandelanotte C, The effectiveness of e-& mHealth interventions to promote physical activity and healthy diets in developing countries: A systematic review, Int J Behav Nutr Phys Act 13(1) (2016) 109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Davies CA, Spence JC, Vandelanotte C, Caperchione CM, Mummery WK, Meta-analysis of internet-delivered interventions to increase physical activity levels, Int J Behav Nutr Phys Act 9 (2012) 52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Hall AK, Cole-Lewis H, Bernhardt JM, Mobile text messaging for health: a systematic review of reviews, Annu Rev Public Health 36 (2015) 393–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Buchholz SW, Wilbur J, Ingram D, Fogg L, Physical activity text messaging interventions in adults: a systematic review, Worldviews Evid Based Nurs (2013). [DOI] [PubMed] [Google Scholar]
- [34].Beishuizen CR, Stephan BC, van Gool WA, Brayne C, Peters RJ, Andrieu S, et al. , Web-based interventions targeting cardiovascular risk factors in middle-aged and older people: a systematic review and meta-analysis, J Med Internet Res 18(3) (2016) e55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Whitt-Glover MC, Keith NR, Ceaser TG, Virgil K, Ledford L, Hasson RE, A systematic review of physical activity interventions among African American adults: evidence from 2009 to 2013, Obes Rev 15 Suppl 4 (2014) 125–45. [DOI] [PubMed] [Google Scholar]
- [36].Pekmezi D, Jennings E, Interventions to promote physical activity among African Americans., American Journal of Lifestyle Medicine 3 (2009) 173–184. [Google Scholar]
- [37].Whitt-Glover MC, Kumanyika SK, Systematic review of interventions to increase physical activity and physical fitness in African-Americans, Am J Health Promot 23(6) (2009) S33–56. [DOI] [PubMed] [Google Scholar]
- [38].Resnicow K, Baranowski T, Ahluwalia JS, Braithwaite RL, Cultural sensitivity in public health: defined and demystified, Ethn Dis 9(1) (1999) 10–21. [PubMed] [Google Scholar]
- [39].Resnicow K, Soler R, Braithwaite RL, Ahluwalia JS, Butler J, Cultural sensitivity in substance use prevention, J Community Psychol 28(3) (2000) 271–290. [Google Scholar]
- [40].Resnicow K, Braithwaite R, Dilorio C, G. K, Applying theory to culturally diverse and unique populations, in: Glanz K, Lewis F, Rimer B (Eds.), Health Behav Health Educ, Jossey-Bass, San Francisco, CA, 2002, pp. 485–509. [Google Scholar]
- [41].Matthews L, Kirk A, Macmillan F, Mutrie N, Can physical activity interventions for adults with type 2 diabetes be translated into practice settings? A systematic review using the RE-AIM framework, Transl Behav Med 4(1) (2014) 60–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Belanger-Gravel A, Godin G, A Vezina-lm L, Amireault S, Poirier P, The effect of theory-based interventions on physical activity participation among overweight/obese individuals: a systematic review, Obes Rev 12(6) (2011) 430–9. [DOI] [PubMed] [Google Scholar]
- [43].Brook RD, Appel LJ, Rubenfire M, Ogedegbe G, Bisognano JD, Elliott WJ, et al. , Beyond medications and diet: alternative approaches to lowering blood pressure: a scientific statement from the american heart association, Hypertension 61(6) (2013) 1360–83. [DOI] [PubMed] [Google Scholar]
- [44].U.S. Census Bureau, Community Facts, 2017. https://factfinder.census.gov/faces/nav/isf/pages/community_facts.xhtmI. (Accessed October 3 2017).
- [45].Centers for Disease Control and Prevention (CDC), BRFSS Web Analysis Tool, 2017. https://nccd.cdc.gov/s_broker/WEATSQL.exe/weat/index.hsql. (Accessed October4 2017).
- [46].H.C. Institute, Disparities Dashboard, 2017. http://www.arizonahealthmatters.org/index.php?module=indicators&controller=index&action=dashboard&id=83016456097935108&card=0&localeld=5. (Accessed October3 2017).
- [47].Pew Research Center, Mobile Fact Sheet, 2017. http://www.pewinternet.org/fact-sheet/mobile/. (Accessed August 31 2017).
- [48].Joseph RP, Keller C, Adams MA, Ainsworth BE, Validity of two brief physical activity questionnaires with accelerometers among African-American women, Prim Health Care Res Dev 17(3) (2016) 265–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Thomas S, Reading J, Shephard RJ, Revision of the Physical Activity Readiness Questionnaire (PAR-Q), Can J Sport Sci 17(4) (1992) 338–45. [PubMed] [Google Scholar]
- [50].Joseph RP, Ainsworth BE, Mathis L, Hooker SP, Keller C, Utility of social cognitive theory in intervention design for promoting physical activity among African-American women: a qualitative study, Am J Health Behav 54(5) (2017) 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Joseph RP, Keller C, Affuso O, Ainsworth BE, Designing culturally relevant physical activity programs for African-American women: a framework for intervention development, J Racial Ethn Health Disparities (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Joseph RP, Ainsworth BE, Keller C, Dodgson JE, Barriers to physical activity among African American women: an integrative review of the literature., Women & Health 55(6) (2015) 579–699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Joseph RP, Coe K, Ainsworth BE, Hooker SP, Mathis L, Keller C, Hair as a carrier to physical activity among African American women: a qualitative exploration, Front Public Health 5 (2017) 367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Tudor-Locke C, Han H, Aguiar EJ, Barreira TV, Schuna JM Jr., Kang M, et al. , How fast is fast enough? Walking cadence (steps/min) as a practical estimate of intensity in adults: a narrative review, Br J Sports Med 52(12) (2018) 776–788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Slaght J, Senechal M, Hrubeniuk TJ, Mayo A, Bouchard DR, Walking cadence to exercise at moderate intensity for adults: a systematic review, J Sports Med (Hindawi Publ Corp) 2017 (2017) 4641203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Reese JM, Joseph RP, Cherrington A, Allison J, Kim YI, Spear B, et al. , Development of participant-informed text messages to promote physical activity among African American women attending college: a qualitative mixed-methods inquiry, J Transcult Nurs 28(3) (2017) 236–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Joseph RP, Keller C, Adams MA, Ainsworth BE, Print versus a culturally-relevant Facebook and text message delivered intervention to promote physical activity in African American Women: a randomized pilot trial, BMC Women’s Health 15 (2015) 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Bandura A, Social foundations of thought and action: a social cognitive framework, Prentice Hall, Englewood Cliffs, NJ, 1986. [Google Scholar]
- [59].Glanz K, Rimer B, Viswanath K, Health Behavior: Theory, Research, and Practice, 5th ed., Jossey-Bass, San Francisco, CA, 2015. [Google Scholar]
- [60].Michie S, Abraham C, Whittington C, McAteer J, Gupta S, Effective techniques in healthy eating and physical activity interventions: a meta-regression, Health Psychol, PsycINFO Database Record 2009 APA, all rights reserved., United States, 2009, pp. 690–701. [DOI] [PubMed] [Google Scholar]
- [61].Chase JA, Physical activity interventions among older adults: a literature review, Res Theory Nurs Pract 27(1) (2013) 53–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Belanger-Gravel A, Godin G, Vezina-Im LA, Amireault S, Poirier P, The effect of theory-based interventions on physical activity participation among overweight/obese individuals: a systematic review., Obes Rev 12(6) (2011) 430–9. [DOI] [PubMed] [Google Scholar]
- [63].Rovniak LS, Hovell MF, Wojcik JR, Winett RA, Martinez-Donate AP, Enhancing theoretical fidelity: an e-mail-based walking program demonstration., Am J Health Promot 20(2) (2005) 85–95. [DOI] [PubMed] [Google Scholar]
- [64].Joseph RP, Pekmezi D, Dutton GR, Cherrington AL, Kim YI, Allison JJ, et al. , Results of a culturally adapted internet-enhanced physical activity pilot intervention for overweight and obese young adult African American women, J Transcult Nurs (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Joseph RP, Pekmezi DW, Lewis T, Dutton G, Turner LW, Durant NH, Physical activity and Social Cognitive Theory outcomes of an Internet-enhanced physical activity intervention for African American female college students, Journal of Health Disparities Research and Practice 6(2) (2013) 18. [PMC free article] [PubMed] [Google Scholar]
- [66].Centers for Disease Control and Prevention, National Center for Health Statistics, Health Data Interactive., 2015. (Accessed August 1 2015).
- [67].Eyler AA, Matson-Koffman D, Vest JR, Evenson KR, Sanderson B, Thompson JL, et al. , Environmental, policy, and cultural factors related to physical activity in a diverse sample of women: The Women’s Cardiovascular Health Network Project-summary and discussion, Women Health 36(2) (2002) 123–34. [PubMed] [Google Scholar]
- [68].Jones LV, Hopson LM, Gomes A-M, Intervening with African-Americans: culturally specific practice considerations, J Ethnic Cult Divers Soc Work 21(1) (2012) 37–54. [Google Scholar]
- [69].Im EO, Ko Y, Hwang H, Yoo KH, Chee W, Stuifbergen A, et al. , “Physical activity as a luxury”: African American women’s attitudes toward physical activity, West J Nurs Res 34(3) (2012) 317–39. [DOI] [PubMed] [Google Scholar]
- [70].Harley AE, Odoms-Young A, Beard B, Katz ML, Heaney CA, African American social and cultural contexts and physical activity: strategies for navigating challenges to participation, Women Health 49(1) (2009) 84–100. [DOI] [PubMed] [Google Scholar]
- [71].Awad GH, Norwood C, Taylor DS, Martinez M, McClain S, Jones B, et al. , Beauty and body image concerns among African American college women, Journal of Black Psychology 41(6) (2015) 540–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Huebschmann AG, Campbell LJ, Brown CS, Dunn AL, “My hair or my health:” Overcoming barriers to physical activity in African American women with a focus on hairstyle-related factors, Women Health 56(4) (2016) 428–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [73].Versey HS, Centering perspectives on Black women, hair politics, and physical activity, Am J Public Health 104(5) (2014) 810–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Chithambo TP, Huey SJ, Black/white differences in perceived weight and attractiveness among overweight women, J Obes 2013 (2013) 320326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [75].Hesse-Biber S, Livingstone S, Ramirez D, Barko EB, Johnson AL, Racial identity and body image among black female college students attending predominately white colleges, Sex Roles 63(9) (2010) 697–711. [Google Scholar]
- [76].Carter-Edwards L, Bastian LA, Revels J, Durham H, Lokhnygina Y, Amamoo MA, et al. , Body image and body satisfaction differ by race in overweight postpartum mothers, J Womens Health (Larchmt) 19(2) (2010) 305–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [77].Lemelle AJ, Reed W, Taylor SE, Handbook of African American health: social and behavioral interventions, Springer Science & Business Media; 2011. [Google Scholar]
- [78].Kreuter MW, Lukwago SN, Bucholtz RD, Clark EM, Sanders-Thompson V, Achieving cultural appropriateness in health promotion programs: targeted and tailored approaches, Health Educ Behav 30(2) (2003) 133–46. [DOI] [PubMed] [Google Scholar]
- [79].Choi L, Liu Z, Matthews CE, Buchowski MS, Validation of accelerometer wear and nonwear time classification algorithm, Med Sci Sports Exerc 43(2) (2011) 357–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80].Troiano RP, McClain JJ, Brychta RJ, Chen KY, Evolution of accelerometer methods for physical activity research, British Journal of Sports Medicine 48(13) (2014) 1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [81].Tudor-Locke C, Barreira TV, Schuna JM, Mire EF, Chaput J-P, Fogelholm M, et al. , Improving wear time compliance with a 24-hour waist-worn accelerometer protocol in the International Study of Childhood Obesity, Lifestyle and the Environment (ISCOLE), Int J Behav Nutr Phys Act 12 (2015) 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [82].Molina L, Sarmiento M, Penafiel J, Donaire D, Garcia-Aymerich J, Gomez M, et al. , Validation of the Regicor Short Physical Activity Questionnaire for the adult population, PLoS One 12(1) (2017) e0168148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [83].Burckhardt CS, Clark SR, Padrick KP, Use of the modified Balke treadmill protocol for determining the aerobic capacity of women with fibromyalgia, Arthritis Care Res 2(4) (1989) 165–7. [DOI] [PubMed] [Google Scholar]
- [84].American College of Sports Medicine, ACSM’s Guidelines for Exercise Testing and Prescription, 9th ed, Wolters Kluwer/Lippincott Williams & Wilkins Health, Baltimore, MD, 2013. [Google Scholar]
- [85].Foster C, Crowe AJ, Daines E, Dumit M, Green MA, Lettau S, et al. , Predicting functional capacity during treadmill testing independent of exercise protocol, Med Sci Sports Exerc 28(6) (1996) 752–6. [DOI] [PubMed] [Google Scholar]
- [86].Vlachopoulos C, Aznaouridis K, Stefanadis C, Prediction of cardiovascular events and all cause mortality with arterial stiffness: a systematic review and meta-analysis, J Am Coll Cardiol 55(13) (2010) 1318–27. [DOI] [PubMed] [Google Scholar]
- [87].Ben-Shlomo Y, Spears M, Boustred C, May M, Anderson SG, Benjamin EJ, et al. , Aortic pulse wave velocity improves cardiovascular event prediction: an individual participant meta-analysis of prospective observational data from 17,635 subjects, J Am Coll Cardiol 63(7) (2014) 636–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [88].Sallis JF, Pinski RB, Grossman RM, Patterson TL, Nader PR, The development of self-efficacy scales for health-related diet and exercise behaviors, Health Educ Res 3 (1988). [Google Scholar]
- [89].Sallis JF, Grossman RM, Pinski RB, Patterson TL, Nader PR, The development of scales to measure social support for diet and exercise behaviors, Prev Med 16(6) (1987) 825–36. [DOI] [PubMed] [Google Scholar]
- [90].Anderson ES, Winett RA, Wojcik JR, Williams DM, Social cognitive mediators of change in a group randomized nutrition and physical activity intervention: social support, self-efficacy, outcome expectations and self-regulation in the guide-to-health trial, J Health Psychol 15(1) (2010) 21–32. [DOI] [PubMed] [Google Scholar]
- [91].Anderson ES, Wojcik JR, Winett RA, Williams DM, Social-cognitive determinants of physical activity: the influence of social support, self-efficacy, outcome expectations, and self-regulation among participants in a church-based health promotion study., Health Psychol 25(4) (2006) 510–20. [DOI] [PubMed] [Google Scholar]
- [92].Resnick B, Zimmerman SI, Orwig D, Furstenberg AL, Magaziner J, Outcome expectations for exercise scale: utility and psychometrics, J Gerontol B Psychol Sci Soc Sci 55(6) (2000) S352–6. [DOI] [PubMed] [Google Scholar]
- [93].Resnick B, Luisi D, Vogel A, Junaleepa P, Reliability and validity of the self-efficacy for exercise and outcome expectations for exercise scales with minority older adults, J Nurs Meas 12(3) (2004) 235–47. [DOI] [PubMed] [Google Scholar]
- [94].Vega WA, Sallis JF, Patterson T, Rupp J, Atkins C, Nader PR, Assessing knowledge of cardiovascular health-related diet and exercise behaviors in Anglo- and Mexican-Americans, Prev Med 16(5) (1987) 696–709. [DOI] [PubMed] [Google Scholar]
- [95].Kay MC, Carroll DD, Carlson SA, Fulton JE, Awareness and knowledge of the 2008 Physical Activity Guidelines for Americans, J Phys Act Health 11(4) (2014) 693–698. [DOI] [PubMed] [Google Scholar]
- [96].Mujahid MS, Diez Roux AV, Morenoff JD, Raghunathan T, Assessing the measurement properties of neighborhood scales: from psychometrics to ecometrics, Am J Epidemiol 165(8) (2007) 858–67. [DOI] [PubMed] [Google Scholar]
- [97].Martinez ME, Marshall JR, Graver E, Whitacre RC, Woolf K, Ritenbaugh C, et al. , Reliability and validity of a self-administered food frequency questionnaire in a chemoprevention trial of adenoma recurrence, Cancer Epidemiol Biomarkers Prev 8(10) (1999) 941–6. [PubMed] [Google Scholar]
- [98].Thomson CA, Giuliano A, Rock CL, Ritenbaugh CK, Flatt SW, Faerber S, et al. , Measuring dietary change in a diet intervention trial: comparing food frequency questionnaire and dietary recalls, Am J Epidemiol 157(8) (2003) 754–62. [DOI] [PubMed] [Google Scholar]
- [99].Whitehead AL, Julious SA, Cooper CL, Campbell MJ, Estimating the sample size for a pilot randomised trial to minimise the overall trial sample size for the external pilot and main trial for a continuous outcome variable, Statistical Methods in Medical Research 25(3) (2016) 1057–1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [100].Rubin DB, Multiple Imputation for Nonresponse in Surveys, J. Wiley & Sons, New York, 1987. [Google Scholar]
- [101].Attwood S, Morton KL, Mitchell J, Van Emmenis M, Sutton S, Reasons for non-participation in a primary care-based physical activity trial: a qualitative study, BMJ Open 6(5) (2016) e011577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [102].Ingram D, Wilbur J, McDevitt J, Buchholz S, Women’s walking program for African American women: expectations and recommendations from participants as experts, Women Health 51(6) (2011) 566–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [103].Fisher G, Hyatt TC, Hunter GR, Oster RA, Desmond RA, Gower BA, Markers of inflammation and fat distribution following weight loss in African-American and white women, Obesity (Silver Spring) 20(4) (2012) 715–20. [DOI] [PMC free article] [PubMed] [Google Scholar]


