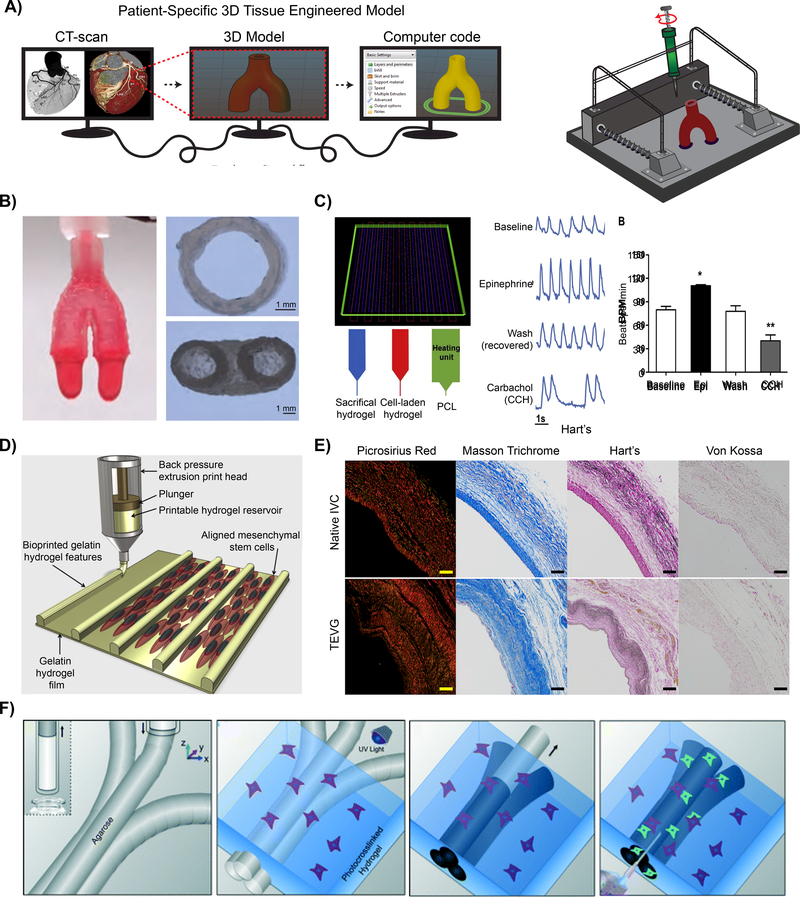
Figure 4: Vascular 3D printed models.
A) Schematic demonstrating the process of fabricating a patient-specific complex geometry using the layer-by-layer 3D printing process. B) A bioink utilizing Nanoengineered Ionic-Covalent Entanglements (NICE) improves the hydrogels printability, producingstiff and elastomeric constructs that are physiologically relevant at modeling macroscale organ biology.[114] © 2018 ACS Applied Materials & Interfaces C) 3D printing of 3-component cardiac tissue to demonstrate the feasibility of cardiac model drug response. The printed cardiac tissue increased in beating frequency (beats per minute; BPM) and amplitude, compared to the baseline, when exposed to epinephrine (Epi). However, once removed, washed, established baseline, and then exposed to Carbachol (CCH), the opposite effect was confirmed. [137] © 2018 Acta Biomaterialia D) Schematic of the manufacturing process used to produce hydrogel printed microchannels that aid in cellular alignment, mimicking the arrangement observed in vivo.[136] © 2018 Biofabrication E) Collagen (Picrosirius Red and Masson Trichrome) and elastin (Hart) deposition of a native inferior vena cava (IVC) compared to a 3D printed tissue engineered vascular graft (TEVG) after 6 months. No signs of ectopic calcification were demonstrated (Von Kossa).[153] © 2017 The Journal of Thoracic and Cardiovascular Surgery F) Graphic representation of the use of 3D printing to form microchannels via template micro-molding, permitting for the use of dynamic co-culture within a printed construct. [76] © 2014 Lab on chip