The NHS England low-priority medicines initiative 2017 described a range of medicines that should not be routinely prescribed in primary care. We previously described trends and variation in prescribing for the medications covered.1 Six months on, we set out to describe how prescribing has changed.
We used the same methodology as before, but with prescribing data updated to May 2018. We examined data on ‘number of items prescribed’, rather than expenditure, as price fluctuations may otherwise obfuscate changes in clinicians’ prescribing choices.
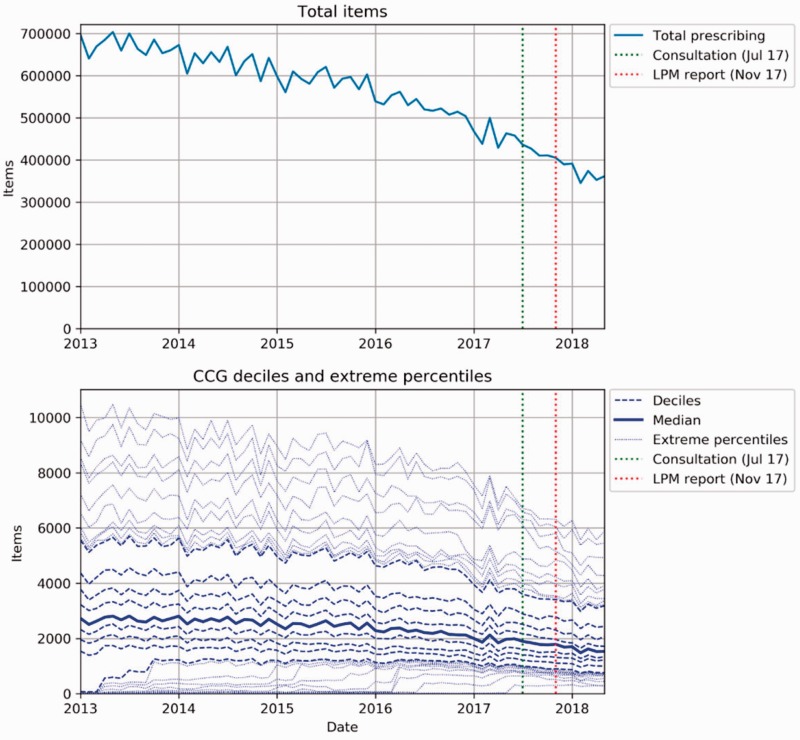
Although there was a reduction in overall use of these medicines (Figure 1), that reduction is in line with the existing downward trend, with no change either after the announcement of the consultation on the scheme (July 2017) or publication of the subsequent consultation report (November 2017). Full results can be seen in our figshare repository.2
Figure 1.
Trends and variation in total number of items prescribed across all areas of NHS England low-priority medicines initiative 2017.
The same pattern is seen for most individual drugs or classes covered by the initiative (online supplementary Figures 2-18). There is a drop in travel vaccine prescriptions, which coincides with the announcement of the consultation (online supplementary Figure 17) and can be observed across most Clinical Commissioning Groups and a drop in lutein and antioxidants coinciding with the publication of the report (online supplementary Figure 10), which seems to be mediated by change in very high-prescribing Clinical Commissioning Groups.
In summary: in most cases, NHS England advising doctors to stop prescribing a drug, in a report and consultation, is not sufficient to cause a noticeable change in clinical practice at a national level.
This reflects our own wider work on trends and variation in care, and the drivers for change, raising issues far beyond cost-saving initiatives.3 The NHS would do well to invest in better ways to disseminate, implement and audit guidance.
Supplemental Material
Supplemental material for Six months on: NHS England needs to focus on dissemination, implementation and audit of its low-priority initiative by Alex J Walker, Seb Bacon, Helen Curtis, Richard Croker, Brian MacKenna and Ben Goldacre in Journal of the Royal Society of Medicine
Declarations
Conflicts of Interest
BG has received research funding from the Laura and John Arnold Foundation, the Wellcome Trust, the Oxford Biomedical Research Centre, the NHS National Institute for Health Research School of Primary Care Research, the Health Foundation and the World Health Organisation; he also receives personal income from speaking and writing for lay audiences on the misuse of science. RC, AJW, HC, SB are employed on BG’s grants for OpenPrescribing. BM is seconded to the DataLab from NHS England and worked on the NHS England low-priority prescribing initiative.
References
- 1.Walker AJ, Curtis HJ, Bacon S, Croker R, Goldacre B. Trends and variation in prescribing of low-priority treatments identified by NHS England: a cross-sectional study and interactive data tool in English primary care. J R Soc Med 2018; 111: 203–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Walker AJ, Goldacre B. Has the NHS England “Low-Value medicines” initiative had an impact on prescribing? Figshare. See 10.6084/m9.figshare.6984296 (last checked 12 October 2018. [DOI] [Google Scholar]
- 3.Curtis HJ, Walker AJ, Goldacre B. Impact of NICE guidance on tamoxifen prescribing in England 2011–2017: an interrupted time series analysis. Br J Cancer 2018; 118: 1268–1275. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material for Six months on: NHS England needs to focus on dissemination, implementation and audit of its low-priority initiative by Alex J Walker, Seb Bacon, Helen Curtis, Richard Croker, Brian MacKenna and Ben Goldacre in Journal of the Royal Society of Medicine