Abstract
Background
Preventing anterior cruciate ligament (ACL) injuries is important to avoid long-term adverse health consequences. Identifying barriers to implementation of these prevention programs is crucial to reducing the incidence of these injuries. Our purpose was to identify barriers of implementation for ACL injury prevention programs and suggest mechanisms for reducing the barriers through application of a Socio-Ecological Model (SEM).
Methods
Studies investigating ACL prevention program effectiveness were searched in Medline via PubMed and the Cochrane Library, and a subsequent review of the references of the identified articles, yielded 15 articles total. Inclusion criteria encompassed prospective controlled trials, published in English, with ACL injuries as the primary outcome. Studies were independently appraised by 2 reviewers for methodological quality using the PEDro scale. Barriers to implementation were identified when reported in at least 2 separate studies. A SEM was used to suggest ways to reduce the identified barriers.
Results
Five barriers were identified: motivation, time requirements, skill requirements for program facilitators, compliance, and cost. The SEM suggested ways to minimize the barriers at all levels of the model from the individual through policy levels.
Conclusion
Identification of barriers to program implementation and suggesting how to reduce them through the SEM is a critical first step toward enabling ACL prevention programs to be more effective and ultimately reducing the incidence of these injuries.
Keywords: Anterior cruciate ligament injury prevention, Barriers to implementation, Neuromuscular training programs, Socio-Ecological Model, Sports injury prevention
1. Introduction
Injuries to the anterior cruciate ligament (ACL) are a common and costly type of sports injury that can detrimentally affect the quality of life for individuals who sustain them.1, 2 It has been estimated that 80,000 people in the USA tear an ACL each year.3 As a serious injury with a long rehabilitation, ACL injuries can cause emotional distress4 and can hinder academic and athletic achievement.5, 6 The cost of surgery and rehabilitation is estimated at USD 2 billion in the USA and contributes to high health care costs.7 Additionally, ACL ruptures are associated with damage to the menisci, as well as an increased risk of osteoarthritis.8, 9, 10 Osteoarthritis is a chronic condition that can cause difficulties with working, exercising, and other daily activities and can contribute to long-term disability.9, 11 Osteoarthritis can occur as soon as 10 years after an ACL tear, and it affects individuals who elect to receive ACL reconstruction and those who elect conservative treatment.2, 10 Because the burden of sustaining an ACL injury is extensive and multifaceted, reducing the number of these injuries that occur would benefit both athletes as individuals and society as a whole. A component of the goals of “Healthy People 2020” is to live high-quality longer lives free of injury.12 Therefore, prevention of ACL injuries through effective ACL injury prevention programs can be viewed as an important public health goal.
Due to the fact that ACL tears carry long-term health and financial burdens and that some (but not all) neuromuscular training programs are effective for reducing ACL injuries, there is a need to better understand the obstacles that may be hindering the widespread use and effectiveness of these programs. Little research has been conducted on barriers to implementing ACL injury prevention programs, and some researchers have been urging that more attention be paid to identifying and overcoming these barriers.13, 14 A systematic review that not only identifies barriers to implementation but also suggests mechanisms to overcome these barriers is non-existent in the literature and would provide a critical framework for ultimately enhancing program effectiveness while lowering the incidence of ACL injuries.
The purpose of our research was to identify and describe potential barriers to implementing ACL injury prevention programs in team sport athletes through a systematic review of the literature. We then utilized the Socio-Ecological Model (SEM), which provides a framework for understanding the interaction and influence of various factors on behavior, to suggest ways to reduce these implementation barriers.
2. Methods
2.1. Data sources and strategy
A systematic review of literature was conducted on ACL injury prevention programs by searching Medline via PubMed and the Cochrane Library (Fig. 1) and in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.15 The keywords “anterior cruciate ligament”, “injury”, and “prevention” combined using Boolean logic were used to conduct the search. This search produced 610 records to which we applied our eligibility criteria of being published in the English language, being published in a peer-reviewed journal, investigating a neuromuscular training program for injury prevention, being a controlled prospective study of team sport athletes, and having ACL injury as an outcome measure. As detailed in Fig. 1, 599 studies were excluded.
Fig. 1.
Flowchart of literature search. ACL = anterior cruciate ligament.
Published meta-analyses and systematic reviews on this topic were also retrieved through the primary search and checked to ensure that relevant studies were not being overlooked. Finally, a subsequent search from the reference lists of articles to be included was then conducted to identify other relevant articles that were not located by the primary online database search. This search added 4 more articles, for a total of 15 studies which met our inclusion criteria.
2.2. Criteria for inclusion
Only prospective, controlled studies of team sport athletes that evaluated a neuromuscular training program for injury prevention and reported ACL injury as an outcome measure were eligible for inclusion. Further, we required that studies be published in English in a peer-reviewed journal. Information on the 15 included studies (types of programs, program effectiveness, and methodological quality) is shown in Table 1.
Table 1.
Summary of studies on ACL injury prevention training programs.
| Study | Description of participants | Number of participants |
Study design | Program description | ACL injuries |
Data analysis methods | PEDro score | ||
|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Intervention | Control | ||||||
| Caraffa et al.25 (1996)* |
Semi-professional and amateur soccer players (not specified whether male or female) | 300 | 300 | Non-randomized cohort study | •Pre-season and playing season program: balance and proprioception exercises; •20 min × 3 per week for season duration. |
10 | 70 | χ2 (p < 0.001) |
2 |
| Hewett et al.11 (1999)* |
High school soccer, volleyball, and basketball players | 366 females | 463 females 434 males |
Non-randomized cohort study | •Pre-season program: stretching, strength, plyometrics; •60–90 min × 3 per week for 6 weeks. |
0 | 6 | χ2 (p < 0.05) |
3 |
| Heidt et al.31 (2000) |
Female high school soccer players | 42 | 258 | RCT | •Pre-season program: cardiovascular conditioning, strength, plyometrics, agility •3 times per week for 7 weeks. |
1 | 8 | Student's t test (p < 0.05) |
4 |
| Soderman et al.35 (2000) |
Female soccer players, average 20 years of age | 121 | 100 | Cluster RCT | •Home-based proprioceptive program using balance boards; •10–15 min daily × 30 days followed by 10–15 min × 3 per week for rest of season. |
4 | 1 | RR with 95%CI (p < 0.05) |
4 |
| Myklebust et al.32 (2003) |
Female handball players | Intervention season 1: 855 Intervention season 2: 850 |
Control Season: 942 | Non-randomized cohort study | •At-practice program: balance exercises (neuromuscular control), planting and cutting and jumping or landing drills; •15 min × 3 per week for 5–7 weeks followed by 15 min per week for rest of season. |
Intervention season 1: 23 Intervention season 2: 17 |
Control season: 29 |
OR (p < 0.05) |
4 |
| Mandelbaum et al.28 (2005)* |
Female soccer players, 14–18 years of age | Year 1: 1041 Year 2: 844 |
Year 1: 1905 Year 2: 1913 |
Non-randomized cohort study | •Warm-up program: stretching, strengthening, plyometrics, agility drills; •20 min program. No other details on frequency or intervention length provided. |
Year 1: 2 Year 2: 4 |
Year 1: 32 Year 2: 35 |
Relative risk with 95%CI (p < 0.05) |
3 |
| Olsen et al.24 (2005)* |
Male and female handball players, 15–17 years of age | 958: 808 females, 150 males |
879: 778 females, 101 males |
Cluster RCT | •Warm-up program: running, strengthening, balance, technique; •15–20 min for 15 consecutive practices followed by 15–20 min per week for rest of season. |
3 | 10 | RR with 95%CI (p < 0.05) |
7 |
| Petersen et al.33 (2005) |
Female handball players | 134 | 142 | Non-randomized cohort study | •At-practice program: balance and jump training; •10 min × 3 per week for 8 weeks (preseason) and 10 min per week during season. |
0 | 5 | OR with 95%CI (p < 0.05) |
2 |
| Pfeiffer et al.34 (2006) |
Female high school soccer, basketball, volleyball players | 577 | 862 | Non-randomized cohort study | • At-practice program:plyometrics and agility drills; •20 min per session. No other details on frequency or intervention length provided. |
3 | 3 | OR with 95%CI (p < 0.05) |
2 |
| Gilchrist et al.37 (2008)* |
Female college soccer players | 583 | 852 | Cluster RCT | •At-practice program: stretching, strength, plyometrics, agility; •3 times per week for 12 weeks. |
2 | 10 |
Z-statistic for RR (p < 0.05) |
4 |
| Pasanen et al.29 (2008) |
Female floorball players | 256 | 201 | Cluster RCT | •At-practice program: running, balance, plyometrics, strengthening, stretching; •20–30 min × 2–3 per week for intensive periods and 20–30 min per week for maintenance. |
4 | 6 | RR with 95%CI (p < 0.05) |
8 |
| Steffen et al.36 (2008) |
Female soccer players, 12–17 years of age | 1073 | 947 | Cluster RCT | •Warm-up program: core stability, balance, dynamic stabilization, and hamstring strength; •20 min for 15 consecutive training sessions and 20 min per week for rest of season. |
4 | 5 |
Z-test with 95%CI RR (p < 0.05) |
7 |
| Kiani et al.26 (2010)* |
Female soccer players, 13–19 years of age | 777 | 729 | Non-randomized cohort study | •At-practice program: warm-up, muscle activation, balance, strength, core stability. •20–25 min × 2 per week in pre-season and 20–25 min per week in- regular season. |
0 | 5 | RR with 95%CI (p < 0.05) | 4 |
| LaBella et al.27 (2011)* |
Female high school soccer and basketball players | 737 | 755 | Cluster RCT | •At-practice program: warm-up, strength, agility, balance, plyometrics, technique instruction; •20 min prior to practices and abbreviated program before games for entire season. |
2 | 6 | χ2 and Fisher exact test, Cochran–Armitage test (p < 0.05) |
6 |
| Walden et al.30 (2012)* |
Female soccer players, 12–17 years of age | 2479 | 2085 | Cluster RCT | •Warm-up program: knee control and core stability, jumping or landing technique; •15 min × 2 per week for whole season. |
7 | 14 | RR with 95%CI (p < 0.05) |
7 |
Abbreviations: ACL = anterior cruciate ligament; CI = confidence interval; OR = odd ratio; RCT = randomized controlled trial; RR = rate ratio.
Indicates that authors found a significant injury reduction effect from intervention.
The methodological quality of each study was assessed with the PEDro scale,16, 17 which has been used commonly for studies investigating ACL prevention program effectiveness. This scale, developed by the Centre of Evidence-Base Physiotherapy, is scored on a 1–10 point scale with a 10 representing excellent methodological quality. There are 11 criteria included in this scale, with the eligibility criteria specification not counted toward the 10-point total. The other 10 items in this scale relate to the study's internal validity and whether the study appropriately reported statistical information such that the results can be interpreted. Examples of these criteria include the presence of blinding (subjects, assessors, or therapists), baseline information of study groups, reporting of key outcomes from a minimum of 85% of the subjects, and reporting of point measures and measures of variability. Thus, reporting the PEDro scores for the included studies in this systematic review served to give the reader context as to the overall methodological quality of this literature that possesses barriers to program implementation.
2.3. Identifying and addressing barriers to program implementation
The primary purpose of this study was to examine the most commonly encountered barriers to implementation of ACL injury prevention programs. We conducted this examination by carefully reading the included articles and recording a list of phrases or sentences that directly or indirectly indicated hindrances to the success of the programs. In order for a hindrance to the success of the program to be considered a barrier, it was required to be mentioned in at least 2 separate studies.
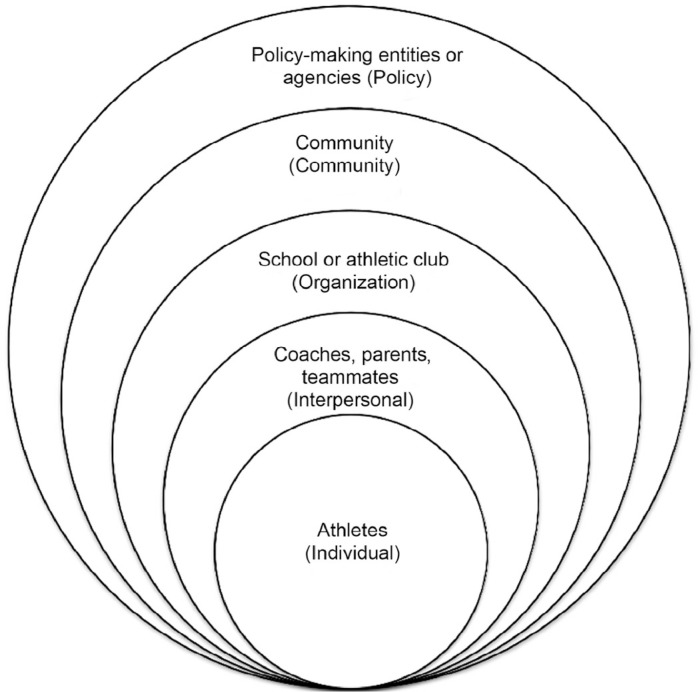
We sought to examine the issue of barriers to implementation of ACL injury prevention programs from a socio-ecological perspective. As a group, we discussed what the 5 levels of influence of the SEM18, 19 represented in the context of athletes avoiding ACL injuries. The SEM contributes to our understanding of this important issue by highlighting the multiple levels at which barriers can occur. We also utilized the SEM as a framework for suggesting ways to reduce the identified barriers to implementation.
The socio-ecological framework explains behavior as being influenced by 5 factors, which are represented by concentric bands.18, 19 The innermost section is the individual or intrapersonal level, which is surrounded by interpersonal, organizational, community, and public policy factors. This approach is commonly used for developing health promotion interventions because it goes beyond just individual influences on behavior and considers an assortment of environmental factors that can also affect behavior. For instance, the Centers for Disease Control and Prevention (CDC) applied the SEM and its multi-level approach to prevention to the development of its colorectal cancer control program.20 Similarly, other health promotion studies have utilized the SEM to analyze contributing factors and develop interventions for an obesity prevention program,21 to increase fruit and vegetable intake,22 and to analyze enablers and inhibiters to physical activity.23
3. Results
3.1. Characteristics of reviewed studies
Table 1 summarizes the characteristics of the 15 included studies. The athletes who participated in the studies played soccer, basketball, volleyball, team handball, or floorball. The Hewett et al.11 and Olsen et al.24 studies involved male and female athletes, Caraffa et al.25 did not indicate the sex of the athletes, and all of the other studies involved only female athletes. All of the studies used one or more of the following training methods: balancing, strengthening, plyometrics, agility drills, and technique instruction. The studies differed as to the athlete population examined, the components of the programs, the length of the programs, the background and training of the program facilitators, and the results.
Eight of the studies were randomized controlled trials and 7 were prospective cohort studies. Eight studies supported a significant effect from the training program,11, 24, 25, 26, 27, 28, 29, 30 6 studies did not show a significant effect,31, 32, 33, 34, 35, 36 and 1 study had a significant effect only in the second part of the season.37 The PEDro scores for the 15 studies are also displayed in Table 1. The average PEDro score for the studies was 4.29 with a high score of 8 and a low score of 2.
3.2. Data synthesis for barriers to program implementation
After examining the data for barriers, 5 barriers emerged, each being mentioned in at least 2 of the reviewed studies. The 5 identified barriers are motivation, time requirements, skill requirements for program facilitators, compliance, and cost. Table 2 details the studies in which these barriers were identified.
Table 2.
Barriers to implementation with citations from studies.
| Barrier | Study quotes |
|---|---|
| Motivation | “Most of the 12 teams that declined to participate after learning about the preventive program expressed skepticism regarding the usefulness of the program as the reason for nonparticipation, which suggests a different attitude toward preventive training.” (Kiani et al.,26 2010, p. 44) “Considerable efforts were made to motivate the intervention teams to include the exercise program as a standard part of their training program. Instructors visited the teams three times during training at the start of the study and again after the summer break, and the teams received balance mats and a brochure detailing the intervention program. Despite this, the intervention teams included the injury prevention program in only 60% of their training sessions during the first half of the season…” (Steffen et al.,36 2008, p. 609) “As we discovered, implementing these types of exercise studies can be challenging because many coaches are unwilling to modify their practice protocols.” (Pfeiffer et al.,34 2006, p. 1773) “Furthermore, it might be difficult to motivate the subjects to perform the training as prescribed and to maintain their motivation at a high level throughout the study period. Therefore, in this investigation the authors (K.D. and S.W.) were in regular contact with the players to try to keep them motivated to perform the balance board training as prescribed. (Soderman et al.,35 2000, p. 361) “…all of the 10 exercises were to be carried out during every 15-min training session, generally without progression or variation. This may have resulted in reduced motivation among coaches and players.” (Steffen et al.,36 2008, p. 611) |
| Time requirements | “…during the competitive season, many of the teams in the present investigation often trained only once or twice weekly. As a consequence of these factors, the ability to include preventive training sessions on a consistent basis may have been limited.” (Steffen et al.,36 2008, p. 611) In the beginning of the present study many coaches were not convinced that the exercises suggested in the initial program may help to prevent injuries. Instead they were concerned that the exercises would steal valuable preseason training time. (Petersen et al.,33 2005, p. 620) “In an effort to design an effective program to prevent noncontact ACL injuries that could readily be used at many levels of play without significant investment in equipment or time, an expert panel was convened by the Santa Monica Orthopedic and Sports Medicine Research Foundation in 1999. This group designed the Prevent injury and Enhance Performance (PEP) Program.” (Gilchrist et al.,37 2008, p. 1477) |
| Skill requirements | “In the intervention a strong emphasis was placed on proper technical performance of every exercise. We considered it important that the intervention coaches and players had good knowledge of the correct training technique, typical mistakes in each exercise manoeuvre, and appropriate methods for their correction.” (Pasanen et al.,29 2010, p. 6) “During the practical demonstration of the exercises, study therapists instructed the coaches carefully on how to clear player to progress to the next level of difficulty—that is, when all repetitions were performed with good neuromuscular control, mainly focusing on core stability and proper knee alignment.” (Walden et al.,30 2012, p. 2) “The instructors had been familiarized with the programme during a two hour seminar, in which they received theoretical and practical training on how to conduct the programme.” (Olsen et al.,24 2005, p. 2) “Older, overweight, and less physically fit coaches tended to include fewer exercises, suggesting that they may have omitted exercises that they could not demonstrate themselves. Compliance may improve if each coach brings an athlete to the training session to learn demonstration of the exercises.” (LaBella et al.,27 2011, p. 1038) |
| Compliance | “In conclusion, we observed no effect of the injury prevention program on the injury rate, most likely because the compliance with the program was low.” (Steffen et al.,36 2008, p. 605) “We were somewhat surprised by the low compliance in the study because the problem of ACL injuries has received a lot of attention from the media and within the handball community. Despite the high incidence of injury, the dire future consequences to knee function in injured players, and close follow-up of the teams by physical therapists, acceptable compliance was achieved in less than half of the players.” (Myklebust et al.,32 2003, p. 76) “Older, overweight, and less physically fit coaches tended to include fewer exercises, suggesting that they may have omitted exercises that they could not demonstrate themselves. Compliance may improve if each coach brings an athlete to the training session to learn demonstration of the exercises.” (LaBella et al.,27 2011, p. 1038) “The high compliance rate in this study suggests that the program is easy to implement and incorporate into regular soccer practice.” (Kiani et al.,26 2010, p. 49) |
| Cost | “The cost of training a group of 15 to 20 coaches was $80 per coach.” (LaBella at al.,27 2011, p. 1036) “In an effort to design an effective program to prevent noncontact ACL injuries that could readily be used at many levels of play without significant investment in equipment or time, an expert panel was convened by the Santa Monica Orthopedic and Sports Medicine Research Foundation in 1999. This group designed the Prevent injury and Enhance Performance (PEP) Program.” (Gilchrist et al.,37 2008, p. 1477) |
Abbreviation: ACL = anterior cruciate ligament.
3.2.1. Motivation
Low motivation to participate can be a substantial barrier to implementation of ACL injury prevention programs. Low motivation from athletes and coaches can result from lack of confidence about the programs' effectiveness. Kiani et al.26 found that some coaches declined to participate because they were skeptical about the effectiveness of the program. Furthermore, low motivation can arise from boredom with the exercises or exercises that are not challenging enough. For example, Steffen et al.36 stated that having their intervention group athletes perform the same 10 exercises in every practice session without varying the exercises or increasing the intensity may have contributed to a decrease in motivation among the athletes and coaches. The authors reported that their preventive program was utilized at 60% of all training sessions in the first half of the season and 44% in the second half of the season. In addition, resistance to change may be a cause of low motivation to participate in injury prevention training programs. Pfeiffer et al.34 noted that many coaches were not willing to change their practice protocols.
3.2.2. Time requirements
Because sports training time is limited and there are various components of training that coaches need to cover with their athletes, the time required to conduct an injury prevention program may be a barrier to regular use of preventive programs. This appears to have been an issue for Steffen et al.36 who conducted their study with teams that practiced once or twice a week and had competitions on weekdays. The authors noted that this kind of schedule made it difficult to consistently include preventive training. Furthermore, Petersen et al.33 stated that some coaches in their study were concerned that the preventive exercises would take up valuable training time.
3.2.3. Skill requirements for program facilitators
Several authors emphasized the importance of technique, reporting that their intervention group participants were taught proper technique for the preventive exercises or encouraged to pay attention to performing the exercises with good form.11, 24, 29, 30, 32, 36 The preparation and physical fitness of the program facilitator may have an impact on the quality of program implementation. LaBella et al.27 observed that certain coaches in their study included fewer of the program exercises. They suggested that these coaches who were overweight or older may have omitted exercises they could not demonstrate. Many of the studies we examined had coaches leading the training programs,24, 26, 27, 28, 30, 36 whereas some had physical therapists or certified athletic trainers,32, 37 and a few had coaches and physical therapists or athletic trainers.1, 29, 33
3.2.4. Compliance
Poor compliance with an injury prevention training program is a barrier to obtaining satisfactory results from the program. Steffen et al.36 attributed the lack of effect in their injury prevention program to insufficient compliance. In their study, the training program was used by intervention group teams in 52% of the practice sessions. Furthermore, Myklebust et al.32 had only a 29% compliance rate in their study. They found this surprising because of the media attention given to the problem of ACL injuries and because they had physical therapists monitor their intervention teams to improve compliance. Both of these studies failed to demonstrate a significant effect from their intervention training programs.
3.2.5. Cost
The cost of ACL injury prevention training programs is another potential barrier. LaBella et al.27 reported that the cost of training the coaches for their study was USD 80 per coach. Additionally, Gilchrist et al.37 discussed the importance of development of programs that did not cost a lot or take too much time. With tighter budgets for schools and community programs in recent years, the cost of equipment, facilitator training, and assistance by health professionals for preventive programs may present a barrier to some teams.
4. Discussion
Through our systematic review of ACL injury prevention programs, we found 5 barriers to implementation. These are motivation, time requirements, facilitator skill requirements, compliance, and cost. As a response to these barriers, we have provided suggestions to reduce them via the SEM model.
4.1. Application of the SEM to program implementation barriers
4.1.1. Individual level
Fig. 2 shows the application of the SEM to team sport athletes. When applying the SEM to ACL injury prevention, the individual level represents the athletes in the program. One way to improve program implementation from an individual level is through ACL injury-related awareness and education, which might help address motivation and compliance barriers. Education and building of awareness should go beyond providing information on ACL injuries. Ideas for effective education about ACL injuries could include opportunities for athletes to interact with each other around the topic (e.g., group projects or discussions), the use of a realistic anatomic model of the knee, and a post-instructional assessment.
Fig. 2.
Representation of Socio-Ecological Model as it applies to athletes.
4.1.2. Interpersonal level
The interpersonal level of the SEM would focus on coaches, parents, and teammates. As with the individual level, awareness and education about ACL injuries is a strategy to improve adoption of training programs among coaches. This could include clearly communicating to coaches and parents that ACL injuries can increase the risk of early-onset osteoarthritis. In addition, camaraderie could be developed among team members by encouraging athletes to work together and watch each other's technique when performing the ACL injury prevention training, similar to practices implemented by Pasanen et al.29
Furthermore, broadening the programs may help improve motivation and compliance. Instead of just an ACL injury prevention program, a program that encompasses prevention of other lower extremity injuries may have wider appeal to coaches, as the risk of a number of injuries can be reduced with 1 training program. Studies such as those conducted by LaBella et al.,27 Pasanen et al.,29 and Olsen et al.24 have indicated that this type of program can be effective.
4.1.3. Organizational level
Ways to improve program implementation at the organizational level include overcoming barriers within schools and athletic clubs. One strategy at this level might be to develop and evaluate versions of injury prevention programs that are as brief as they can be without compromising effectiveness. Kiani et al.26 suggested that their study's high compliance rates might be because their program was easy to incorporate into practice, keeping extra time requirements low. Relatively short, easy-to-use programs could help to overcome resistance from coaches based on using up too much practice time and would keep program costs low.
Another way to reduce barriers at this level is to ensure that program facilitators receive quality preparation for leading the ACL injury prevention training programs. The injury prevention programs are not likely to be successful if the exercises are not performed properly. Therefore, it is important for coaches or athletes leading these programs to obtain training that will adequately prepare them to correctly demonstrate and explain the exercises and monitor technique.
4.1.4. Community level
Reducing barriers to implementation at the community level could focus on institutions beyond the sports team. One possible strategy at this level is to develop moderately priced videos or online tutorials of knee or lower-extremity injury prevention programs. A similar approach has already been utilized by the CDC in their “Heads up: concussion in youth sports” initiative.38 An affordable DVD that is readily available could help to overcome the barriers of prohibitive cost and low motivation to begin a preventive program. A media campaign to increase awareness of the injury prevention video could also be beneficial. Another idea at the community level is to solicit assistance from faculty and students at local universities that have programs such as athletic training, sports science, or physical therapy. These groups could set up or assist with ACL injury prevention programs in local middle schools, high schools, or community sports leagues.
4.1.5. Policy level
Policy level changes could center on state and federal agencies, as well as the views of society regarding sports injury prevention. Policies could be implemented by high school and college athletic associations and state departments of education such as a mandate that schools have a certified athletic trainer on staff, the inclusion of sports injury prevention material in middle school physical education curricula, and the requirement that some injury prevention exercises be included in school sports team training. To increase the willingness of legislators to make policy changes, it would be advantageous to develop evidence-based preventive training programs that effectively reduce risk for several lower extremity injuries (i.e., a program that not only reduces ACL injuries, but also meniscus tears, ankle sprains, and calf muscle strains).
4.2. Strengths and limitations
The primary strength of the present study is that it raises awareness of barriers to implementation for ACL injury prevention programs, which can lead to more discussion, further research, and increased collaboration between researchers, clinicians, and coaches about barriers to implementation and how to overcome them. Our study also has some limitations that are important to note. As expected, the participants in the studies we analyzed tended to share particular characteristics (e.g., almost all females, mostly in their teens or twenties, who played certain sports). Therefore, the study may not be generalizable to other populations. Another limitation of our study is the possibility that some barriers to implementation were not indicated in the studies we reviewed. The current systematic review may also possess bias in that unpublished reports were not included in the review. Typically, unpublished studies are not included in systematic reviews due to the inability to identify and retrieve them or due to poor methodological quality. However, it is conceivable that if some unpublished studies possessed sufficient barriers to program implementation, these studies may not be published due to a perception that these barriers could be a threat to the internal validity of the study. Therefore, our description of barriers to implementation may be incomplete. However, identifying and overcoming barriers to program success will likely be necessary for ACL programs to be effective in reducing the overall incidence of ACL injuries in team sports.
5. Conclusion
Given that ACL incidence rates have not declined over the past 10 years,19 and the burden imposed by ACL injuries, which include an increased risk of early onset osteoarthritis, we believe it would be beneficial to have greater dissemination and utilization of ACL injury prevention programs. Our study highlights the need for future research to examine the most cost-effective and time-efficient training for ACL injury prevention and the effectiveness of the training programs in men as well as women. It would be advantageous to more clearly define the barriers, determine which barriers are the most detrimental, and determine if programs are more readily adopted by the target population when certain barriers are reduced.
Authors' contributions
RLB conducted the literature review, identified relevant studies, analyzed the data, and drafted the manuscript; ASK designed the study, identified relevant studies, analyzed the data, and drafted the manuscript; RJM and ARR assisted with study design, contributed to the interpretation of the data, and drafted the manuscript. All authors have read and approved the final version of the manuscript, and agree with the order of presentation of the authors.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Peer review under responsibility of Shanghai University of Sport.
References
- 1.Hewett T., Ford K., Myer G. Anterior cruciate ligament injuries in female athletes: part 2, a meta-analysis of neuromuscular interventions aimed at injury prevention. Am J Sports Med. 2006;34:490–498. doi: 10.1177/0363546505282619. [DOI] [PubMed] [Google Scholar]
- 2.Maffulli N., Longo U., Gougoulias N., Loppini M., Denaro V. Long-term health outcomes of youth sports injuries. Br J Sports Med. 2010;44:21–25. doi: 10.1136/bjsm.2009.069526. [DOI] [PubMed] [Google Scholar]
- 3.Griffin L., Agel J., Albohm M.J., Arendt E.A., Dick R.W., Garrett W.E. Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg. 2010;8:141–150. doi: 10.5435/00124635-200005000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Morrey M., Stuart M., Smith A., Wiese-Bjornstal D. A longitudinal examination of athletes' emotional and cognitive responses to anterior cruciate ligament injury. Clin J Sport Med. 1999;9:63–69. doi: 10.1097/00042752-199904000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Freedman K., Glasgow M., Glasgow S., Bernstein J. Anterior cruciate ligament injury and reconstruction among university students. Clin Orthop Relat Res. 1998;356:208–212. doi: 10.1097/00003086-199811000-00028. [DOI] [PubMed] [Google Scholar]
- 6.Hewett T., Ford K., Myer G. Anterior cruciate ligament injuries in female athletes: part 1, mechanisms and risk factors. Am J Sports Med. 2006;34:299–308. doi: 10.1177/0363546505284183. [DOI] [PubMed] [Google Scholar]
- 7.Wojtys E., Brower A. Anterior cruciate ligament injuries in the prepubescent and adolescent athlete: clinical and research considerations. J Athl Train. 2010;45:509–512. doi: 10.4085/1062-6050-45.5.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Donnelly C., Elliott B., Ackland T.R., Doyle T.L., Beiser T.F., Finch C.F. An anterior cruciate ligament injury prevention framework: incorporating the recent evidence. Res Sports Med. 2012;20:239–262. doi: 10.1080/15438627.2012.680989. [DOI] [PubMed] [Google Scholar]
- 9.Hutchinson M., Ireland M. Knee injuries in female athletes. Sports Med. 1995;19:288–302. doi: 10.2165/00007256-199519040-00006. [DOI] [PubMed] [Google Scholar]
- 10.Lohmander L., Englund P., Dahl L., Roos E. The long-term consequence of anterior cruciate ligament and meniscus injuries. Am J Sports Med. 2007;35:1756–1796. doi: 10.1177/0363546507307396. [DOI] [PubMed] [Google Scholar]
- 11.Hewett T., Lindenfeld T., Riccobene J., Noyes F. The effect of neuromuscular training on the incidence of knee injury in female athletes. Am J Sports Med. 1999;27:699–706. doi: 10.1177/03635465990270060301. [DOI] [PubMed] [Google Scholar]
- 12.U.S. Department of Health and Human Services Healthy people 2020. 2010. www.healthypeople.gov Available at. [accessed 03.01.2013]
- 13.Hootman J., Albohm M. Anterior cruciate ligament injury prevention and primary prevention of knee osteoarthritis. J Athl Train. 2012;47:589. doi: 10.4085/1062-6050-47.5.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shultz S., Schmitz R., Benjaminse A., Chaudhari A., Collins M., Padua D. ACL research retreat VI: an update on ACL injury risk and prevention. J Athl Train. 2012;47:591–603. doi: 10.4085/1062-6050-47.5.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moher D., Liberati A., Tetzlaff J., Altman D.G., PRISMA Group Reprint—preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Phys Ther. 2009;89:873–880. [PubMed] [Google Scholar]
- 16.Centre for Evidence-Based Physiotherapy Physiotherapy Evidence Database (PEDro) 2012. http://www.pedro.org.au Available at. [accessed 03.01.2013]
- 17.Maher C., Sherrington C., Herbert R., Moseley A., Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83:713–721. [PubMed] [Google Scholar]
- 18.McLeroy K., Bibeau D., Steckler A., Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;14:351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- 19.Richard L., Potvin L., Kishchuk N., Green L. Assessment of the integration of the ecological approach in health promotion programs. Am J Health Promot. 1996;10:318–328. doi: 10.4278/0890-1171-10.4.318. [DOI] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention (CDC) Colorectal CancerControl Program. 2013. http://www.cdc.gov/cancer/crccp/sem.htm Available at. [accessed 03.01.2013]
- 21.Pratt C.A., Lemon S.C., Fernandez I.D., Goetzel R., Beresford S.A., French S.A. Design characteristics of worksite environmental interventions for obesity prevention. Obesity (Silver Spring) 2007;15:2171–2180. doi: 10.1038/oby.2007.258. [DOI] [PubMed] [Google Scholar]
- 22.Robinson T. Applying the socio-ecological model to improving fruit and vegetable intake among low-income African Americans. J Community Health. 2008;33:395–406. doi: 10.1007/s10900-008-9109-5. [DOI] [PubMed] [Google Scholar]
- 23.Siddiqi Z., Tiro J., Shuval K. Understanding impediments and enablers to physical activity among African American adults: a systematic review of qualitative studies. Health Educ Res. 2011;26:1010–1024. doi: 10.1093/her/cyr068. [DOI] [PubMed] [Google Scholar]
- 24.Olsen O., Mykelbust G., Engelbretsen L., Holme I., Bahr R. Exercises to prevent lower limb injuries in youth sports: cluster randomized controlled trial. BMJ. 2005;330:449. doi: 10.1136/bmj.38330.632801.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Caraffa A., Cerulli G., Projetti M., Aisa G., Rizzo A. Prevention of anterior cruciate ligament injuries in soccer. Knee Surg Sports Traumatol Arthrosc. 1996;4:19–21. doi: 10.1007/BF01565992. [DOI] [PubMed] [Google Scholar]
- 26.Kiani A., Hellquist E., Ahlqvist K., Gedeorg R., Michaelsson K., Byberg L. Prevention of soccer-related knee injuries in teenaged girls. Arch Intern Med. 2010;170:43–49. doi: 10.1001/archinternmed.2009.289. [DOI] [PubMed] [Google Scholar]
- 27.LaBella C., Huxford M., Grissom J., Kim K., Peng J., Christoffel K. Effect of neuromuscular warm-up on injuries in female soccer and basketball athletes in urban public high schools. Arch Pediatr Adolesc Med. 2011;166:1033–1040. doi: 10.1001/archpediatrics.2011.168. [DOI] [PubMed] [Google Scholar]
- 28.Mandelbaum B.R., Silvers H.J., Watanabe D.S., Knarr J.F., Thomas S.D., Griffin L.Y. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes. Am J Sports Med. 2005;33:1003–1010. doi: 10.1177/0363546504272261. [DOI] [PubMed] [Google Scholar]
- 29.Pasanen K., Parkkari J., Pasanen M., Hiilloskorpi H., Mäkinen T., Järvinen M. Neuromuscular training and the risk of leg injuries in female floorball players: cluster randomized controlled study. BMJ. 2008;337:a295. doi: 10.1136/bmj.a295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Walden M., Atroshi I., Magnusson H., Wagner P., Hagglund M. Prevention of acute knee injuries in adolescent female football players: cluster randomized controlled trial. BMJ. 2012;344:e3042. doi: 10.1136/bmj.e3042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Heidt R., Sweeterman L., Carlonas R., Traub J., Tekulve F. Avoidance of soccer injuries with preseason conditioning. Am J Sports Med. 2000;28:659–662. doi: 10.1177/03635465000280050601. [DOI] [PubMed] [Google Scholar]
- 32.Myklebust G., Engebretsen L., Braekken I., Skjolberg A., Olsen O., Bahr R. Prevention of anterior cruciate ligament injuries in female team handball players: a prospective intervention study over three seasons. Clin J Sport Med. 2003;3:71–78. doi: 10.1097/00042752-200303000-00002. [DOI] [PubMed] [Google Scholar]
- 33.Petersen W., Braun C., Bock W., Schmidt K., Weimann A., Drescher W. A controlled prospective case control study of a prevention training program in female team handball players: the German experience. Arch Orthop Trauma Surg. 2005;125:614–621. doi: 10.1007/s00402-005-0793-7. [DOI] [PubMed] [Google Scholar]
- 34.Pfeiffer R., Shea K., Roberts D., Grandstrand S., Bond L. Lack of effect of a knee ligament injury prevention program on the incidence of noncontact anterior cruciate ligament injury. J Bone Joint Surg. 2006;88:769–776. doi: 10.2106/JBJS.E.00616. [DOI] [PubMed] [Google Scholar]
- 35.Soderman K., Werner S., Pietila T., Engstrom B., Alfredson H. Balance board training: prevention of traumatic injuries of the lower extremities in female soccer players? Knee Surg Sports Traumatol Arthrosc. 2000;8:356–363. doi: 10.1007/s001670000147. [DOI] [PubMed] [Google Scholar]
- 36.Steffen K., Myklebust G., Olsen O., Holme I., Bahr R. Preventing injuries in female youth football—a cluster-randomized controlled trial. Scand J Med Sci Sports. 2008;18:605–614. doi: 10.1111/j.1600-0838.2007.00703.x. [DOI] [PubMed] [Google Scholar]
- 37.Gilchrist J., Mandelbaum B.R., Melancon H., Ryan G.W., Silvers H.J., Griffin L.Y. A randomized controlled trial to prevent noncontact anterior cruciate ligament injury in female collegiate soccer players. Am J Sports Med. 2008;36:1476–1483. doi: 10.1177/0363546508318188. [DOI] [PubMed] [Google Scholar]
- 38.Centers for Disease Control and Prevention Heads up: concussion in youth sports initiative. 2012. http://www.cdc.gov/concussion/HeadsUp/youth.html Available at. [accessed 03.01.2013]