Abstract
Background
Lipoblastoma is a rare, benign, fatty tissue tumor that occurs in infancy and early childhood. The most common tumor locations are the extremities and the torso. The location of this tumor in the chest wall and an intrathoracic extension is uncommon.
Case report
We present a case of a 3-year-old boy with anterior chest wall lipoblastoma with an intrathoracic extension. Computed tomography was suggestive of lipoblastoma. The mass was completely excised through a right posterolateral thoracotomy. The histologic examination of the lesion confirmed the diagnosis of lipoblastoma.
Conclusion
Although extremely rare, chest wall lipoblastoma should be included in the differential diagnosis of thoracic mass in childhood.
Keywords: Lipoblastoma, Chest wall, Thoracic mass, Children
1. Background
Lipoblastoma is a rare benign tumor of adipose tissue that occurs almost always in infancy and early childhood. It is typically located in the extremities and the torso and less frequently in the head–neck region, mediastinum, and retroperitoneum. Lipoblastoma is a tumor with good prognosis despite the potential for local invasion and rapid growth. Despite the benign biological behavior of the tumor, it may become symptomatic by compressing adjacent organs and tissues. Complete surgical excision is the best therapeutic option to prevent recurrences.
2. Case presentation
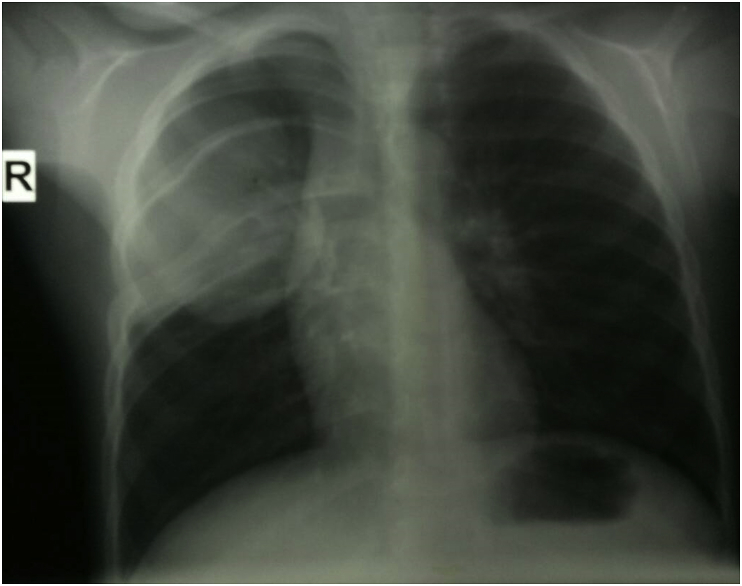
A 3-year-old boy was referred to our clinic for further investigation of a mass in the right hemithorax. Present illness started 5 days ago with fever, cough and wheeze that complicated with and signs of respiratory distress (tachypnea, intercostal retractions) two days later. A chest X-ray was performed showing a giant soft tissue, well-demarcated, well – demarked mass in the right hemithorax expanding and splaying the adjacent ribs, Fig. 1. The mass was an incidental finding in the chest X-ray, as the mass was not visible, nor palpable on examination. Complete Blood Count examination was within normal limits. Signs of respiratory distress gradually resolved after the administration of inhaled bronchodilators and systemic steroids (methylprednisolone). Contrast enhanced CT images revealed a large lobulated, well defined, predominantly fatty mass originating from the chest wall. The lesion was seen to be invading between the ribs with extension into the thorax and into the overlying muscles of the thoracic wall. Inside the fatty mass there where thick enhancing septations with some nodularity. There were no calcifications. Fig. 2.
Fig. 1.
Chest X-Ray: There is a giant soft tissue, well-demarcated, lobulated mass in the right hemithorax expanding and splaying the adjacent ribs.
Fig. 2.
Contrast enhanced CT Images in axial and coronal planes show a large predominantly fatty mass containing thick internal enhancing septations with some nodularity. The mass is situated in the right posterolateral thoracic wall and is seen to be invading between the ribs with extension into the overlying muscles of the thoracic wall.
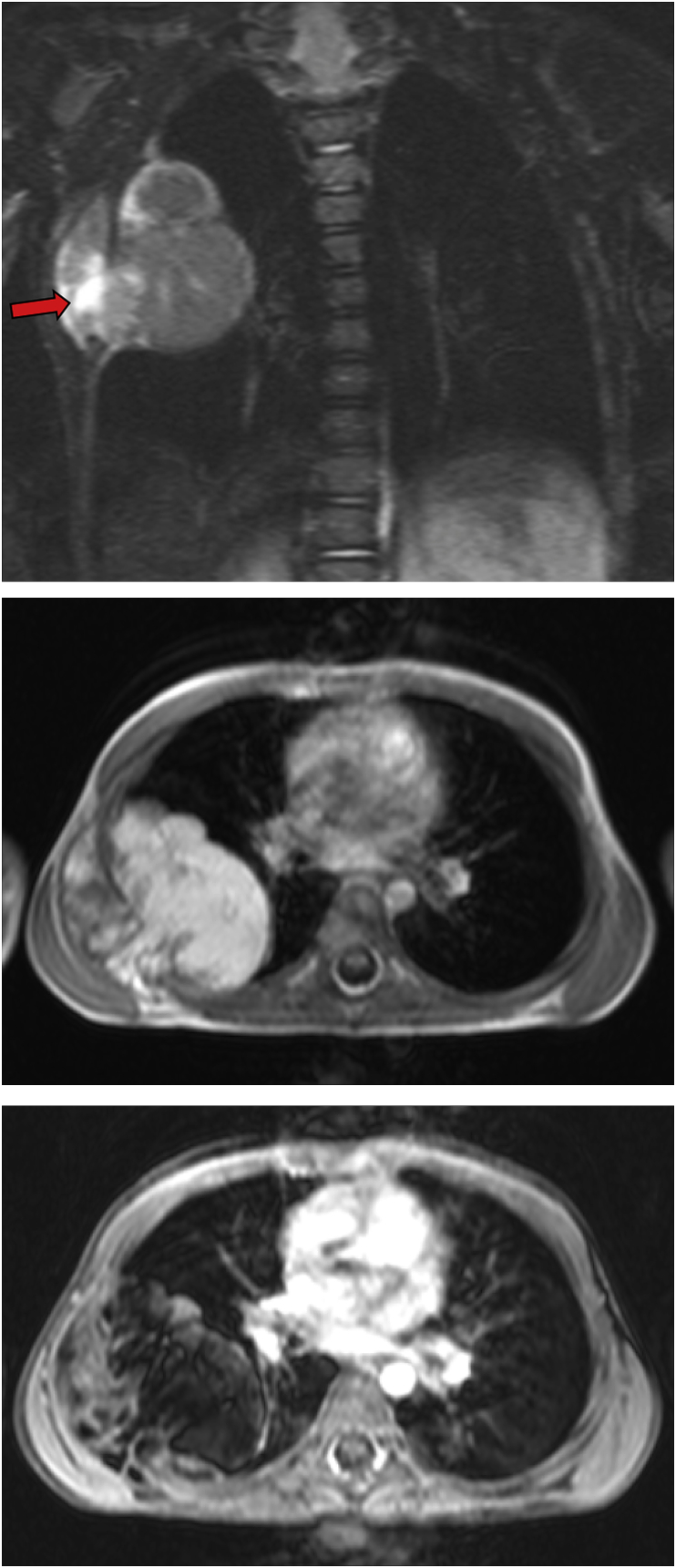
Abdominal ultrasound was performed with normal findings. Magnetic Resonance Imaging (MRI) showed a large heterogeneous, lobulated mass in the right posterolateral thoracic wall, measuring 7,1 × 6,3 × 6,8cm. The mass contained mainly high-signal; material identical to that of subcutaneous adipose tissue in all sequences. Inside the mass there were low-signal, non-enhancing streaks probably representing fibrous tissue. There was also a mild enhancing area with high signal on T2 images probably representing myxoid cystic changes. Fig. 3. I n this patient age group the imaging findings were highly suggestive of thoracic wall lipoblastoma. Biopsy of the extrathoracic part of the tumor confirmed the diagnosis of also revealed lipoblastoma. A week later, excision of the tumor through a right posterolateral incision at the level of the fifth rib took place. The arch of the 5th rib was removed and the extrapleural part of the mass was excised. The pleura was opened and the intrapleural part of the tumor was exposed extending from the apex of the right lung to the level of the 7th rib and to the midline. The upper and the medial lobe of the lung were compressed towards the midline. Gradual removal of the tumor due to its friability took place. Finally, full excision of the tumor was managed, the lung was decompressed and a thoracic drain was left at the area of the removed mass.
Fig. 3.
MRI scan with i.v. contrast demonstrate a large heterogeneous heterogenous mass that is predominantly isointense relative to subcutaneous fat in all sequences. Inside the mass there are thick septations probably representing fibrous tissue. There are also areas of soft tissue attenuation and with high signal intensity on T2 WI probably representing myxoid tissue (arrow).
Postoperatively, the patient was stable and had an uncomplicated course. He was discharged on the 7th postoperative day with instructions. Three and six months later, on the follow up visit the boy was asymptomatic.
3. Discussion
Lipoblastoma is a rare, benign tumor of the embryonic fat tissue [1]. It was first described by Jaffe in 1926. In 1958 Vellios et al. described 2 histopathologic types. The first is a localized, superficial and well-circumscribed or encapsulated lesion called lipoblastoma. The second is a diffuse, multicentric, un-encapsulated and infiltrative form called lipoblastomatosis [2].
The majority of the tumors occur in infancy and early childhood, 90% arise before the age of 3 years old; it is more common among males with a male to female ratio of 1.5–3:1. The tumor is most commonly located in the extremities and the torso, areas where immature adipose elements persist. Tumors located in the head, neck, mediastinum and chest wall are rare. Anterior chest wall lipoblastoma with an intrathoracic extension as described in the present case is extremely uncommon [3].
Clinically, lipoblastoma presents as a painless subcutaneous soft tissue mass characterized by rapid growth and discrete local recurrence rate (14%–25%), which sometimes requires multiple excisions. Symptoms vary depending on the location of the primary tumor. Whereas lipoblastoma of other parts of the body is usually asymptomatic, thorax cases are generally symptomatic. In chest wall lipoblastoma findings may include recurrent respiratory infections, cough and dyspnea; in such cases airway compression leads to poor airway clearance that may eventually predispose to infections. Symptoms resulting from vascular or spinal cord compression have been reported but are extremely rare.
On conventional chest radiography, lipoblastoma appears as a nonspecific, soft-tissue density mass. Whyte and Powell report that the findings on a chest radiograph depend on tumor size, thickness, and location. Usually, there is neither calcium deposition nor adjacent bone erosion because the tumor grows too fast. In our case chest radiograph showed a soft-tissue density mass with adjacent bone deforestation due to pressure.
Both CT and MRI are excellent tools for determining the origin of the tumor, its anatomical extent and composition. The imaging appearances highly depend on the composition of the lesion and in particular the proportion of adipose tissue versus myxoid stroma as well as the presence of internal fibrous tissue, vascular bundles and soft tissue nodules. In infants and young children myxoid components are more prominent, whereas in older children the predominant tissue is fat [4].
CT allows direct identification of the fatty components as well as intratumoral thick septa with some nodularity and mild enhancement representing mainly fibrous tissue [5]. MRI characterizes the internal structure of the lesion in more detail. Fatty components are seen as areas of signal intensity identical to that of subcutaneous adipose tissue with all sequences. Myxoid cystic changes are low signal intensity with T1-weighted sequences and high signal intensity with T2-weighted sequences reflecting high water content. Fibrous tissue is seen as internal mildly enhancing septations. Small enhancing soft tissue nodules are sometimes seen [6].The differential diagnosis includes other fat-containing tumors in particular lipoma, liposarcoma and teratoma [7]. The presence of soft tissue components and cystic changes distinguishes lipoblastoma from lipoma. Regarding liposarcoma and particularly myxoid liposarcoma, there are no known imaging features that can reliably differentiate the two entities. The age of the patient is crucial as liposarcomas are extremely rare prior to ten years of age. Teratomas often contain readily detectable calcification or ossification, which is not a feature of lipoblastoma.
Diagnosis is established only by the histologic examination [8]. In our case the histologic examination was typical of lipoblastoma. It demonstrated adipocytes in different stages of maturation without anaplasia. The main histologic features of the tumor were multinodular and myxoid foci.
Regardless of the location of the tumor, surgical excision is the treatment of choice. Complete resection yields an excellent prognosis, as it is fundamental to prevent local recurrence. Metastases and malignant transformation have not been reported 1.
In conclusion, chest wall lipoblastoma is a rare benign tumor in children. The presence of soft tissue components and cystic changes in a predominantly fatty mass should alert to the possibility of lipoblastoma and However, it should be considered in the differential diagnosis of a rapid growing fatty tumor, because it may become life threatening. Total surgical excision is important and gives good results. Due to discrete local recurrence rate of the tumor a regular follow-up is necessary.
4. Summary
Lipoblastoma is a rare, benign tumor of the embryonic fat tissue tumor that occurs in infancy and early childhood. We present a case of a 3-year-old boy with anterior chest wall lipoblastoma with an intrathoracic extension. Computed Tomography and Magnetic Resonance Imaging was suggestive of lipoblastoma. The mass was completely excised and the histologic examination confirmed the diagnosis. Chest wall lipoblastoma should be included in the differential diagnosis of thoracic mass in childhood.
Consent
Informed consent was obtained from the patient's parents for publication and use of imaging. A copy of the written consent is available for review.
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
References
- 1.Benato C., Falezza G., Lonardoni A., Magnanelli G., Ricci M., Gilioli E., Calabr F. Acute respiratory distress caused by a giant mediastinal lipoblastoma in a 16-month-old boy. Ann. Thorac. Surg. 2011;92(6):e119–e120. doi: 10.1016/j.athoracsur.2011.06.019. [DOI] [PubMed] [Google Scholar]
- 2.Harrer J., Hammon G., Wagner T., Bolkenius M. Lipoblastoma and lipoblastomatosis: a report of two cases and review of the literature. Eur. J. Pediatr. Surg. 2001;11(5):342–349. doi: 10.1055/s-2001-18544. [DOI] [PubMed] [Google Scholar]
- 3.Salem R., Zohd M., Njim L., Maazoun K., Jellali M.A., Zrig A., Mnari W., Harzallah W., Nouri A., Zakhama A., Golli M. Lipoblastoma: a rare lesion in the differential diagnosis of childhood mediastinal tumors. J. Pediatr. Surg. 2011;46(5):e21–e23. doi: 10.1016/j.jpedsurg.2011.01.030. [DOI] [PubMed] [Google Scholar]
- 4.Moholkar S., Sebire N.J., Roebuck D.J. Radiological-pathological correlation in lipoblastoma and lipoblastomatosis. Pediatr. Radiol. 2006;36(8):851–856. doi: 10.1007/s00247-006-0175-5. [DOI] [PubMed] [Google Scholar]
- 5.Glazer H.S., Wick M.R., Anderson D.J., Semenkovich J.W., Molina P.L., Siegel M.J., Sagel S.S. CT of fatty thoracic masses. Am. J. Roentgenol. 1992;159(6):1181–1187. doi: 10.2214/ajr.159.6.1442378. [DOI] [PubMed] [Google Scholar]
- 6.Chen C.W., Chang W.C., Lee H.S., Ko K.H., Chang C.C., Huang G.S. MRI features of lipoblastoma: differentiating from other palpable lipomatous tumor in pediatric patients. Clin. Imaging. 2010;34(6):453–457. doi: 10.1016/j.clinimag.2009.11.009. [DOI] [PubMed] [Google Scholar]
- 7.Brisse H., Orbach D., Klijanienko J., Fréneaux P., Neuenschwander S. Imaging and diagnostic strategy of soft tissue tumors in children. Eur. Radiol. 2006;16(5):1147–1164. doi: 10.1007/s00330-005-0066-4. [DOI] [PubMed] [Google Scholar]
- 8.Ching A.S.C., Lee S.F., Chan Y.L. Diagnosing paediatric mediastinal lipoblastoma using ultrasound-guided percutaneous needle biopsy: review and report. Clin. Imaging. 2002;26(1):23–26. doi: 10.1016/s0899-7071(01)00339-4. [DOI] [PubMed] [Google Scholar]