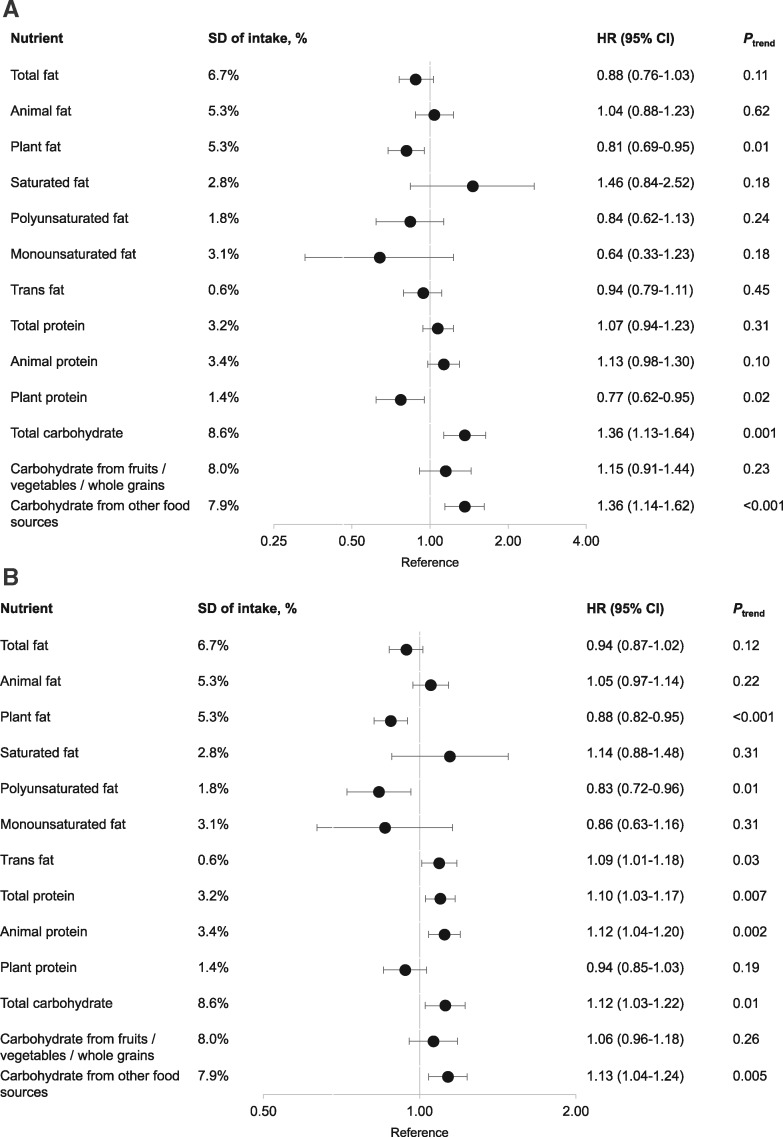
Figure 1.
Association of postdiagnostic macronutrient intake and colorectal cancer (CRC)-specific mortality (A) and all-cause mortality (B) among CRC patients in the Nurses’ Health Study and the Health Professionals Follow-up Study cohorts. Multivariable-adjusted hazard ratios (HRs) and 95% confidence intervals (CI) per one-SD increment in intake, expressed as percentage of total energy intake, are presented on the axis with log(2) scale. The HRs were derived from the Cox proportional hazards regression model stratified by sex and adjusted for age at diagnosis (continuous), cancer stage (I, II, III, and unspecified), year of diagnosis (continuous), subsite (proximal colon, distal colon, rectum, and unspecified), prediagnostic intake of the nutrient under analysis (continuous), postdiagnosis intake of total calories (continuous), alcohol consumption (<0.15, 0.15–1.9, 2.0–7.4, ≥7.5 g/d), pack-years of smoking (0, 1–15, 16–25, 26–45, >45), BMI (<23, 23–24.9, 25–27.4, 27.5–29.9, ≥30 kg/m2), physical activity (women: <5, 5–11.4, 11.5–21.9, ≥22 MET-h/wk; men: <7, 7–14.9, 15–24.9, ≥25 MET-h/wk), regular use of aspirin (yes or no), and total fiber intake (in quartiles). For the analysis of fat and carbohydrate, we further adjusted for postdiagnostic protein intake (continuous); for the analysis of protein, we further adjusted for postdiagnostic total fat intake. Animal and plant fat were adjusted for each other; animal and plant protein were adjusted for each other; carbohydrates from fruits, vegetables, whole grains, and other food sources were adjusted for each other.