Abstract
Invertebrates are often overlooked as laboratory animals, yet they are commonly used in toxicology, developmental, cellular and molecular biology, and radiation studies with euthanasia as an endpoint. Little is known regarding appropriate euthanasia methods for invertebrate species, particularly for Artemia. Here, we evaluated the AVMA-recommended 2-step method of euthanasia in brine shrimp (Artemia franciscana). Artemia were exposed first to anesthetic solutions of 60% alcohol, 2.5 mg/L eugenol, or 4 g/L tricaine methanesulfonate (TMS) and then were transferred to euthanasia solutions of 70% alcohol, 95% alcohol, or 10% neutral buffered formalin. We examined time to anesthesia, behavioral response to anesthesia, anesthesia recovery, and time to euthanasia. Our results show that 2.5 mg/L eugenol and 4 g/L TMS inconsistently achieved anesthesia. Although 60% alcohol produced anesthesia, the time to anesthesia varied among replicate groups, and exposure resulted in an increase in abnormal behavior. We therefore do not recommend any of the tested anesthetic solutions for use in Artemia. Although all 3 euthanasia solutions were effective, more research is needed to provide recommendations regarding euthanasia for this species.
Abbreviations: NBF, neutral buffered formalin; TMS, tricaine methanesulfonate
Brine shrimp (Artemia spp.) are branchiopod crustaceans found along coastlines and in salt lakes. They are used in research for toxicology, developmental, cellular and molecular biology, and radiation studies and as food for aquatic laboratory species, including zebrafish.2 At our institution, a pilot experiment showed that 95% alcohol was an effective euthanasia agent but produced abnormal behavior in Artemia, yet 5% alcohol, recommended by the AVMA Guidelines for the Euthanasia of Animals: 2013 Edition (AVMA Guidelines) as a first-step agent for euthanasia of aquatic invertebrates, was ineffective at producing anesthesia.8 Information regarding euthanasia techniques for this species is sparse currently. As our culture becomes more sensitive to the possibility that invertebrates may experience pain and distress, guidelines for humane treatment and euthanasia should be established.
The AVMA Guidelines provide euthanasia recommendations for both terrestrial and aquatic invertebrates.8 Recommendations comprise a 2-step process involving first anesthesia or presumptive death, followed by an adjunct method to either chemically or physically destroy the brain or major ganglia. The use of an adjunct method alone is described as not acceptable. Recommended first-step solutions include eugenol, 1% to 5% ethanol, and magnesium salts, and second-step, adjunct methods include 70% ethanol, formalin, freezing, boiling, or pithing. It is unacceptable to remove invertebrates from water to desiccate, to leave them in unaerated water to become hypoxic, or to use caustic substances or traumatic techniques.8
For testing, we selected 3 first-step (that is, anesthetic) solutions—alcohol, eugenol, and tricaine methanesulfonate (TMS)—in light of their practicality. No data regarding the dosage of these agents for Artemia have been published, and only sparse, widely disparate data are available regarding their dosage in other invertebrate species.
Alcohol may be used as an anesthetic in invertebrates.10,16,24 The mechanism of action is not fully known but is likely multifactorial.19 In mollusks, alcohol inhibits neuronal sodium and calcium channels.21 In crustaceans, there is evidence of neuromuscular junction depression of the excitatory postsynaptic potentials.3,19 Alcohol is cost-effective and easily available. The AVMA Guidelines recommend using 1% to 5% ethanol as the first step in a 2-step euthanasia process and suggest that concentrations above 70% should be used only as a second-step solution.8 Ethanol at a concentration of 10% has been used as an anesthetic in giant tiger shrimp (Penaeus monodon).23
Eugenol is commonly used as an anesthetic in both fish and crustaceans.5 This organic phenol is the main constituent of clove oil and has a low potential for toxicity and side effects. Its mechanism of action in fish is thought to involve the antagonism of vanilloid receptor 1; it also has a demonstrated affinity for GABAA and NMDA glutamate receptors.17 Eugenol is cost-effective and readily available. The AVMA Guidelines recommend using 0.125 mL/L (125 mg/L) for euthanasia or anesthetic induction; lower concentrations should be used for anesthesia alone.8 For anesthesia, a dose range of 0.03 to 1 mL/L (30 to 1000 mg/L) has been recommended for crustaceans.24 A safe dose of eugenol for the sedation of postlarvae of white Indian shrimp (Fenneropenaeus indicus) was 1.3 mg/L; other doses tested were 2.5 and 3.7 mg/L.5 In Norway lobsters (Nephrops norvegicus), a eugenol concentration of 900 μL/L (900mg/L) has been determined to be effective.12
TMS (also known as MS222) is an FDA-approved agent for the anesthesia of fish, amphibians, and other aquatic, cold-blooded animals. It is a sulfonated isomer of benzocaine. The mechanism of action is unconfirmed but is thought to be similar to that of benzocaine, which blocks action potential conductance through voltage-gated sodium channels.27 Although TMS has been suggested to be ineffective in crustaceans,9,13,24 successful anesthesia was shown in ostracods.29 The minimum effective anesthetic dose in the ostracod Eucypris virens was 500 mg/L, with induction times ranging from 20 s to 2.5 min depending on concentration.29 The effective dose for cherry shrimp, Neocardinina denticulate, was determined to be 2500 mg/L in a 20-min bath.20 A well-known reference work recommends a dose of 100 mg/L for the anesthesia of aquatic invertebrates.17 Although more costly than the other agents, a small amount of TMS could be used to euthanize large numbers of Artemia.
Adjunct agents recommended by the AVMA for the second step of the euthanasia process include 70% alcohol, 95% alcohol, and 10% neutral buffered formalin (NBF).8 These agents are all common preservatives used in labs, are cost-effective, and are expected to be compatible with post-euthanasia histology. Because researchers at our institution need to analyze euthanized Artemia histologically, we did not assess other AVMA-recommended methods, such as boiling, freezing, and pithing, in this study.8
The purpose of this study was to determine a method for efficiently euthanizing Artemia by using a 2-step approach. After titrating first-step solutions for anesthetic efficacy, we hypothesized, given our previous experience with 95% alcohol, that 60% alcohol would likely cause abnormal behavior and consequently be deemed unsuitable as a first-step agent. We also hypothesized that TMS and eugenol would provide adequate anesthesia and that eugenol would provide more consistent anesthesia than TMS. Finally, after Artemia were anesthetized by using a first-step solution, we anticipated that 70% alcohol would be inadequate for euthanasia, whereas 95% alcohol and 10% NBF would be effective.
Materials and Methods
Adult A. franciscana (The Aquatic Critter, Nashville, TN) were maintained in 7.5 L artificial seawater (made by using tap water and Instant Ocean [catalog no. SS15-10, Spectrum Brands, Blacksburg, VA]) at 25 °C, salinity of 1.030 g/dL (40 parts per thousand), and pH 8.0. The Artemia were fed spirulina (Whole Foods, Nashville, TN) once daily, and API Stress Coat (85A, Mars Fish Care North America, Chalfont, PA) was added to the water to remove chlorine and chloramines. LED lighting was provided on a 12:12-h light:dark cycle, and moderate aeration was provided at all times. Although our institution does not require an IACUC-approved protocol for invertebrate use, the current research was performed in accordance with the animal use policies and procedures of Vanderbilt University Medical Center. Concentrations of the anesthetic solutions were determined according to the results of the titration trials (described later).
Titration of first-step solutions.
Alcohol.
Using 95% reagent alcohol (85% ethyl alcohol, 5% isopropyl alcohol, 4% methanol; product no. 9500-1, StatLab Medical Products, McKinney, TX) and tap water, we produced solutions containing 5%, 10%, 20%, 30%, 40%, 50%, 60%, and 70% alcohol; therefore, the total ethanol concentration was 53.7% for the 60% alcohol solution. Although our goal was to maintain a similar salinity to the tank water for all anesthetic solutions to diminish stress, salt precipitated out of solutions containing 30% alcohol or more in tank water; in these cases, the precipitated salt formed a gel-like consistency, which was difficult for the Artemia to swim through. For this reason, we mixed alcohol with tap water; Artemia did not differ between tap water and tank water in preliminary experiments. We pipetted 1.5 mL of solution each into 2 wells of a 24-well plate, and 5 Artemia were then placed in each well. The time to anesthesia and any abnormal behaviors were recorded. Anesthesia was defined as a lack of forward motion and lack of response to stimulation by using a probe. Euthanasia was defined as a lack of thoracopod movement for 10 s of observation.
Eugenol.
Eugenol was tested at 1.3 and 2.5 mg/L. For a stock solution, we diluted 99% eugenol (product no. AC119110050, ACROS Organics, Morris, NJ USA) with 95% alcohol, and then with tank water, and stored the resulting solution in an amber bottle at room temperature. The final concentration of alcohol in the 2.5-mg/L dose was 2.4%. We pipetted 1 mL of each solution into each of 2 wells of a 24-well plate, and 5 Artemia were then placed in each well. The time to anesthesia and any abnormal behaviors were recorded.
TMS.
TMS (product no. NC0135573, Tricaine-S, Western Chemical, Ferndale, WA) was diluted to 10 g/L by using tank water and then buffered to pH 7 to 7.5 with sodium bicarbonate (product no. S233-500, Fisher Scientific, Hampton, NH). The solution was then further diluted with tank water to 1, 2, and 4 g/L; resulting solutions were stored in amber bottles at 4 °C. Each solution was allowed to warm to room temperature prior to exposure. We pipetted 1 mL of each solution into each of 2 wells of a 24-well plate, and 5 Artemia were then placed in each well. The time to anesthesia and any abnormal behavior were recorded.
Anesthesia.
Artemia were assigned to 4 groups (n = 30 per group) and placed in solutions of 60% alcohol, 4 g/L TMS, 2.5 mg/L eugenol, or tank water (control). In each of six 24-well plates, 20 wells contained either 1 mL of an anesthetic solution or tank water according to a permuted plate randomization (Figure 1). We then used a transfer pipet to add a single Artemia to each well. A maximum of 50 μL of tank water was moved with each shrimp, to minimize dilution of the solution. A treatment-blinded observer used a wooden probe to confirm anesthesia, which was defined as a lack of forward motion and lack of response to the probe. Time to anesthesia was recorded for each animal, with a cut-off time of 60 min. After 5 min of anesthesia, the Artemia were transferred to a euthanasia solution.
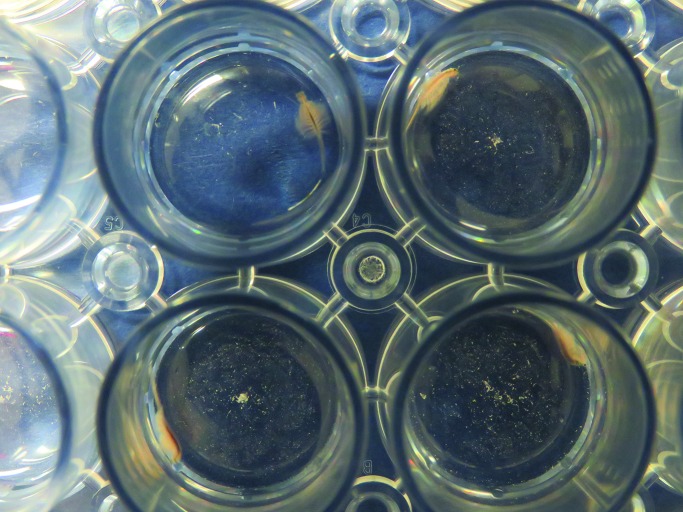
Figure 1.
Artemia were placed in 1 mL of anesthetic solution in a 24-well plate according to a permuted plate randomization design.
Euthanasia.
Anesthetized Artemia were divided into subgroups of 10; each subgroup was transferred to a euthanasia solution: 70% alcohol (product no. 7070-1, StatLab), 95% alcohol (product no. 9500-1, StatLab), or 10% NBF (product no. 28600-5, StatLab). Time to euthanasia, defined as a lack of thoracopod movement for 10 s of observation, was recorded.28
Behavioral scoring.
Behavior during the first 5 min in the anesthetic solution was scored by a treatment-blinded observer. One point each was given for abnormal posturing, hyperactivity, or seizure-like behavior, for a score of 0 to 3; 0, no abnormal behavior; 1, mild; 2 or greater, severe abnormal behavior.
Anesthesia, euthanasia, and behavior scoring were tested in triplicate on separate days.
Recovery from anesthesia.
Artemia (n = 10) from each anesthetic group were anesthetized in a 24-well plate as described earlier. After 5 min of anesthesia, they were rinsed by placing them in a well of tank water and were immediately transferred into a second well of tank water to assess their ability to recover over a 2-h period. Recovery was considered to be achieved on regaining forward motion. This experiment was repeated in triplicate (total, n = 90).
Replication of eugenol anesthesia.
During the original experimental period, eugenol consistently induced anesthesia, as shown in the Results section. Approximately 4 mo later, we attempted to repeat anesthetic induction of Artemia and were unable to obtain similar results with 2.5 mg/L eugenol. Troubleshooting was performed, including purchasing a new bottle of eugenol. We began a series of titrations of eugenol to determine what concentration would produce results similar to our previous experiment. Four titrations of eugenol were performed over a 7 mo period to account for possible seasonal variation. Eugenol was prepared as described earlier: 99% eugenol was first diluted with 95% alcohol and then further diluted with tank water. Each solution was plated in duplicate by pipetting 1 mL into 2 wells of a 24-well plate, and 5 Artemia were then placed in each well. Concentrations tested included 0.125, 1.3, 2.5, 13, 25, 75, and 130 mg/L; the total alcohol concentration in the 130-mg/L dose was 12.4%. As a control, 2 wells of 60% alcohol each containing 5 Artemia were tested also. The time to anesthesia was recorded.
Statistical analyses.
Kaplan–Meier survival and cumulative morbidity curves were drawn for each treatment group, and differences were analyzed by using log-rank statistics for anesthesia and euthanasia, respectively. Proportional odds logistic regression was used to determine cumulative odds ratios of abnormal behavior between groups. The Kruskal–Wallis ANOVA was used to compare behavior scores between groups. Logistic regression analysis was used to compare the significance of anesthetic recovery rates among the 3 anesthetic groups. One-way ANOVA was used to determine significance of replication anesthetic times of alcohol. A P value of less than or equal to 0.05 was considered significant. Statistical analyses were performed by using Stata version 14 (StataCorp, College Station, TX) or Prism 7.03 (GraphPad Software, La Jolla, CA).
Results
One Artemia in the eugenol group and 3 in the TMS group were removed from the study results, due to recording errors.
Titration of first-step solutions.
Alcohol.
No anesthesia of Artemia was observed within 60 min of exposure at concentrations less than 30%. Time to anesthesia decreased from 30 min at 40% to 10 min at 60% with no obvious difference in behavior. We therefore used 60% alcohol as the test concentration.
Eugenol.
Time to anesthesia decreased from 30 min at 1.3 mg/L eugenol to approximately 5 min at 2.5 mg/L with no obvious difference in behavior. We therefore used 2.5 mg/L eugenol as the concentration. Because 2.5 mg/L produced adequate, fast anesthesia, no additional concentrations were tested prior to study initiation. However, in subsequent experiments, anesthesia of Artemia could not be achieved with eugenol, even at concentrations as high as 130 mg/L.
TMS.
No anesthesia was observed within 60 min of exposure at concentrations of 1 or 2g/L; approximately 70% of Artemia became anesthetized at 4 g/L. Given the doses in the literature20,17,29 higher concentrations seemed excessive, and we therefore tested 4 g/L TMS in this study.
Anesthesia.
Artemia were placed in tank water, 2.5 mg/L eugenol, 4 g/L TMS, or 60% alcohol to assess time to anesthesia. Kaplan–Meier plots of the time to anesthesia (Figure 2 A) revealed marked differences (P < 0.0000) between treatments. Eugenol was excluded due to the inability to repeat anesthesia. TMS successfully anesthetized only 63% of the subjects. In addition, 5 of the 90 control animals were recorded as anesthetized; however, these shrimp were likely in poor health and died during the experiment. The average time to anesthesia was 7.2 min for 60% alcohol and 35.5 min for TMS.
Figure 2.
(A). TMS achieved anesthesia in 63% of Artemia; 60% alcohol achieved anesthesia in nearly 100%. Time to anesthesia differed significantly (P = 0.0000) among all groups. (B). Survival curves for euthanasia after anesthesia show 100% probability of death for all groups. All 3 solutions achieved euthanasia, but 95% alcohol led to the fastest euthanasia. (C). Total euthanasia time from placement into anesthetic, 5 min of anesthesia time, until euthanasia in the second-step solution. Euthanasia was fastest by using 60% alcohol followed by 95% alcohol.
Euthanasia.
As part of the 2-step euthanasia process, after 5 min of confirmed anesthesia, Artemia were placed in 70% alcohol, 95% alcohol, or 10% NBF for euthanasia. The time to euthanasia was recorded both as total time from entry into the anesthetic solution and the time to euthanasia after entry into the euthanizing solution. All subjects that entered a euthanasia solution became euthanized. Kaplan–Meier survival estimates of the time to euthanasia (Figure 2 B) revealed marked differences (P < 0.0000) between groups regardless of the anesthetic used, with 95% alcohol providing the fastest euthanasia times for all 3 anesthetics. The total times of euthanasia (from entry into the anesthetic solution, including 5 min of anesthesia, until euthanasia in the second-step solution) for all 2-step combinations are shown in Figure 2 C. In addition, 26.7% of Artemia exposed to 60% alcohol were considered euthanized prior to entry into a euthanasia solution. This result was in comparison to only 14.4% of deaths in eugenol and 1.1% in TMS. The combination of 60% alcohol for anesthesia with 95% alcohol for euthanasia provided the fastest 2-step euthanasia process, with an average time of 13.9 min.
Behavioral scoring.
To assess the potential stress of exposure to the anesthetic solutions, Artemia were observed during the first 5 min of exposure to tank water, 2.5 mg/L eugenol, 4g/L TMS, or 60% alcohol. Each animal was scored for the presence of abnormal behaviors, specifically abnormal posturing, hyperactivity, and seizure-like behavior. One point was given for each abnormal behavior noted, for a combined score of 0 to 3. In comparison to no treatment (tank water control), alcohol caused significantly (P = 0.023) more abnormal behaviors (Figure 3), whereas eugenol caused fewer (P = 0.0005). Abnormal behavior in the TMS group did not differ significantly from the control group. The cumulative odds of abnormal behavior after alcohol treatment was approximately twice that of the control group; in the eugenol group the cumulative odds of abnormal behavior was one third that of control animals (Table 1).
Figure 3.
The incidence of abnormal behavior scores was significantly (*, P = 0.023) greater in the alcohol group compared with the control group. These behaviors were significantly (+, P = 0.0005) reduced in the eugenol group compared with the control group.
Table 1.
Cumulative odds ratios for abnormal behaviors
| Group | Odds ratio | 95% CI |
| Control | 1.0a | |
| 60% alcohol | 1.983779 | 1.1–3.5 |
| 2.5 mg/L eugenol | 0.3135952 | 0.16–0.61 |
| 4 g/L TMS | 0.5874129 | 0.32–1.1 |
These data indicate that 60% alcohol is twice as likely to cause abnormal behaviors and eugenol approximately 30% less likely to cause abnormal behavior relative to no treatment (control group).
Reference group
Recovery from anesthesia.
To assess the ability of Artemia to recover from anesthesia within a 2-h period, Artemia were anesthetized for 5 min in 2.5 mg/L eugenol, 4 g/L TMS, or 60% alcohol; rinsed; and then placed in tank water to recover. In comparison to alcohol, TMS was significantly (P = 0.032) more likely to result in recovery with 80% recovering within 2 h compared with 53.3% for those in alcohol. Results from eugenol are not shown, due to the inability to repeat anesthesia.
Replication of eugenol anesthesia.
Subsequent trials using eugenol over a 7-mo period failed to reproduce reliable anesthesia in Artemia. At 130 mg/L, only 20% of Artemia reached an anesthetized state during any given trial. To compare results between groups more accurately, 60% alcohol was used as a standard in each eugenol trial. Whereas 60% alcohol consistently produced anesthesia within 60 min, the time to anesthesia was significantly (P < 0.0001) prolonged when compared with previous results. In particular, 60% alcohol previously had an average anesthesia time of 7.2 min (n = 90), but the time for each subsequent trial (n = 10 per trial) was 19.3 (P < 0.0001), 14.6 (P < 0.0054), 22.6 (P < 0.0001), and 35.7 (P < 0.0001) min.
Discussion
We performed the current study to establish a reliable 2-step method of euthanasia for Artemia by using recommendations by the AVMA Guidelines. The results support our hypothesis that 60% alcohol would cause abnormal behavior and therefore is poorly suitable as a first-step, anesthetic agent. In our first experiment, eugenol provided more consistent anesthesia than TMS, but the overall results do not support our hypothesis that TMS and eugenol would provide adequate anesthesia: neither agent reliably induced anesthesia in Artemia. Lastly, we incorrectly hypothesized that 70% alcohol would be inadequate for euthanasia for anesthetized Artemia. In contrast to our expectation, all 3 second-step solutions tested (70% alcohol, 95% alcohol, and 10% NBF) were effective as euthanasia agents.
Most regulations do not specifically protect invertebrate animals, although the general consensus is that they should be treated humanely and that euthanasia methods that minimize pain and distress should be used.1,18 Recent regulatory changes in the European Directive now cover the use of cephalopods, and Switzerland has instituted new requirements regarding the transport and culinary killing of lobsters.22,11,25 Although no current regulations in the United States govern the use of invertebrates, increased regulatory oversight in the future is a possibility. The extent to which invertebrates sense pain and distress is unclear, yet many species of invertebrates do have nociceptors and show behavioral changes when exposed to potentially painful or adverse conditions.15,30 The CNS of Artemia consists of a dorsal brain with a double–ventral row of ganglia. The brain connects to the ventral nerve cord through the circumesophageal connective, and many other ganglia and peripheral nerves are present in the body.32 The presence of nociceptors alone does not imply that Artemia feel pain,15 and many factors need to be considered when determining the likelihood that an animal can experience pain or distress;15,30 such evaluation is beyond the scope of this study.
Literature on the behavior of adult Artemia includes references describing their phototaxis.4,6 One group of investigators performed ethological observations of Artemia in field studies and described spatial distribution and swarming behavior.7 No information is available regarding abnormal behavior of Artemia. Toxicity studies generally depend on mortality, hatchability, or various biomarkers for evidence of toxicity.26 Attempts have been made to use phototaxis as a measure of ecotoxicity in Artemia,14 but the complexity of the phototaxic behavior in this species made data interpretation difficult. Another study used video tracking to detect differences in the movement of individual Artemia exposed to inhalant anesthetics, and shrimp highly affected by the anesthetic maintained only approximately 10% of their initial activity level.31 No other references specific to the anesthesia or euthanasia of adult Artemia are available. Although other information regarding the anesthesia and euthanasia of various other crustaceans is available, results vary among species and anesthetic agents, suggesting that more research is needed prior to using any anesthetic in any invertebrate species.12,13
In our current study, Artemia were exposed to the anesthetic until 5 min after confirmation of anesthesia or for a maximum of 60 min, at which point the anesthesia was considered to have failed. Only 63% of Artemia became anesthetized with TMS, suggesting that a 4-g/L solution of this agent is not consistently effective for anesthetizing Artemia. Although our initial data showed that 2.5 mg/L eugenol provided fast and consistent anesthesia of Artemia, we were unable to replicate these results in subsequent trials, during which eugenol failed to induce anesthesia at concentrations as high as 130 mg/L, a dose 2 orders of magnitude higher than the published dose for white Indian shrimp (1.3 mg/L) and well in excess of the AVMA recommendation of 0.125 mL/L (125 mg/L).5,8 Titrations were performed over a 7-mo period to account for possible seasonal variation. We are confident in our calculations, solutions used, chemical quality, and water quality, and no reason for the differing results has been determined. One explanation of the inconsistency may be the overall health of the batch of shrimp used in the first set of experiments. Compared with the later batches of Artemia purchased, these earlier animals were difficult to keep alive; perhaps their health status was poor for the first part of the experiment. In addition, it is possible that the producer that we used has bred for hardier shrimp since our initial purchase. We also do not know the conditions in which these animals are shipped. Furthermore, 5.5% of control animals were recorded as anesthetized, but these animals were likely in poor health, and they died during the experiment. Consequently approximately 5.5% of subjects in each group could have been considered anesthetized but that actually died due to poor health, and determining which ones died due to the anesthetic agent compared with poor health is impossible. The groups differed with overwhelming significance in both time to anesthesia and probability of anesthesia when presented as Kaplan-Meier plots. Overall, the cumulative results indicate that none of the first-step solutions tested here produced reliable anesthesia; we therefore cannot recommend any of them for use in Artemia.
After 5 min of anesthesia, Artemia were transferred to 1 of 3 euthanasia solutions. All subjects that entered the second-step solution were euthanized, suggesting that all 3 agents are suitable for euthanasia in a 2-step process. These results disprove our hypothesis that 70% alcohol would not achieve euthanasia of anesthetized Artemia. Regardless of the anesthetic used, euthanasia groups differed significantly from each other, with 95% alcohol providing the fastest euthanasia times for all 3 anesthetics. When assessing the total time of euthanasia from entry into the anesthetic solution, the combination of 60% alcohol with 95% alcohol provided the fastest euthanasia process, whereas TMS followed by 10% NBF took the longest time.
To assess the potential stress of exposure to the anesthetics, Artemia were observed for the first 5 min of immersion in the first-step solutions. In comparison to the control group, alcohol caused significantly more abnormal behaviors, thereby fitting our hypothesis that 60% alcohol is not appropriate as an anesthetic solution. However, eugenol caused less abnormal behavior than the control group (tank water only), thus suggesting that either eugenol had a calming effect on Artemia or that our behavior scoring system is not effective for assessing these animals. To our knowledge, this study represents the first time that behavior has been used to assess stress in adult Artemia. Although we observed and characterized normal behavior before developing a behavior scoring system for use with Artemia, more research may be necessary to determine what constitutes normal and abnormal behavior for this species. We interpreted these abnormal behaviors to be the result of direct exposure to the chemicals, which acted as aversive stimuli. The abnormal behavior we saw was predominantly abnormal posturing, followed by hyperactivity. Abnormal posturing and hyperactivity were observed in the eugenol group, with abnormal posturing occurring most commonly during the first few seconds of exposure. No seizure-like behavior was observed in this group. The most seizure-like behavior was observed in the control group, which brings into question what this behavior signifies. The behavior of the alcohol group was characterized by hyperactivity and abnormal posturing over prolonged periods of time, followed by many of the shrimp remaining in a curled position. Abnormal behavior for the TMS group was dominated by abnormal posturing. The duration of abnormal behavior did not affect the overall score. Perhaps the initial behavioral reaction in all groups was due to stress from the transfer process.
To assess the ability of Artemia to recover from anesthesia, Artemia were anesthetized for 5 min and then placed in tank water for as long as 2 h. In comparison to alcohol, TMS was significantly more likely to result in recovery, suggesting that TMS may be safe at high doses in Artemia. Recovery times for all groups were highly variable, and some shrimp considered as not recovered displayed thoracopod movement, suggesting that extending the incubation time might have resulted in recovery.
Although recommended by the AVMA, 5% alcohol produced inconsistent anesthesia in Artemia during preliminary dosing titrations, and much higher doses were needed. To comply with AVMA Guidelines, our goal was to keep the alcohol below 70%, and 60% alcohol anesthetized Artemia in a reasonable timeframe. Throughout the study, 60% alcohol produced abnormal behavior during anesthetic induction; even when defined abnormal behaviors were absent, the animals had uneven swimming patterns and frequently curled while anesthetized. Although 2.5 mg/L eugenol produced consistent anesthesia during the initial study, it was inconsistent in repeat trials, when doses as high as 130 mg/L were ineffective. TMS led to high variability in responses, with a low rate of anesthesia, but for those Artemia that became anesthetized, TMS provided a smooth induction and wide safety margins for recovery. Overall, TMS took an extended amount of time (average, 35.5 min) to produce anesthesia, and we therefore do not recommend TMS for use as part of a 2-step euthanasia process.
A limitation of this study is the inability to confirm euthanasia of Artemia. The euthanasia parameter we used was lack of thoracopod movement for 10 s of observation, as in a previous study.28 According to this standard during the recovery portion of the study, several Artemia that had been confirmed dead in the anesthetic solution actually regained thoracopod movement during the recovery period, and some even regained forward movement. The AVMA Guidelines recommend a 2-step euthanasia process because it may be difficult to confirm death in invertebrates.8 We did not perform a recovery experiment after the euthanasia step, and the animals remained at least overnight in the euthanasia solution before they were discarded.
Another limitation of our study was our inability to fully assess the animals’ health status. We attempted to choose only actively swimming, vigorous Artemia; when a shrimp stopped swimming on initial placement in the anesthetic, we replaced it. Even with this method, 5.5% of the controls were recorded as anesthetized and euthanized by the solutions, when they in fact died due to reasons unrelated to the experiment. We also had difficulty in keeping the Artemia alive in their housing tank; we therefore purchased a new batch of Artemia for each day of the project. In this regard, we were able to maintain a supply of vigorous Artemia for study use. Tank parameters, temperature, and salinity were all closely evaluated prior to beginning the study; nevertheless, we were unable to find a solution to this problem, even after consulting with other investigators using adult Artemia. When we repeated part of the study 6 mo later, we were easily able to keep the Artemia alive for 1 wk; however, our anesthesia results differed also, rendering eugenol as an ineffective anesthetic.
The potential for future studies is abundant. More research regarding anesthetic solutions is needed to determine an appropriate 2-step euthanasia method for Artemia. It will be interesting to know whether intrinsic factors—including cuticle thickness, sex, and age—play a role in the variability of anesthesia. Extrinsic factors such as water temperature may contribute to the rate of anesthetic induction. More research on scoring and characterizing abnormal behaviors is needed. Lastly, determining the ED50 and LD50 of the anesthetic solutions could be useful in determining safe levels of anesthesia compared with euthanasia.
In conclusion, our results show that eugenol at doses of 2.5mg/L and even as high as 130 mg/L as well as 4 g/L TMS inconsistently achieved anesthesia in Artemia. Although 60% alcohol produced anesthesia, the time to anesthesia varied among repeated trials, and significantly more abnormal behaviors were noted in animals exposed to this concentration. We conclude that, given the number of abnormal behaviors observed after exposure, none of the 3 anesthetic solutions we tested are appropriate for use in Artemia. In contrast, all 3 second-step solutions resulted in euthanasia.
Acknowledgments
We thank Dr Billy Hudson and Kern C Darbyshire for the use of their resources. We acknowledge the Translational Pathology Shared Resource supported by NCI/NIH Cancer Center Support Grant no. 5P30 CA68485 and the Vanderbilt Mouse Metabolic Phenotyping Center Grant no. 2 U24 DK059637.
This work was supported by the NIH grant reference no. DK18381, authored by Billy G Hudson.
References
- 1.AAALAC International. [Internet]. 2016. Canadian Council on Animal Care (CCAC) guidelines to the care and use of experimental animals, vol.1. [Cited 16 Oct 2016]. Available at: http://www.aaalac.org/accreditation/resources_list.cfm
- 2.Dhont J, Sorgeloos P. 2002. Applications of artemia. Chapter 6, p 270–271. In: Abatzopoulos J, Beardmore JA, Clegg JS, Sorgeloos PP. Artemia: basic and applied biology. Dordrecht (Netherlands): Kluwer Academic Publishers. [Google Scholar]
- 3.Adams DJ, Gage PW, Hamill OP. 1977. Ethanol reduces excitatory postsynaptic current duration at a crustacean neuromuscular junction. Nature 266:739–741. 10.1038/266739a0. [DOI] [PubMed] [Google Scholar]
- 4.Aiken RB, Hailman JP. 1978. Positive phototaxis of the brine shrimp Artemia salina to monochromatic light. Can J Zool 56: 708–711. 10.1139/z78-098. [DOI] [Google Scholar]
- 5.Akbari S, Khoshnod MJ, Rajaian H, Afsharnasab M. 2010. The use of eugenol as an anesthetic in transportation of with Indian shrimp (Fenneropenaeus indicus) post larvae. Turk J Fish Aquat Sci 10:423–429. 10.4194/trjfas.2010.0317. [DOI] [Google Scholar]
- 6.Ali AA, Fortuna L, Frasca M, Rashid MT, Xibilia MG. 2011. Complexity in a population of Artemia. Chaos Solitons Fractals 44:306–316. 10.1016/j.chaos.2011.02.007. [DOI] [Google Scholar]
- 7.Anufriieva EV, Shadrin NV. 2014. The swimming behavior of Artemia (Anostraca): new experimental and observational data. Zoology (Jena) 117:415–421. 10.1016/j.zool.2014.03.006. [DOI] [PubMed] [Google Scholar]
- 8.AVMA Panel on Euthanasia. 2013. AVMA guidelines for the euthanasia of animals: 2013 ed, p 74. Schaumber (IL): American Veterinary Medical Association. [Google Scholar]
- 9.Brown P, White MR, Chaille J, Russell M, Oseto C. 1996. Evaluation of 3 anesthetic agents for crayfish (Orconectes virilis). J Shellfish Res 15:433–435. [Google Scholar]
- 10.Cooper JE. 2011. Anesthesia, analgesia, and euthanasia of invertebrates. ILAR J 52:196–204. 10.1093/ilar.52.2.196. [DOI] [PubMed] [Google Scholar]
- 11.Council of the European Communities. 1986. Council Directive 86/609/EEC on the approximation of laws, regulations, and administrative provisions of the member states regarding the protection of animals used for experimental and other scientific purposes. Off J Eur Commun L358: 1–29. [Google Scholar]
- 12.Cowing D, Powell A, Johnson M. 2015. Evaluation of different concentration doses of eugenol on the behaviour of Nephrops norvegicus. Aquaculture 442:78–85. 10.1016/j.aquaculture.2015.02.039. [DOI] [Google Scholar]
- 13.Coyle SD, Dasgupta S, Tidwell JH, Beavers T, Bright LA, Yasharian DK. 2007. Comparative efficacy of anesthetics for the freshwater prawn Macrobrachiurn rosenbergii. J World Aquac Soc 36:282–290. 10.1111/j.1749-7345.2005.tb00332.x. [DOI] [Google Scholar]
- 14.Dojmi Di Delupis G, Rotondo V. 1988. Phototaxis in aquatic invertebrates: possible use in ecotoxicity test. Ecotoxicol Environ Saf 16:189–193. 10.1016/0147-6513(88)90049-8. [DOI] [PubMed] [Google Scholar]
- 15.Elwood RW. 2011. Pain and suffering in invertebrates? ILAR J 52:175–184. 10.1093/ilar.52.2.175. [DOI] [PubMed] [Google Scholar]
- 16.Gilbertson CR, Wyatt JD. 2016. Evaluation of euthanasia techniques for an invertebrate species, land snails (Succinea putris). J Am Assoc Lab Anim Sci 55:577–581. [PMC free article] [PubMed] [Google Scholar]
- 17.Gunkel C, Lewbart GA. 2008. Anesthesia and analgesia of invertebrates, p 535–542. In: Fish RE, Brown MJ, Danneman PJ, Karas AZ. Anesthesia and analgesia in laboratory animals, 2nd ed Cambridge (MA): Academic Press. [Google Scholar]
- 18.Institute for Laboratory Animal Research. 2011. Guide for the care and use of laboratory animals, 8th ed Washington (DC): National Academies Press. [Google Scholar]
- 19.Judge SE. 1980. General anaesthetic action in the invertebrate central nervous system. Gen Pharmacol 11:337–341. 10.1016/0306-3623(80)90095-6. [DOI] [PubMed] [Google Scholar]
- 20.Kenny NJ, Sin YW, Shen X, Zhe Q, Wang W, Chan TF, Tobe SS, Shimeld SM, Chu KH, Hui JH. 2014. Genomic sequence and experimental tractability of a new decapod shrimp model, Neocaridina denticulata. Mar Drugs 12:1419–1437. 10.3390/md12031419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kerschbaum HH, Hermann A. 1997. Ethanol suppresses neuronal Ca2+ currents by effects on intracellular signal transduction. Brain Res 765:30–36. 10.1016/S0006-8993(97)00386-7. [DOI] [PubMed] [Google Scholar]
- 22.Le Conseil Federal Le Portail du Gouvernement Suisse. [Internet]. 2008Ordinance on the protection of animals. Amendment 1-10-2018. Articles 23, 178, and 178a. [Cited 25 February 2018]. https://www.blv.admin.ch/blv/fr/home/tiere/tierschutz/revision-verordnungen-veterinaerbereich.html. [In French].
- 23.Lew HC, Din M, Shariff M. 2010. Reliability of total haemocyte count as stress indicator in giant tiger shrimp (Penaeus monodon). In: The 5th proceedings of the Seminar in Veterinary Sciences, Serdang, Selangor. 5–8 January 2010. Universiti Putra Malaysia Institutional Repository; 54–58. [Google Scholar]
- 24.Murray MJ. 2011. Euthanasia. p 441–444. In: Lewbart GA. Invertebrate medicine, 2nd ed Hoboken (NJ): John Wiley and Sons; 10.1002/9780470960806 [DOI] [Google Scholar]
- 25.National Health and Medical Research Council. [Internet] 2013. Australian code of practice for the care and use of animals for scientific purposes, 8th ed. [Cited 01 Jan 2017]. Available at: http://www.nhmrc.gov.au.
- 26.Nunes BS, Carvalho FD, Guilhermino LM, Van Stappen G. 2006. Use of the genus Artemia in ecotoxicity testing. Environ Pollut 144:453–462. 10.1016/j.envpol.2005.12.037. [DOI] [PubMed] [Google Scholar]
- 27.Ramlochansingh C, Branoner F, Chagnaud BP, Straka H. 2014. Efficacy of tricaine methanesulfonate (MS222) as an anesthetic agent for blocking sensory–motor responses in Xenopus laevis tadpoles. PLoS One 9:1–11. 10.1371/journal.pone.0101606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sanchez MI, Petit C, Martinez-Haro M, Taggart MA, Green AJ. 2016. May arsenic pollution contribute to limiting Artemia franciscana invasion in southern Spain? PeerJ 4:e1703.1 –22. doi:10.7717/peerj.1703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schmit O, Mezquita F. 2010. Experimental test on the use of MS222 for ostracod anaesthesia: concentration, immersion period, and recovery time. J Limnol 69:350–352. 10.4081/jlimnol.2010.350. [DOI] [Google Scholar]
- 30.Sneddon LU. 2015. Pain in aquatic animals. J Exp Biol 218:967–976. 10.1242/jeb.088823. [DOI] [PubMed] [Google Scholar]
- 31.Takasaki M, Tatara T, Suezaki Y, Shirahama K, Kamaya H, Ueda I, Totoki T.1991. Effect of inhalation anesthetics on swimming activity of Artemia salina. J Anesth 5:287–293. 10.1007/s0054010050287. [DOI] [PubMed] [Google Scholar]
- 32.Zhang Q, Keller R, Dircksen H. 1997. Crustacean hyperglycaemic hormone in the nervous system of the primitive crustacean species Daphnia magna and Artemia salina (Crustacea: Branchiopoda). Cell Tissue Res 287:565–576. 10.1007/s004410050779. [DOI] [PubMed] [Google Scholar]