Abstract
Promoting healthy lifestyle factors (e.g., physical activity, healthy eating, less screen time) among young people is a relevant and challenging step toward reducing non-communicable diseases. This study aimed to evaluate the effect of a multicomponent intervention on lifestyle factors among adolescents from schools in low Human Development Index (HDI < 0.500) areas. The Fortaleça sua Saúde program was conducted with 548 adolescents aged 11–18 years old in the intervention group and 537 in the control group. The four-month intervention included strategies focused on training teachers, new opportunities for physical activity in the school environment, and health education strategies for the school community (including parents). Moderate- to-vigorous physical activity level (≥420 min/week), TV watching and computer use/gaming (<2 h/day), daily consumption of fruit juice, fruit, vegetables, soft drinks, savory foods and sweets, and current alcohol and tobacco use were measured before and after intervention. McNemar’s test and logistic regression (odds ratio [OR] and a 95% confidence interval [95% CI]) were used, considering p < 0.05. In the intervention schools, a significant increase occurred in the number of adolescents who met physical activity guidelines (5.3%; 95% CI = 0.8; 9.8) and who reported using computer for <2 h a day (8.6%; 95% CI = 3.8; 13.4) after intervention. No changes were observed in the control schools. At the end of the intervention, adolescents from intervention schools were more likely to practice physical activity at recommended levels (OR = 1.44; 95% CI = 1.00; 2.08) than adolescents from control schools. No significant change was observed for the other lifestyle factors. In conclusion, this multicomponent intervention was effective in promoting physical activity among adolescents from vulnerable areas. However, other lifestyle factors showed no significant change after intervention. This study is registered at Clinicaltrials.gov NCT02439827.
Keywords: childhood behaviors, chronic disease, social vulnerability
1. Introduction
Modifiable unhealthy behaviors, such as tobacco use, excessive alcohol consumption, unhealthy eating, physical inactivity [1] and sedentary behavior [2] are important lifestyle factors which impact the occurrence of non-communicable diseases (NCDs) [3]. An increase in NCDs such as hypertension and type 2 diabetes has been observed worldwide; in particular, these diseases are becoming more prevalent in economically vulnerable areas [4]. For this reason, promoting healthy lifestyles is urgent.
Agendas focused on reducing NCDs emphasize that adolescents’ lifestyles should be a target of the intervention programs [5,6]. Most of the habits are established in this period of life which in turns might influence them later in life [7,8]. The World Health Organization has highlighted actions in schools as one of the most cost effectiveness ways to prevent NCDs in children and adolescents [6], these initiatives are also encouraged by several researchers [9,10,11,12].
However, few studies of school-based lifestyle interventions are multicomponent (i.e., focusing on different lifestyle outcomes) at this point [13,14]. A systematic review found that most interventions target either addiction (drug use, alcohol use, and smoking) or energy balance (nutrition, physical activity, and screen time) [13], but few, if any, have combined these outcomes. Thus studies analyzing synergistic effects from interventions are scarce [13], even though the issue is a priority for public health.
Another central concern is that social and environmental aspects play an important role as determinants of health and lifestyle behaviors [15]. A review of reviews focusing on behavioral interventions concluded that there is an urgent call for studies in a lower socioeconomic context (usually defined as areas with a Human Development Index [HDI] lower than 0.500), as individuals from vulnerable contexts might face more barriers to managing their behaviors and health [16], which contributes directly to health inequities [17,18]. Thus, monitoring efforts and advancement offers is an opportunity to understand the challenges faced by areas that need more attention [19].
Based on these concerns, the present study aimed to evaluate the effect of a multicomponent intervention on lifestyle indicators (physical activity, TV watching and computer use/gaming, healthy and unhealthy eating habits, and tobacco and alcohol use) among adolescents from schools situated in low-HDI (<0.500) municipalities in the northeast region of Brazil.
2. Materials and Methods
2.1. Study Design and Sample
The present study is a cluster-randomized controlled trial in which schools were the sample selection units. The authorization of the participants’ parents or guardians, through the signing of free and informed consent forms, was a criterion for participation in the research. The National Ethics System (protocol nº 17366313.9.0000.0121) approved this research project. Further methodological details of the study, including a description of the sample size estimate and the flowchart of the sample selection, can be found elsewhere [20,21].
This study was carried out in 2014 in Fortaleza, Northeastern Brazil. All six full-time schools with adolescents enrolled in grades 7–9 and allied to the School Health Program (Programa Saúde na Escola, PSE) were considered eligible for the study. The Programa Saúde na Escola (Federal Decree No. 6286) aims to provide comprehensive prevention, health promotion and care for children and adolescents who attend schools in the public education system. The schools were randomly allocated to each group, with three in the intervention group and three in the control group.
A total of 1272 adolescents (639 in intervention schools and 633 in control schools) were enrolled in grades 7–9 of eligible schools in the beginning of the study. Of these, 1182 adolescents completed the baseline measures (92.0% and 93.8% of the adolescents in the intervention and control schools, respectively) and 1085 completed follow-up measures (with a response rate of 93.2% and 90.4% in the intervention and control schools, respectively) [21].
2.2. Description of the Intervention
The full description of the intervention can be observed in previous publications [20,21]. The intervention was based on socioecological theory [22] and socio-cognitive theory [23], as well as allied with the concept of Health Promoting Schools [24]. The control group schools maintained their regular routine of activities. Strategies regarding the intervention were focused on three components: teacher training, health education, and environmental changes.
The teacher training was given to all teachers from intervention schools at the beginning of the study, and it was focused on two aspects. The first part focused on lifestyle, addressing physical activity and its implications for health, excessive screen time, eating, and prevention of alcohol and tobacco consumption; the second part focused on the relationship of these behaviors to school environment and academic performance. Supportive material was delivered to teachers to assist them in creating both lessons related to the promotion of a healthy lifestyle and strategies proposed by the intervention protocol.
Specific training for physical education teachers was conducted over the same period and duration as that received by teachers from other disciplines. The main impetus was to make physical education classes more active, reaching moderate or vigorous physical activity intensity. Supporting materials were also made available for teachers. In addition to the supporting material, undergraduate physical education adolescents were present throughout the semester to assist the teacher during the classes.
Changes in the school environment were also made to encourage physical activity and decrease sedentary behavior outside classes. Supervised sessions of 10 to 15 min, called “Gymnastics at School”, were performed twice a week. In addition, Games were organized in school places and equipment was made available so that adolescents could play games/sports during free time at school. Strategies involving the school environment also included banners with explanations of the games/sports and health messages involving lifestyle factors.
Strategies focused on health education were enhanced through teacher training, as proposed activities in the classroom and physical education classes involved producing educational material (e.g., posters, newsletters, and health pamphlets) which was then exhibited throughout the school. In addition, pamphlets focusing on physical activity and health, screen time and health, and healthy eating and healthy behaviors were distributed to adolescents, while parents received pamphlets about parental/family involvement in physical activity and screen time. The pamphlets were delivered to a member of the school administration (coordinator or principal) early in the intervention, advising that pamphlets should be distributed at the beginning of school day, during classes, and at parent/teacher meetings at the school.
Considering these strategies, different healthy lifestyle factors were focused on the Fortaleça sua Saúde program, as described in Table 1. The primary goals of the Fortaleça sua Saúde program were to promote physical activity and reduce screen time; thus, all strategies had content related to these lifestyle factors. Strategies to promote healthy eating comprised teacher training, health lessons in the classroom, and health education messages in the school context. Moreover, substance (alcohol and tobacco) use was also addressed in teacher training, health lessons in the classroom, and the health education pamphlets distributed to adolescents.
Table 1.
Description of the Components and Lifestyle Factors Focused of the Fortaleça sua Saúde Program Strategies.
| Component Descriptions and Strategies | PA | Screen Time | Healthy Eating | Alcohol and Tobacco Use Prevention |
|---|---|---|---|---|
| Training and activities in general curriculum and PE classes | ||||
|
✓ | ✓ | ✓ | ✓ |
|
✓ | ✓ | ✓ | ✓ |
|
✓ | ✓ | ✓ | ✓ |
|
✓ | ✓ | ✓ | ✓ |
| Active opportunities in the school environment | ||||
|
✓ | ✓ | ||
|
✓ | ✓ | ||
|
✓ | ✓ | ✓ | |
|
✓ | ✓ | ✓ | |
| Health education in school community | ||||
|
✓ | ✓ | ✓ | ✓ |
|
✓ | ✓ | ||
PA: physical activity; PE: Physical Education. ✓ = Lifestyle behaviors that were focused on the intervention strategies of the Fortaleça sua Saúde program.
2.3. Lifestyle Factors and Data Collection
The lifestyle factors examined include physical activity level, screen time (TV watching and computer use/gaming), healthy and unhealthy eating habits, and tobacco and alcohol use. A physical activity list, validated for Brazilian adolescents [21], was used to estimate the weekly time spent in moderate to vigorous physical activity [25]. This 19-item list included team sports (e.g., soccer, basketball, volleyball), individual physical activity/sports (e.g., swimming, athletics), ride-in physical activity (e.g., skateboarding, rollerblading) and popular games (e.g., dodgeball, “forty-forty”). Adolescents reported the frequency and duration of each physical activity that they performed in a typical week. We identified whether adolescents met the World Health Organization’s physical activity guidelines (60 min per day = 420 min per week) [26]. These items showed acceptable reliability (kappa > 0.60) [20].
Screen time during leisure hours was assessed using questions based on the Youth Risk Behavior Survey Questionnaire, which was previously validated for the Brazilian population: daily time watching TV on habitual weekdays (intra-class correlation coefficient/ICC = 0.72) and daily time using computer/video games on habitual weekdays (ICC = 0.80). The cut-off point of less than two hours per day was adopted for each screen time outcome [27].
Eating habits were observed through a questionnaire with three questions related to healthy food indicators (fruits, fruit juice, and vegetables) and three to unhealthy food indicators (soft drinks, sweets, and savory foods) (ICC range = 0.71–0.89) in a typical week [28,29]. We defined healthy consumption as those who consumed each of the healthy food on a daily basis, or who did not consume each of the unhealthy food daily. The frequency of tobacco (ICC = 0.99) and alcohol (ICC = 0.71) consumed in the month preceding the survey was included [30], with healthy consumption defined as those who did not use tobacco or alcohol in the last month.
The control variables were demographic characteristics: gender, age, and socioeconomic status. They were evaluated using a standardized questionnaire, and socioeconomic status was measured using a questionnaire [30] that estimates the purchasing power of families and ranks them according to categories from richest (A1, A2, B1, B2 = A + B) to poorest (C1, C2, D, E = C + D + E) based on the accumulation of material goods, housing conditions, number of working individuals in the household and the education level of the head of household.
The data collection took place in the second semester of 2014, before and after the implementation of the Fortaleça sua Saúde program. The questionnaire was administered by evaluators who gave prior instructions and read each question aloud to adolescents in the classroom, who then answered the questionnaire individually. Evaluators were aware which schools were in the intervention and control groups, but they were trained in order to assure standardize measurements regardless of group assignment. Data were computed by scanning using the SPHYNX® software (Sphynx Software Solutions Inc., Washington, DC, USA), with corrections for errors and/or inconsistencies.
2.4. Data Analyses
Descriptive statistics were used based on relative frequencies. Proportions of adolescents according to sex, age group, socioeconomic status, and lifestyle factors at baseline were compared between intervention and control groups using the chi-square test. The comparison of the change (follow-up vs. baseline) in proportions of lifestyle factors was performed in each group using McNemar’s test.
Logistic regression was used to identify the odds ratio for the intervention group, when compared with the control group, adopting the healthy categories of the different lifestyle behaviors after follow-up. In the adjusted analysis, models were adjusted for gender, age, socioeconomic status, occupation and outcome variable at baseline, and clustering by school. The level of significance for all analysis was 5% for two-tailed tests using the statistical software SPSS® 23.0 (SPSS IBM Inc., Chicago, IL, USA).
3. Results
The sample consisted of 1085 participants. Of these, 51.5% were male and 52.9% were aged 11–13 years-old. A large proportion of adolescents (74.3%) came from lower socioeconomic status households. Three out of ten adolescents (29.7%) met the physical activity guidelines at baseline. The percentage of adolescents who reported watching TV or using a computer for less than two hours a day were 29.1% and 45.5%, respectively. Daily consumption of fruit juices, fruits, and/or vegetables was reported by 20.1%, 18.9%, and 12.4%, respectively. Not consuming soft drinks, savory foods and sweets on a daily basis were reported by 73.6%, 77.9%, and 68.9% adolescents, respectively. A total of 77.4% and 93.9% reported not drinking alcohol and using tobacco in the month previous to the baseline. There was no statistically significant difference between intervention and control adolescents at baseline for lifestyle factors, except for savory foods (p = 0.005) and sweets (p = 0.017; see Table 2).
Table 2.
Adolescents’ Characteristics at Baseline of the Fortaleça sua Saúde Program, 2014.
| Variables at Baseline | All (n = 1085) |
Intervention (n = 548) |
Control (n = 537) |
p-Value b |
|---|---|---|---|---|
| Gender | % (n) | |||
| Boys | 51.5 (559) | 51.8 (284) | 51.2 (275) | 0.903 |
| Girls | 48.5 (526) | 48.2 (264) | 48.8 (262) | |
| Age groups (years) | ||||
| 11–13 | 52.9 (574) | 54.2 (297) | 51.6 (277) | 0.160 |
| 14–18 | 47.1 (574) | 45.8 (251) | 48.4 (260) | |
| Socioeconomic status | ||||
| A + B (higher status) | 25.7 (277) | 27.5 (150) | 23.8 (127) | 0.256 |
| C + D + E (lower status) | 74.3 (802) | 72.5 (395) | 76.2 (407) | |
| Lifestyle factors | ||||
| % adolescents who met PA guideline (420 min/wk MVPA) a | 29.7 (322) | 28.2 (166) | 31.9 (190) | 0.159 |
| % adolescents who reported watching TV < 2 h/day | 29.1 (316) | 28.7 (169) | 31.1 (185) | 0.367 |
| % adolescents who reported using computer <2 h/day | 45.5 (491) | 43.7 (257) | 46.6 (277) | 0.312 |
| % adolescents who consumed fruit juice daily | 20.1 (218) | 18.7 (110) | 22.1 (131) | 0.153 |
| % adolescents who consumed fruit daily | 18.9 (205) | 19.4 (114) | 18.2 (108) | 0.596 |
| % adolescents who consumed vegetables daily | 12.4 (134) | 12.4 (73) | 12.6 (75) | 0.913 |
| % adolescents who did not intake soft drinks daily | 73.6 (799) | 72.3 (425) | 73.1 (434) | 0.762 |
| % adolescents who did not intake savory foods daily | 77.9 (845) | 80.3 (472) | 73.4 (436) | 0.005 |
| % adolescents who did not intake sweets daily | 68.9 (747) | 71.8 (422) | 65.3 (388) | 0.017 |
| % adolescents who did not intake alcohol in the last month | 77.4 (840) | 78.7 (463) | 75.3 (447) | 0.154 |
| % adolescents who did not use tobacco in the last month | 93.9 (1019) | 93.2 (548) | 93.6 (556) | 0.779 |
Abbreviations: Min/wk, minutes per week; PA, physical activity; MVPA, moderate to vigorous physical activity. a Missing in PA = 2. b p-value were estimated using the Chi-square test, and bold data indicated significant values (p < 0.05).
In the intervention group, the proportion of adolescents who met physical activity guidelines, who reported watching TV less than two hours a day, and who reported using the computer less than two hours per day increased significantly after follow-up: 5.3% (p = 0.016), 6.4% (p = 0.004), and 8.6% (p < 0.001), respectively. The proportion of adolescents who did not eat sweets daily increased by 8.2% (p < 0.001) after intervention. In the control group, significant changes occurred for the proportion of adolescents who reported watching TV for less than two hours per day (increase of 4.7%; p = 0.038) and who did not intake sweets daily (increase of 7.4%; p = 0.001). No significant changes were observed for other lifestyle factors (consumption of fruit juice, fruits, vegetables, soft drinks, savory foods, or current alcohol and tobacco use) for adolescents from the intervention and control groups (p > 0.05). Analyzing the adolescents who adopted healthy lifestyle factors after follow-up (changes at individual level) similar changes occurred for intervention and control adolescents; there was an overlap of the 95% CI for all variables (see Table 3).
Table 3.
Effect of the Fortaleça sua Saúde Program on Lifestyle Factors among Brazilian Adolescents from Low-HDI Areas, 2014.
| Lifestyle Factors | Prevalence Difference between Follow-Up vs. Baseline (95% CI) a | Prevalence of Adolescents Who Adopt the Outcome after Follow-Up (Individual Level) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention (n = 548) |
Control (n = 537) |
Intervention (n = 548) |
Control (n = 537) |
|||||||||||
| % | (95% CI) | p a | % | (95% CI) | p a | % | (95% CI) | % | (95% CI) | |||||
| % adolescents who met PA guideline (420 min/wk MVPA) | 5.3 | 0.8 | 9.8 | 0.016 | −3.2 | −7.6 | 1.2 | 0.141 | 15.9 | 13.0 | 19.2 | 10.8 | 8.4 | 13.7 |
| % adolescents who reported watching TV < 2 h/day | 6.4 | 1.9 | 10.8 | 0.004 | 4.7 | 0.1 | 9.2 | 0.038 | 16.4 | 13.5 | 19.8 | 15.8 | 13.0 | 19.2 |
| % adolescents who reported using computer < 2 h/day | 8.6 | 3.8 | 13.4 | <0.001 | 3.7 | −0.9 | 8.3 | 0.098 | 19.9 | 16.7 | 23.5 | 15.5 | 12.6 | 18.8 |
| % adolescents who consumed fruit juice daily | 2.0 | −2.2 | 6.2 | 0.333 | −2.4 | −6.6 | 1.8 | 0.241 | 12.8 | 10.2 | 15.8 | 10.2 | 7.9 | 13.1 |
| % adolescents who consumed fruit daily | 0.2 | −3.8 | 4.2 | 0.926 | −0.6 | −4.7 | 3.6 | 0.783 | 10.6 | 8.3 | 13.5 | 10.8 | 8.4 | 13.7 |
| % adolescents who consumed vegetables daily | 0.9 | −2.5 | 4.3 | 0.579 | 1.1 | −2.4 | 4.6 | 0.513 | 7.8 | 5.9 | 10.4 | 8.4 | 6.3 | 11.1 |
| % adolescents who did not intake soft drinks daily | 2.9 | −1.2 | 7.1 | 0.151 | 2.2 | −1.9 | 6.3 | 0.265 | 12.8 | 10.2 | 15.8 | 11.9 | 9.4 | 15.0 |
| % adolescents who did not intake savory foods daily | −1.5 | −5.6 | 2.6 | 0.465 | 3.2 | −1.2 | 7.5 | 0.138 | 10.2 | 7.9 | 13.1 | 13.8 | 11.1 | 17.0 |
| % adolescents who did not intake sweets daily | 8.2 | 3.8 | 12.6 | <0.001 | 7.4 | 3.0 | 11.9 | 0.001 | 17.3 | 14.4 | 20.7 | 16.6 | 13.7 | 20.0 |
| % adolescents who did not intake alcohol in the last month | −0.7 | −4.7 | 3.2 | 0.706 | 0.4 | −3.4 | 4.1 | 0.837 | 9.9 | 7.6 | 12.7 | 8.9 | 6.8 | 11.7 |
| % adolescents who did not use tobacco in the last month | 0.4 | −2.2 | 2.9 | 0.763 | −0.4 | −2.6 | 1.9 | 0.724 | 4.2 | 2.8 | 6.2 | 2.8 | 1.7 | 4.6 |
Note: Min/wk: minutes per week; OR: odds ratio; PA: physical activity; MVPA: moderate-to-vigorous physical activity; 95% CI: 95% confidence interval. a p-values obtained using the McNemar’s test for comparisons of proportions, and bold data indicated significant values (p < 0.05).
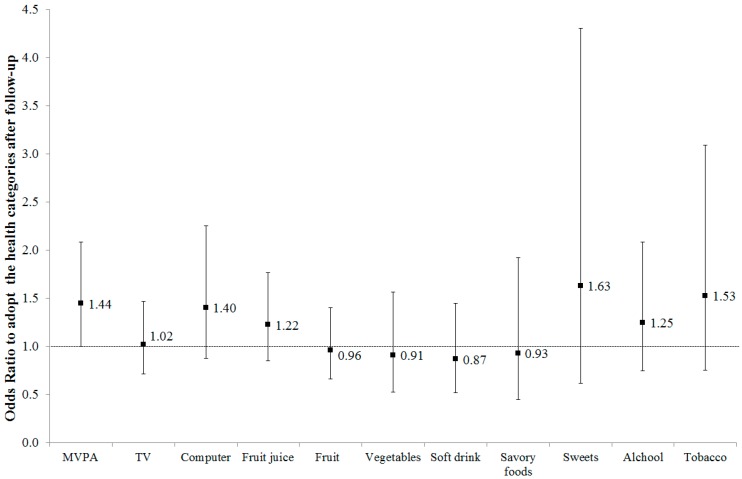
After adjusting for confounders, adolescents from the intervention group were more likely (OR = 1.44; 95% CI: 1.00; 2.08; p = 0.50) to adopt the physical activity guidelines after follow-up, in comparison to adolescents in the control group. No significant changes were observed for the other lifestyle factors (p > 0.05, see Figure 1).
Figure 1.
Logistic Regression (Odds Ratio and 95% Confidence Interval) of Intervention Group Adolescents (vs. Control Group Adolescents) Adopting Healthy Lifestyle Factors after Follow-up of the Fortaleça sua Saúde Program, 2014. Note: MVPA: moderate-to-vigorous physical activity. Logistic regression adjusted by gender, age, socioeconomic status and lifestyle factor at baseline and clustering by school.
4. Discussion
Our results indicated that the Fortaleça sua Saúde program had a positive (small) effect on physical activity, but not on other health-related behaviors such as healthy eating and substance use, among adolescents in low-HDI areas in Brazil. This highlights the relevance, but also the difficulty, of finding a comprehensively effective form (i.e., leading to significant changes in different behaviors) of healthy lifestyle intervention in a school setting, particularly in vulnerable areas [15,16].
Positive changes in adolescents among the intervention group were found mainly for outcomes related to an active lifestyle: physical activity level, TV watching and computer use/gaming. The positive changes may be concentrated on physical activity and screen time because most strategies were focused on these lifestyle factors (as shown in Table 1). Indeed, information on the implementation of the program has shown that strategies such as the availability of sports equipment, active lessons in the school curriculum (e.g., English lessons incorporating physical activity) and educational materials (e.g., health risk of high screen time) have contributed to improve attitudes and behaviors toward an active lifestyle [21].
Similar results were observed in other multicomponent interventions involving physical activity among Brazilian adolescents [31,32]. A systematic review of lifestyle interventions focused on obesity prevention among adolescents from low- and middle-income countries also highlighted that multicomponent interventions tend to be more effective in promoting physical activity, and reducing the prevalence of obesity [33] compared to intervention focused on a single component (e.g., a strategy aimed at changing just the school environment).
Effective intervention for reducing screen time was observed with Chinese adolescents. One seven-month school-based peer education program led to a reduction of sedentary behavior by up to 20 min on weekdays [34]. Another study with adolescents from low-income neighborhoods in New York City showed a significant reduction of days per week and hours per day in the use of videogames and watching TV, when compared to the control group [35]. Considering that elevated screen time and low levels of physical activity are frequent in most Brazilian adolescents [36], and that they are associated with NCD risk factors such as high blood glucose and obesity [4,37], our results have shown relevant evidence that multicomponent school-based interventions can be a reasonable strategy for promoting active lifestyles among adolescents who live in a context with higher social vulnerabilities.
Despite being multicomponent, our study did not observe changes in eating consumption, tobacco use, or alcohol consumption. It is important to mention that those variables were not considered primary targets of the intervention, which may lead to a lack of strategy to implement eating or substance use changes. Indeed, strategies on eating consumption and substance use were exclusively focused on knowledge (i.e., without changes on environment and policies such as food availability), which may be insufficient to promote health behavior change [12]. Also, an implementation analysis of the Fortaleça sua Saúde program highlighted distinctions between schools in the intervention management (e.g., teachers from all three intervention schools performed health lessons, but almost half of the activities were performed in only one school, while teachers from other schools reported issues such as the absence of education facilities and the lack of planning time). This may reduce the changes on lifestyle outcomes in some contexts and, thus, the total effect of the program [21].
Similar results were observed in the multicomponent CLICK-Obesity Study with Chinese adolescents; from the four eating patterns investigated, it was observed change only in a reduced frequency of red meat consumption (OR = 1.50; 95% CI: 1.15; 1.95). However, the CLICK-Obesity study was feasible and effective in improving changes in awareness of selected risk factors for obesity, such as the importance of consuming fewer calorie-dense foods [38]. Our intervention also included a set of strategies focused on healthy eating education (as shown in Table 1) and may also increase the knowledge of obesogenic eating patterns; however, a behavioral change was not found.
Other evidence from less developed countries shows different results, and changes in eating habits were observed in adolescents from Bangkok, Thailand [39] and Beirut, Lebanon [40]. In both studies, eating was a primary outcome; thus, specified strategies focused on school food policy and school community were implemented.
For tobacco and alcohol use among adolescents no changes were found in the present study. However, a systematic review of lifestyle interventions (focused on tobacco use, alcohol, illicit drug use, risky sexual behavior, and aggressive behavior) showed that, when substance use is a primary target with strategies aimed specifically at decreasing its frequency, multicomponent interventions in school settings tend to be effective in decreasing these behaviors [41]. Our work, therefore, demonstrates the urgency of proposing primary strategies that integrate multicomponent programs aligned with the reduction of tobacco and alcohol use among adolescents from vulnerable areas, since the literature consistently observes a negative association between tobacco and alcohol use and NCDs [42,43,44].
Several limitations of the present study can be addressed. First, the extent to which the intervention actions put against the outcomes were not investigated and can be addressed as a constraint. Also, it is unknown if the synergy among positive outcomes was sufficient to promote changes in eating, tobacco, and alcohol use. It is important to mention that all schools (intervention and control) attempted the national diet program, and it is unknown whether strategies other than ours were applied in order to encourage a healthy eating. The health-related behaviors investigated were self-reported, and the biases that accompany self-reported measures can impact the estimates of the effects (e.g., precision, memory, etc.), especially where food habits are concerned. The duration of the intervention for approximately four months, as well as the lack of maintenance assessments, should be a matter for concern. Other methodological limitations have been further explored in a previous publication [21].
5. Conclusions
This multicomponent intervention, which included teacher training, environmental changes, and health education, had a positive effect on physical activity among adolescents from schools in vulnerable areas; relevant changes on screen time among adolescents from intervention schools were also observed. However, no differences were observed in eating consumption or tobacco and alcohol use. Our results showed that the school is a locus for active lifestyle promotion, however designing and implementing interventions that are focused on multiple lifestyle indicators remains a challenge. It is urgent that a global action for healthy lifestyle be implemented in vulnerable contexts, in order to help young people to prevent NCDs and promote health and well-being.
Acknowledgments
We thank the Municipal Education Department for technical support and authorization to the study execution. We thank all members of the school community (managers, teachers, parents and adolescents) who were involved in this study. We thank the Fortaleça sua Saúde Working Group, which is detailed in a previous publication (http://www.biomedcentral.com/1471-2458/15/1212).
Author Contributions
V.C.B.F., A.d.S.B., K.S.d.S. and S.A.M.d.S. participated in all stages of the study, including design, planning, implementation and supervision of the program. V.C.B.F. and A.d.S.B. analyzed the data. All authors participated in the interpretation of data, contributed to the first version of the manuscript, and critically reviewed the document. The final version of the manuscript was approved by all authors.
Funding
This study has no funding for its implementation. Some authors received individual grants from the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior—Brasil Finance Coode 001 (VCBF, N. 10737/2014-6; ASB, N. 88882.181607/2018-01; RMC, N. 88882.181618/2018-01) and Fundação de Amparo à Pesquisa e Inovação do Estado de Santa Catarina (SM, GM, JAS, and SAMS). The funding agencies had no participation in the interpretation, analysis, writing and approval of this manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.World Health Organization . Noncommunicable Diseases Progress Monitor 2017. World Health Organization; Geneva, Switzerland: 2017. [Google Scholar]
- 2.Ding D., Rogers K., van der Ploeg H., Stamatakis E., Bauman A.E. Traditional and Emerging Lifestyle Risk Behaviors and All-Cause Mortality in Middle-Aged and Older Adults: Evidence from a Large Population-Based Australian Cohort. PLoS Med. 2015;12:e1001917. doi: 10.1371/journal.pmed.1001917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization . World Health Statistics 2017: Monitoring Health for the Sustainable Development Goals SDGs. World Health Organization; Geneva, Switzerland: 2017. [Google Scholar]
- 4.Organisation mondiale de la santé . Global Status Report on Noncommunicable Diseases 2014: Attaining the Nine Global Noncommunicable Diseases Targets; a Shared Responsibility. World Health Organization; Geneva, Switzerland: 2014. [Google Scholar]
- 5.Sawyer S.M., Afifi R.A., Bearinger L.H., Blakemore S.-J., Dick B., Ezeh A.C., Patton G.C. Adolescence: A foundation for future health. Lancet. 2012;379:1630–1640. doi: 10.1016/S0140-6736(12)60072-5. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization . Preventing Chronic Diseases Designing and Implementing Effective Policy. World Health Organization; Geneva, Switzerland: 2014. [Google Scholar]
- 7.Gore F.M., Bloem P.J., Patton G.C., Ferguson J., Joseph V., Coffey C., Sawyer S.M., Mathers C.D. Global burden of disease in young people aged 10–24 years: A systematic analysis. Lancet. 2011;377:2093–2102. doi: 10.1016/S0140-6736(11)60512-6. [DOI] [PubMed] [Google Scholar]
- 8.Kann L., Mcmanus T., Harris W.A., Shanklin S., Flint K.H., Hawkins J., Queen B., Lowry R., Olsen E.O., Chyen D., et al. Youth Risk Behavior Surveillance—United States, 2015. MMWR Surveill. Summ. 2016;65:1–174. doi: 10.15585/mmwr.ss6506a1. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization . Interventions on Diet and Physical Activity: What Works: Summary Report. World Health Organization; Geneva, Switzerland: 2009. [PubMed] [Google Scholar]
- 10.Dobbins M., Husson H., DeCorby K., LaRocca R.L. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Database Syst. Rev. 2013 doi: 10.1002/14651858.CD007651.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hayman L.L. Preventive Cardiovascular Health in Schools: Current Status. Curr. Cardiovasc. Risk Rep. 2017;11:24. doi: 10.1007/s12170-017-0549-2. [DOI] [Google Scholar]
- 12.Langford R., Bonell C., Komro K., Murphy S., Magnus D., Waters E., Gibbs L., Campbell R. The Health Promoting Schools Framework: Known Unknowns and an Agenda for Future Research. Health Educ. Behav. 2017;44:463–475. doi: 10.1177/1090198116673800. [DOI] [PubMed] [Google Scholar]
- 13.Busch V., de Leeuw J.R.J., de Harder A., Schrijvers A.J.P. Changing Multiple Adolescent Health Behaviors Through School-Based Interventions: A Review of the Literature. J. School Health. 2013;83:514–523. doi: 10.1111/josh.12060. [DOI] [PubMed] [Google Scholar]
- 14.Champion K.E., Newton N.C., Spring B., Wafford Q.E., Parmenter B.J., Teesson M. A systematic review of school-based eHealth interventions targeting alcohol use, smoking, physical inactivity, diet, sedentary behaviour and sleep among adolescents: A review protocol. Syst. Rev. 2017;6:246. doi: 10.1186/s13643-017-0645-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Havranek E.P., Mujahid M.S., Barr D.A., Blair I.V., Cohen M.S., Cruz-Flores S., Davey-Smith G., Dennison-Himmelfarb C.R., Lauer M.S., Lockwood D.W., et al. Social Determinants of Risk and Outcomes for Cardiovascular Disease: A Scientific Statement from the American Heart Association. Circulation. 2015;132:873–898. doi: 10.1161/CIR.0000000000000228. [DOI] [PubMed] [Google Scholar]
- 16.Jepson R.G., Harris F.M., Platt S., Tannahill C. The effectiveness of interventions to change six health behaviours: A review of reviews. BMC Public Health. 2010;10:538. doi: 10.1186/1471-2458-10-538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Craike M., Wiesner G., Hilland T.A., Bengoechea E.G. Interventions to improve physical activity among socioeconomically disadvantaged groups: An umbrella review. Int. J. Behav. Nutr. Phys. Act. 2018;15:43. doi: 10.1186/s12966-018-0676-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Love R.E., Adams J., van Sluijs E.M.F. Equity effects of children’s physical activity interventions: A systematic scoping review. Int. J. Behav. Nutr. Phys. Act. 2017;14:134. doi: 10.1186/s12966-017-0586-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Niessen L.W., Mohan D., Akuoku J.K., Mirelman A.J., Ahmed S., Koehlmoos T.P., Trujillo A., Khan J., Peters D.H. Tackling socioeconomic inequalities and non-communicable diseases in low-income and middle-income countries under the Sustainable Development agenda. Lancet. 2018;391:2036–2046. doi: 10.1016/S0140-6736(18)30482-3. [DOI] [PubMed] [Google Scholar]
- 20.Barbosa Filho V.C., da Silva Lopes A., Lima A.B., de Souza E.A., do Amaral Gubert F., Silva K.S., Vieira N.F.C., Trompieri Filho N., de Araújo T.S., de Bruin P.F.C., et al. Rationale and methods of a cluster-randomized controlled trial to promote active and healthy lifestyles among Brazilian adolescents: The “Fortaleça sua Saúde” program. BMC Public Health. 2015;15:1212. doi: 10.1186/s12889-015-2543-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barbosa Filho V.C., da Silva K.S., Mota J., Beck C., da Silva Lopes A. A physical activity intervention for Brazilian adolescents from low human development index areas: A cluster-randomized controlled trial. J. Phys. Act. Health. 2016;13:1174–1182. doi: 10.1123/jpah.2016-0113. [DOI] [PubMed] [Google Scholar]
- 22.Bronfenbrenner U. Ecological models of human development. Int. Encycl. Educ. 1994;3:37–43. [Google Scholar]
- 23.Bandura A. Health promotion by social cognitive means. Health Educ. Behav. 2004;31:143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 24.Guedes D.P., Lopes C.C. Validação da versão brasileira do Youth Risk Behavior Survey 2007. Revista de Saúde Pública. 2010;44:840–850. doi: 10.1590/S0034-89102010000500009. [DOI] [PubMed] [Google Scholar]
- 25.de Farias Júnior J.C., Lopes A.D.S., Mota J., Santos M.P., Ribeiro J.C., Hallal P.C. Validade e reprodutibilidade de um questionário para medida de atividade física em adolescentes: Uma adaptação do Self-Administered Physical Activity Checklist. Rev. Bras. Epidemiol. 2012;15:198–210. doi: 10.1590/S1415-790X2012000100018. [DOI] [PubMed] [Google Scholar]
- 26.World Health Organization . Global Recommendations on Physical Activity for Health. World Health Organization; Geneva, Switzerland: 2010. [PubMed] [Google Scholar]
- 27.Tremblay M.S., LeBlanc A.G., Janssen I., Kho M.E., Hicks A., Murumets K., Colley R.C., Duggan M. Canadian Sedentary Behaviour Guidelines for Children and Youth. Appl. Physiol. Nutr. Metab. 2011;36:59–64. doi: 10.1139/H11-012. [DOI] [PubMed] [Google Scholar]
- 28.Nahas M.V., de Barros M.V.G., de Assis M.A.A., Hallal P.C., Florindo A.A., Konrad L. Methods and Participant Characteristics of a Randomized Intervention to Promote Physical Activity and Healthy Eating among Brazilian High School Adolescents: The Saude na Boa Project. J. Phys. Act. Health. 2009;6:153–162. doi: 10.1123/jpah.6.2.153. [DOI] [PubMed] [Google Scholar]
- 29.Silva K.S.D., Lopes A.D.S., Hoefelmann L.P., Cabral L.G.D.A., De Bem M.F.L., Barros M.V.G.D., Nahas M.V. Projeto COMPAC (comportamentos dos adolescentes catarinenses): Aspectos. Revista Brasileira de Cineantropometria e Desempenho Humano. 2013;15 doi: 10.5007/1980-0037.2013v15n1p1. [DOI] [Google Scholar]
- 30.Associação Brasileira de Empresas de Pesquisa—Critério de Classificação Econômica Brasil. 2012. Pesquisa Google. [(accessed on 24 October 2018)]; Available online: http://www.abep.org/criterio-brasil.
- 31.De Barros M.V.G., Nahas M.V., Hallal P.C., de Farias Júnior J.C., Florindo A.A., de Barros S.S.H. Effectiveness of a school-based intervention on physical activity for high school adolescents in Brazil: The Saude na Boa project. J. Phys. Act. Health. 2009;6:163–169. doi: 10.1123/jpah.6.2.163. [DOI] [PubMed] [Google Scholar]
- 32.Ribeiro R.Q., Alves L. Comparison of two school-based programmes for health behaviour change: The Belo Horizonte Heart Study randomized trial. Public Health Nutr. 2014;17:1195–1204. doi: 10.1017/S1368980013000189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Verstraeten R., Roberfroid D., Lachat C., Leroy J.L., Holdsworth M., Maes L., Kolsteren P.W. Effectiveness of preventive school-based obesity interventions in low- and middle-income countries: A systematic review. Am. J. Clin. Nutr. 2012;96:415–438. doi: 10.3945/ajcn.112.035378. [DOI] [PubMed] [Google Scholar]
- 34.Cui Z., Shah S., Yan L., Pan Y., Gao A., Shi X., Wu Y., Dibley M.J. Effect of a school-based peer education intervention on physical activity and sedentary behaviour in Chinese adolescents: A pilot study. BMJ Open. 2012;2:e000721. doi: 10.1136/bmjopen-2011-000721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Contento I.R., Koch P.A., Lee H., Calabrese-Barton A. Adolescents Demonstrate Improvement in Obesity Risk Behaviors after Completion of Choice, Control & Change, a Curriculum Addressing Personal Agency and Autonomous Motivation. J. Am. Diet. Assoc. 2010;110:1830–1839. doi: 10.1016/j.jada.2010.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Costa C.D.S., Flores T.R., Wendt A., Neves R.G., Assunção M.C.F., Santos I.S. Comportamento sedentário e consumo de alimentos ultraprocessados entre adolescentes brasileiros: Pesquisa Nacional de Saúde do Escolar (PeNSE), 2015. Cadernos de Saúde Pública. 2018;34 doi: 10.1590/0102-311x00021017. [DOI] [PubMed] [Google Scholar]
- 37.De Rezende L.F.M., Rodrigues Lopes M., Rey-López J.P., Matsudo V.K.R., Luiz O.D.C. Sedentary Behavior and Health Outcomes: An Overview of Systematic Reviews. PLoS ONE. 2014;9:e105620. doi: 10.1371/journal.pone.0105620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Xu F., Ware R.S., Leslie E., Tse L.A., Wang Z., Li J., Wang Y. Effectiveness of a Randomized Controlled Lifestyle Intervention to Prevent Obesity among Chinese Primary School Adolescents: CLICK-Obesity Study. PLoS ONE. 2015;10:e0141421. doi: 10.1371/journal.pone.0141421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chawla N., Panza A., Sirikulchayanonta C., Kumar R., Taneepanichskul S. Effectiveness of a school-based multicomponent intervention on children nutritional status among primary school children in bangkok, thailand. J. Ayub Med. Coll. Abbottabad. 2017;29:13–20. [PubMed] [Google Scholar]
- 40.Habib-Mourad C., Ghandour L.A., Moore H.J., Nabhani-Zeidan M., Adetayo K., Hwalla N., Summerbell C. Promoting healthy eating and physical activity among school children: Findings from Health-E-PALS, the first pilot intervention from Lebanon. BMC Public Health. 2014;14:940. doi: 10.1186/1471-2458-14-940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hale D.R., Fitzgerald-Yau N., Viner R.M. A Systematic Review of Effective Interventions for Reducing Multiple Health Risk Behaviors in Adolescence. Am. J. Public Health. 2014;104:e19–e41. doi: 10.2105/AJPH.2014.301874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tomita A., Manuel J.I. Evidence on the association between cigarette smoking and incident depression from the South African National Income Dynamics Study 2008–2014: Mental health implications for a resource-limited setting. Nicotine Tobacco Res. 2018 doi: 10.1093/ntr/nty163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Murphy C.M., Janssen T., Colby S.M., Jackson K.M. Low Self-Esteem for Physical Appearance Mediates the Effect of Body Mass Index on Smoking Initiation Among Adolescents. J. Pediatr. Psychol. 2018 doi: 10.1093/jpepsy/jsy070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Granville-Garcia A.F., Clementino M.A., Gomes M.D.N.C., Firmino R.T., Ribeiro G.L.A., Siqueira M.B.L.D. Alcohol consumption among adolescents. Ciência Saúde Coletiva. 2014;19:7–16. doi: 10.1590/1413-81232014191.1989. [DOI] [PubMed] [Google Scholar]