Abstract
We previously identified a nuclear variant of bone morphogenetic protein 2 (BMP2), named nBMP2, that is translated from an alternative start codon. Decreased nuclear localization of nBMP2 in the nBmp2NLStm mouse model leads to muscular, neurological, and immune phenotypes—all of which are consistent with aberrant intracellular calcium (Ca2+) response. Ca2+ response in these mice, however, has yet to be measured directly. Because a prior study suggested impairment of macrophage function in nBmp2NLStm mutant mice, bone marrow derived (BMD) macrophages and splenic macrophages were isolated from wild type and nBmp2NLStm mutant mice. Immunocytochemistry revealed that nuclei of both BMD and splenic macrophages from wild type mice contain nBMP2, while the protein is decreased in nuclei of nBmp2NLStm mutant macrophages. Live-cell Ca2+ imaging and engulfment assays revealed that Ca2+ response and phagocytosis in response to bacterial supernatant are similar in BMD macrophages isolated from naïve (uninfected) nBmp2NLStm mutant mice and wild type mice, but are deficient in splenic macrophages isolated from mutant mice after secondary systemic infection with Staphylococcus aureus, suggesting progressive impairment as macrophages respond to infection. This direct evidence of impaired Ca2+ handling in nBMP2 mutant macrophages supports the hypothesis that nBMP2 plays a role in Ca2+ response.
Introduction
Our group has reported the existence of a nuclear variant of the growth factor bone morphogenetic protein 2 (BMP2), designated nBMP21. This variant protein is produced by translation from an alternative downstream start codon that eliminates the N-terminal endoplasmic reticulum signal peptide, thus preventing the protein’s delivery to the secretory pathway. Instead, nBMP2 is translated in the cytoplasm and translocated to the nucleus by means of an embedded bipartite nuclear localization signal (NLS)1. Using immunohistochemistry, we have detected nBMP2 in skeletal muscle nuclei and in the nuclei of CA1 neurons in the hippocampus2,3.
To examine the function of nBMP2, we generated a mutant mouse strain (nBmp2NLStm) in which a three-amino acid substitution in the NLS inhibits translocation of nBMP2 to the nucleus while still allowing normal synthesis and secretion of the conventional BMP2 growth factor2. The mice appear overtly normal and are fertile. They do, however, lack nBMP2 in myonuclei, and electrophysiological studies revealed that skeletal muscle relaxation is significantly slowed after stimulated twitch contraction, a process that is regulated by intracellular Ca2+ transport. Consistent with impaired intracellular Ca2+ transport, sarco/endoplasmic reticulum Ca2+ ATPase (SERCA) activity is decreased in skeletal muscle2. The mutant mice also lack nBMP2 in CA1 hippocampal neurons, and electrophysiological studies revealed reduced long-term potentiation (LTP) in the hippocampus3. LTP is dependent on intracellular Ca2+ transport and is thought to be the cellular equivalent of learning and memory4–6. Behavioral tests revealed that the nBMP2 mutant mice have impaired object recognition memory3.
Intracellular Ca2+ elevation also regulates the activation and differentiation of several different types of immune cells including T cells, B cells, dendritic cells, and macrophages7–10. To see if nBmp2NLStm mutants had compromised immune response, mice were challenged by systemic infection with Staphylococcus aureus. While the mutants’ immune response to a primary infection appeared normal, their immune response to a secondary infection challenge 30 days later resulted in higher levels of bacteremia, increased mortality, and failure of spleens to enlarge normally11. Although we did not observed differences in the total number of macrophages in spleen, thymus, or lymph node from wild type compared to mutant mice, we did observe that after the secondary infection, spleen from nBmp2NLStm mutant mice showed fewer hemosiderin-laden macrophages than spleen from wild type mice11. Macrophages in the spleen accumulate hemosiderin by phagocytosing damaged red blood cells and hemoglobin, which would be present in the blood stream of S. aureus-challenged mice due to the hemolysins that S. aureus expresses12–14. The observation of fewer hemosiderin-laden macrophages in the spleens of mutant mice after a secondary infection suggested to us that macrophage phagocytic activity might be impaired in the absence of nBMP2, potentially providing us with an accessible cell type in which to directly test our hypothesis that intracellular Ca2+ response is disrupted in the absence of nBMP2.
To interrogate if nBMP2 might play a role in Ca2+ response, we isolated macrophages from wild type and nBmp2NLStm mutant mice. These macrophages included bone marrow derived (BMD) macrophages from uninfected mice, and splenic macrophages from mice that had undergone primary and secondary infections with S. aureus15. Live-cell Ca2+ imaging as well as bead engulfment assays were performed to measure intracellular Ca2+ response and phagocytic activity. These analyses revealed deficient Ca2+ response and phagocytosis in splenic macrophages isolated from mutant mice after secondary systemic infection with S. aureus, but not in BMD macrophages from naïve mice, suggesting that as nBmp2NLStm mutant cells respond to infection over time, Ca2+ response is progressively impaired.
Results
The nuclear variant nBMP2 is expressed in BMD and splenic macrophages from wild type mice
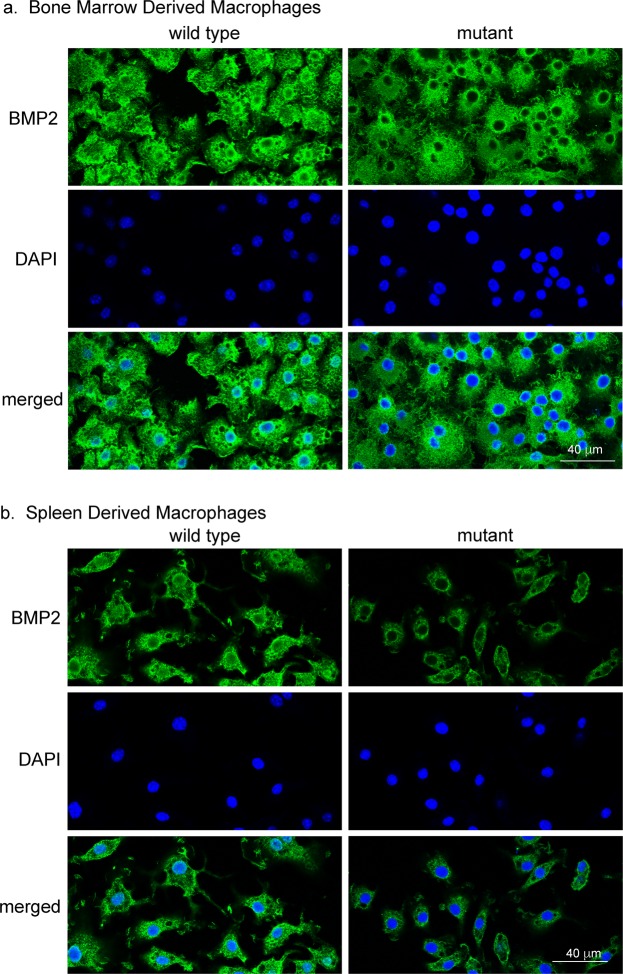
To determine whether nBMP2 is expressed in macrophages, BMD macrophages and splenic macrophages were isolated from naïve (uninfected) wild type and nBmp2NLStm mutant mice and differentiated in vitro, and immunocytochemistry was performed using an anti-BMP2 antibody that binds to both BMP2 and nBMP2. Consistent with our prior observation of impaired immune response in nBmp2NLStm mutant mice11, nBMP2 was detected in the nuclei of wild type BMD (Fig. 1a) and splenic (Fig. 1b) macrophages. As expected, nBMP2 was significantly decreased in macrophage nuclei from nBmp2NLStm mutant mice (Fig. 1a,b, mutant). ImageJ software quantification of immunofluorescence images showed that the density of nuclear BMP2 staining was significantly more intense in wild type compared to mutant macrophages in both BMD macrophages (p = 0.0005) and splenic macrophages (p < 0.0001) (Fig. 2). BMP2 staining was visible throughout the cytoplasm of both wild type and mutant macrophages, as expected, given that nBMP2 is synthesized in the cytosol before being translocated to the nucleus and that the conventional BMP2 growth factor is synthesized in the rough ER and translocated through the Golgi before being secreted from the cell.
Figure 1.
BMD macrophages and splenic macrophages express nBMP2, which is decreased in the nuclei of nBmp2NLStm mutant macrophages. (a) BMD macrophages and (b) splenic macrophages were stained with anti-BMP2 antibody (green) and counterstained with DAPI (blue), demonstrating that nBMP2 is expressed and localized to the nucleus in wild type macrophages, and that nuclear translocation of nBMP2 is inhibited in mutant macrophages. BMP2 labeling within the cytoplasm is present in both wild type and mutant cells as expected, because the targeted mutation allows translation of nBMP2 in the cytoplasm but inhibits nuclear translocation, and it allows normal synthesis and secretion of conventional BMP2.
Figure 2.

Quantification of nBMP2 nuclear staining intensity. Five images each were analyzed for wild type and mutant BMD macrophages and for mutant splenic macrophages. Four images were analyzed for wild type splenic macrophages. Each image contained between 10 and 93 cells, and the number of cells analyzed per group ranged from 100 to 337. ImageJ was used to outline DAPI-stained regions and quantify BMP2 immunostaining as the sum of pixel intensities within each nucleus. The mean density of BMP2 immunostaining was then calculated for all nuclei in an image. An unpaired, two-tailed t-test was performed to compare nuclear staining between wild type and mutant cells. For BMD wild type vs. mutant macrophages, p = 0.0005. For splenic wild type vs mutant macrophages, p < 0.0001.
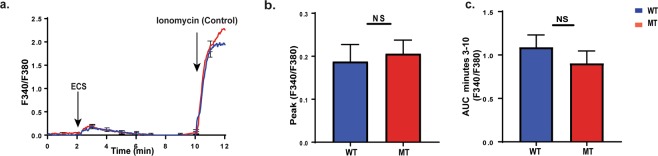
BMD macrophages from uninfected nBmp2NLStm mutant mice and wild type mice have similar Ca2+ response
Naïve BMD macrophages isolated from femurs and tibias of uninfected mice were differentiated and activated in vitro then plated for live-cell Ca2+ imaging. Plated cells were loaded with Fura-2AM, a UV-excitable ratiometric calcium indicator that changes its excitation in response to Ca2+ binding; Fura-2AM emits at 380 nm when Ca2+ is not bound, and at 340 nm when Ca2+ binds to the dye. The fluorescence ratio (F340/F380), increases as cytosolic Ca2+ levels increase16. At the 2 min time point, supernatant from Escherichia coli (ECS) cultures was added to stimulate Ca2+ flux (Fig. 3a)17–19. Following this stimulation, there were no observable differences between naïve mutant and wild type BMD macrophages in peak Ca2+ response (Fig. 3b) or sustained Ca2+ levels (Fig. 3c).
Figure 3.
Naïve bone marrow derived (BMD) macrophages from nBmp2NLStm mutant mice and wild type mice have a similar Ca2+ response. Naïve BMD macrophages from wild type (WT) and nBmp2NLStm mutant (MT) mice were loaded with Fura-2AM for live-cell Ca2+ imaging. During imaging, cells were stimulated at 2 min with E. coli supernatant (ECS), then at 10 min with ionomycin as a positive control. (a) Average curves showing intracellular Ca2+ response in wild type and nBmp2NLStm mutant BMD macrophages. Fluorescence ratios (F340/F380) were measured at 3 sec intervals from 0–12 min (n = 38 cells). Error bars (s.e.m.) are shown at one min intervals. (b) Average (±s.e.m.) of peak Ca2+ influx (F340/F380) in wild type and nBmp2NLStm mutant BMD macrophages (n = 38 cells). (c) Area under the curve (AUC) of F340/F380 ratios from minutes 3 to 10 min shows sustained intracellular Ca2+ levels (n = 38 cells). NS, not significant.
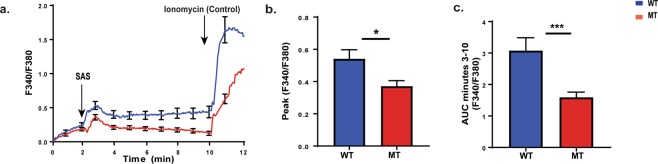
Splenic macrophages isolated from nBmp2NLStm mutant mice after secondary infection show impaired Ca2+ response
In our prior study, immune deficiencies in nBMP2NLStm mice were detectable only after the mice received a secondary infection with S. aureus11. Because our current experiments revealed no significant differences in Ca2+ response in naïve BMD macrophages from mutant compared to wild type mice, we decided to replicate the in vivo conditions of our previous work by examining splenic macrophage harvested from mice after a secondary infection with S. aureus, and by using S. aureus supernatant as the stimulus to trigger Ca2+ flux11. Although S. aureus is a gram positive bacteria that does not produce LPS, it does produce liphoteichoic acid (LTA), which is similarly able to activate macrophages20,21. Thirty-five days after primary systemic S. aureus infections, mice were given a second injection of S. aureus, and splenic macrophages were isolated 3 days later.
After one week in vitro maturation, splenic macrophages were loaded with Fura-2AM for live-cell Ca2+ imaging experiments. S. aureus supernatant (SAS) was used to stimulate Ca2+ flux at the 2-min time point (Fig. 4a). Compared to the lack of a difference in naïve BMD macrophages, it is particularly striking that peak Ca2+ response was significantly decreased (p = 0.0335) in mutant splenic macrophages after secondary infection (Fig. 4b). Sustained Ca2+ levels as measured by the area under the curve (AUC) from minutes 3–10 was also significantly decreased (p = 0.0008) (Fig. 4c).
Figure 4.
Splenic macrophages collected from nBmp2NLStm mutant mice after secondary infection have an impaired Ca2+ response. Splenic macrophages from wild type (WT) and nBmp2NLStm mutant (MT) mice were loaded with Fura-2AM for live-cell Ca2+ imaging. During imaging, cells were stimulated at 2 min with S. aureus supernatant (SAS), then at 10 min with ionomycin as a positive control. (a) Average curves showing intracellular Ca2+ response in wild type and nBmp2NLStm mutant splenic macrophages. Fluorescence ratios (F340/F380) were measured at 3 sec intervals from 0-12 min (n = 44 cells). Error bars (s.e.m.) are shown at one min intervals. (b) Average ± s.e.m. of peak Ca2+ influx (F340/F380) in wild type and nBmp2NLStm mutant splenic macrophages shows a significant difference (n = 44 cells). (c) AUC of F340/F380 ratios from minutes 3 to 10 min shows a significant difference in sustained intracellular Ca2+ levels (n = 44 cells). *p < 0.05, **p < 0.01, ***p < 0.0001.
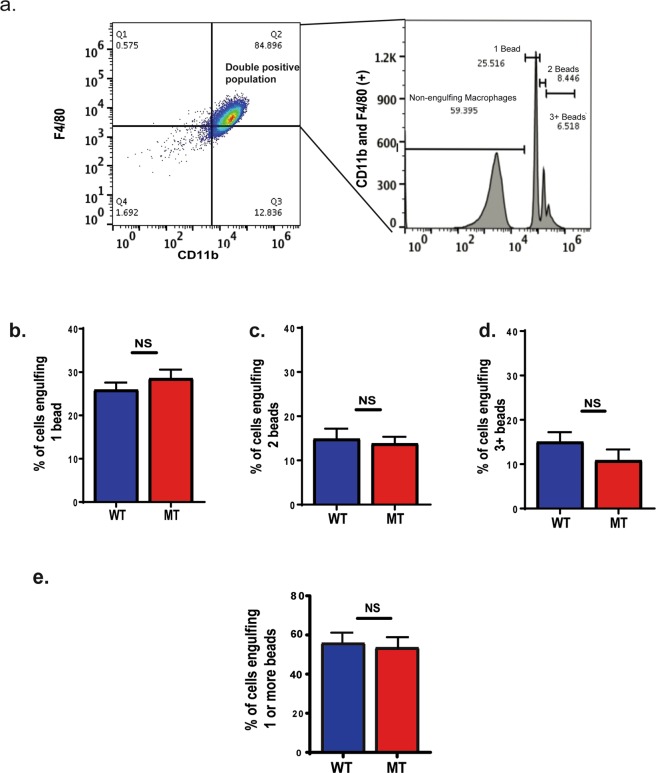
BMD macrophages from uninfected nBmp2NLStm mutant mice and wild type mice show similar phagocytic activity
To test phagocytic activity of naïve BMD macrophages (meaning macrophages that were isolated from uninfected mice) from nBmp2NLStm mutant compared to wild type mice, we measured fluorescent bead engulfment by CD11b and F4/80 positive cells with flow cytometry (Fig. 5a)22–28. We observed no differences in the phagocytic activity of naïve BMD macrophages from nBmp2NLStm mutant compared to wild type mice (Fig. 5b–e).
Figure 5.
Naïve bone marrow derived (BMD) macrophages from nBmp2NLStm mutant mice and wild type mice show similar phagocytic activity. After incubation with fluorescent microspheres, macrophages were analyzed by flow cytometry. (a) A representative analysis is shown. The F4/80 and CD11b double positive population was selected, and from this gate a histogram was produced to identify macrophages that had engulfed 1, 2, or 3 or more beads. The percentages of total double positive cells represented within each peak are indicated. (b) Percent of cells engulfing 1 bead, (c) percent of cells engulfing 2 beads, and (d) percent of cells engulfing 3 or more beads. (e) Percent of cells engulfing one or more beads. N = 3 pairs of wild type and 3 pairs of mutant mice. NS, not significant.
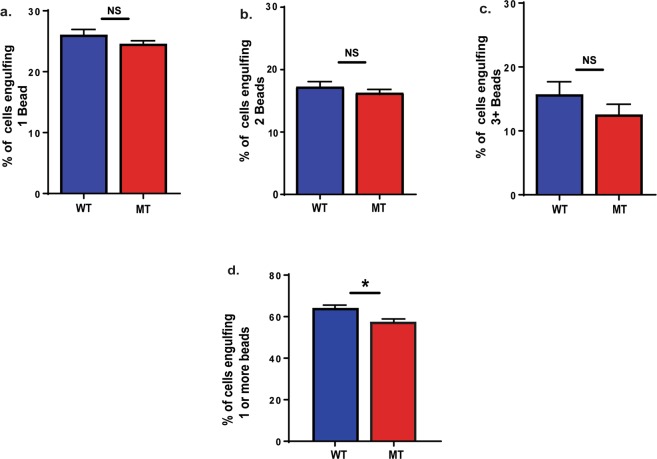
Splenic macrophages from nBmp2NLStm mutant mice show impaired phagocytic activity
To test phagocytic activity in macrophages isolated from mice after secondary infection, splenic macrophages were isolated from wild type and nBmp2NLStm mutant mice 3 days after mice received a second systemic infection with S. aureus, and fluorescent bead engulfment was measured as described above. While differences between wild type and mutant macrophages did not reach significance when subgroups that engulfed 1, 2, or 3 or more beads were analyzed individually (Fig. 6a–c), there was a significant reduction in overall mutant phagocytic activity (p = 0.0176) when the subgroups were pooled (Fig. 6d). These data suggest a possible relationship between the decreased Ca2+ response and reduced phagocytosis in nBmp2NLStm mutant splenic macrophages.
Figure 6.
Splenic macrophages collected from nBmp2NLStm mutant mice after secondary infection show impaired engulfment activity. After incubation with fluorescent microspheres, macrophages were analyzed by flow cytometry as described in Fig. 3. (a) Percent of cells engulfing 1 bead, (b) percent of cells engulfing 2 beads and, (c) percent of cells engulfing 3 or more beads. (d) Percent of cells engulfing one or more beads. N = 3 pairs of wild type and 3 pairs of mutant mice. NS, not significant. *p < 0.05.
Discussion
The role of BMP2 in macrophages is unknown and remains an area of active research. BMP2 has been reported to be constitutively expressed in M1 (inflammatory) macrophages29. Other studies have shown that BMP2 expression is upregulated as macrophages shift toward the pro-healing/anti-inflammatory M2 phenotype30,31. BMP2 secretion by macrophages promotes migration of vascular smooth muscle cells, and macrophages in the intestinal muscularis secrete BMP2 to signal enteric neurons32,33. Reports of BMP2 expression by hematopoietic cells, in particular macrophages, are relevant to this study because nBMP2 can be produced from the same mRNA as the conventional secreted BMP2 growth factor—any time BMP2 mRNA or BMP2 growth factor is detected, the potential for nBMP2 synthesis exists1. Accordingly, we have demonstrated by immunofluorescence that both BMD macrophages and splenic macrophages express the nuclear variant of BMP2, nBMP2, and that nBMP2 is decreased in the nuclei of macrophages from nBmp2NLStm mutant mice.
Previously, we demonstrated that deficiency of nBMP2 in the nucleus impairs secondary immune response as evidenced by diminished spleen enlargement, poor clearance of S. aureus from the bloodstream, and increased mortality after secondary infection11. We have also shown that deficiency of nBMP2 in myonuclei is correlated with slowed skeletal muscle relaxation after contraction, and deficiency of nBMP2 in the nuclei of hippocampal neurons is correlated with learning/memory deficits2,3. Each of these phenotypes is consistent with deficiencies in intracellular Ca2+ transport, but until now, no direct measurements of intracellular Ca2+ have been performed in cells from nBmp2NLStm mutant mice. The discovery that macrophages express nBMP2 (Fig. 1) provided an accessible cell type in which to directly address the question of whether nBMP2 plays a role in intracellular Ca2+ response.
We found that intracellular Ca2+ response was impaired in mutant splenic macrophages after secondary infection with S. aureus, but not in mutant BMD macrophages isolated from uninfected mice, even though both macrophage types expressed nBMP2. Recent work has revealed that innate immune cells can undergo memory-like adaptive responses to increasing pathogen load, and the deficient Ca2+ response in splenic macrophages after secondary infection might represent a failure of those adaptive responses34,35. Alternatively, it may be that the effects of nBMP2 deficiency in the nucleus are simply cumulative, causing a Ca2+-handling phenotype that becomes progressively more severe as cells differentiate and mature. A progressive phenotype is consistent with our previously reported observation that hippocampal long-term potentiation (LTP) was normal in 3-week-old nBmp2NLStm mutant mice but deficient in 3-month-old mice3. Progressive impairment of intracellular Ca2+ response has received attention recently as a potential mechanism for both brain and muscle aging36–38, suggesting that nBMP2 dysfunction could contribute to premature aging or aging-related diseases.
Deficiency of nBMP2 in the nucleus also produced a significant decrease in the total phagocytic activity of splenic macrophages from nBmp2NLStm mutant mice, suggesting that mutant cells may be less effective at clearing pathogens from the blood stream. This is consistent with prior studies suggesting that intracellular Ca2+ mobilization plays a role in macrophage phagocytic activity. For example, impaired Ca2+ response in macrophages from Trpm4(−/−) mutant mice led to decreased phagocytic activity, resulting in bacterial overgrowth and translocation to the bloodstream39. Intracellular Ca2+ levels increase during Fcɣ receptor (FcR)-mediated phagocytosis40–42, and the loss of CaMKK2, a calcium-dependent kinase, left macrophages unable to phagocytose bacteria or synthesize cytokines in response to bacterial lipopolysaccharide (LPS)43.
Although evidence supports the involvement of Ca2+ response in macrophage phagocytic activity, the scale of the decreased phagocytosis by splenic macrophages observed in our study seems insufficient to account for the markedly increased mortality of nBmp2NLStm mutant mice after secondary infection3. We cannot rule out the possibility that the bead engulfment assay did not fully reflect the severity of phagocytosis impairment in splenic macrophages. Liver macrophages also play a role in bacterial clearance, and it is possible that the absence of nBMP2 in the nucleus affects their function more severely44,45. In addition, the absence of nBMP2 in the nucleus might affect other immune system cell types besides macrophages, and it is possible that another cell type, or perhaps several cell types together, account for the increased mortality of nBmp2NLStm mutant mice after secondary infection3. Indeed, BMP2 (and therefore potentially nBMP2) is expressed by a specialized endothelial population in the early embryo, termed hemogenic endothelium, that gives rise to hematopoietic stem cells46. The absence of nBMP2 at the earliest stages of hemogenesis could therefore impact a wide range of immune cell types. BMP2 is also expressed in human cord blood cells, including those that express CD34, a hematopoietic progenitor cell antigen47, and acute bleeding triggers upregulation of BMP2 expression in hematopoietic stem cells48. BMP2 expression is also found in mature B cells, where it is upregulated in response to infection with Aggregatibacter actinomycetemcomitans49. It is possible, therefore, that nBMP2 impacts the activation or function of other immune cell types in addition to macrophages, and the combined functional deficits account for the increased mortality in nBmp2NLStm mutant mice after secondary infection.
It will be important, in future work, to elucidate the molecular mechanisms underlying the Ca2+ response differences between macrophages from wild type and nBMP2 mutant mice. Differences may stem from impaired uptake or release of Ca2+ from endoplasmic reticulum stores, as suggested by the decreased SERCA activity observed in skeletal muscle of nBMP2 mutant mice2. Alternatively, transport of Ca2+ could be impaired at the macrophage cell membrane, consistent with observations that increasing extracellular Ca2+ levels can improve phagocytosis50,51. Neurons and muscle cells are excitable cells and are therefore equipped with a different set of ion channels and transporters than are macrophages, and so it will be important to examine molecular details of the Ca2+ handling defect in all three cell types. This work has thus opened the way for future studies into the molecular interactions and activities of nBMP2.
Questions about how nBMP2 functions from inside the nucleus to affect Ca2+ response also remain to be answered. The novel protein nBMP2 was first identified from among nuclear proteins that had been isolated using DNA affinity chromatography, but subsequent experiments failed to show direct binding of nBMP2 to DNA, and the amino acid sequence of nBMP2 contains no predicted DNA-binding domain1. It is possible that nBMP2 interacts indirectly with DNA through a transcription factor, and future studies of nBMP2’s impact on the expression of genes involved in Ca2+ signaling will be informative.
In summary, this study supports our working hypothesis that aberrant intracellular Ca2+ response is the mechanism that unites the otherwise disparate muscle, neurological, and immune phenotypes observed in nBmp2NLStm mutant mice2,3,11,52–54. In doing so, this study has paved the way for future work to elucidate the precise molecular nature of the Ca2+ signaling disruptions in nBMP2 mutant cells and to understand how nBMP2’s interactions in the nucleus impact Ca2+ signaling.
Materials and Methods
Research Animals
This study was carried out in strict accordance with recommendations in the Guide for the Care and Use of Laboratory Animals55. The protocol was approved by the Institutional Animal Care and Use Committee (IACUC) of Brigham Young University (protocol numbers 15-0107 and 15-0603).
Mice were housed in a temperature-controlled (21–22 °C) room with a 12:12 hr light-dark cycle and fed standard rodent chow and water ad libitum. The nBmp2NLStm mice were constructed on a Bl6/129 background, as described2. The homozygous wild type and mutant mice used in this study were obtained by breeding heterozygotes, and genotyping was performed as previously described3. All experiments were performed with male mice at least 6 months of age.
BMD and Splenic Macrophage Isolation
BMD macrophages were obtained from femurs and tibias of wild type and nBmp2NLStm mutant mice and were differentiated in culture at 37 °C with 5% CO2 for 7 days in macrophage medium (DMEM (HyClone), 10% fetal bovine serum (FBS) (HyClone), 20% supernatant from L929 mouse fibroblast as a source of macrophage colony-stimulating factor (M-CSF), 5% heat inactivated horse serum (Sigma), 1 mM sodium pyruvate (Gibco by Life Technologies), 1.5 mM L-glutamine (Thermofisher), 10 u/ml penicillin, 10 μg/ml streptomycin (Gibco by Life Technologies)) prior to plating for immunocytochemistry, Ca2+ imaging or engulfment assays.
Spleens from wild type and nBmp2NLStm mutant mice were homogenized in phosphate buffered saline (PBS). The homogenate was filtered, pelleted at 450 × g for 5 min, suspended in lysis buffer (155 mM NH2Cl, 10 mM KHCO3, 0.1 mM EDTA) on ice for 3–5 min to lyse erythrocytes, and then washed with 37 °C macrophage media and plated in macrophage medium in 6-well plates. After 3 days of culture at 37 °C in 5% CO2, medium was replaced to remove non-adherent cells56. On day 4, 100 ng/ml lipopolysaccharide (LPS) was added to the culture medium to stimulate differentiation, and cells were incubated for 3–4 more days57. Differentiated cells were then plated for immunocytochemistry, Ca2+ imaging, or engulfment assays.
Immunocytochemistry
Immunocytochemistry was performed using BMD and splenic macrophages. Following macrophage isolation and 7-day differentiation as described above, cells were plated on coverslips that were pre-treated with 0.025% HCl in PBS for 20 min to facilitate cell attachment. Cells were cultured for 1–2 days to reach 70–90% confluence, then fixed at 37 °C in 4% paraformaldehyde for 10 min. Epitopes were exposed through antigen retrieval using 5% sodium citrate and 0.25% Tween-20 in ddH2O, pH 6.0, at 95 °C for 10 min. Cells were permeabilized using 0.1% Triton X-100 then blocked for 1.5 hr at room temperature (RT) using SEA BLOCK blocking buffer (ThermoFisher Scientific, 37527). The samples were then probed with 1:50 anti-BMP2 antibody (Novus Biologicals, NBP1-19751) diluted in 10% SEA BLOCK blocking buffer in 0.1% Tween-20/PBS (PBS-T), overnight at 4 °C. The probed slides were then stained with anti-rabbit Alexa Fluor 488 (ThermoFisher Scientific, A-11034) for 1 hr at RT. Afterwards, nuclei were stained by incubating the slides in 1:5000 DAPI in PBS-T for 15 min., then slides were mounted using ProlongTM Gold Antifade Mountant (Life Technologies, P10144) and cured overnight prior to microscopic imaging. Cells were imaged using a Leica TCS-SP8 confocal microscope with 63X magnification, using the same laser intensities for all samples. Appropriate laser lines were used such as 405 nm for DAPI and 488 nm for BMP2-Alexa Fluor 488.
Comparison of nuclear BMP2 staining intensity between wild type and mutant cells was performed on tiff versions of confocal microscope images using ImageJ to create tracings of DAPI-stained regions and to calculate the mean pixel intensity of nBMP2 staining within each nucleus. Mean nuclear staining intensity was calculated for each image, and groups were compared using an unpaired, two-tailed t-test in GraphPad Prism.
S. aureus Bacterial Infections
S. aureus ATCC strain 12600 was cultured in tryptic soy broth liquid culture alternating with standard streak plating on mannitol salt agar (Thermo Fisher Scientific) for counting. To prepare bacteria for injections, 100 µl of overnight liquid culture was transferred into a new 15 ml broth culture and grown until OD600 reached 1.0, then pelleted and resuspended in 15 ml of PBS with 20% glycerol, aliquoted, and stored at −80 °C for 3 weeks before injection. Frozen stock concentration was verified one day before the infection by thawing a single aliquot and performing standard serial dilution plate counts. On the day of infection, S. aureus was diluted from the frozen stock to the desired concentration in PBS, and mice received a 200 μl retroorbital injection using a 1 ml syringe and 27-gauge needle. The injected volume contained a priming dose of 1 × 104 CFU/g body weight on day 0 (primary infection), and a dose of 3 × 105 CFU/g body weight on day 35 (secondary infection). Macrophages were harvested three days later.
Bacterial Supernatant Preparation
Bacterial supernatant obtained from E. coli K12 and S. aureus 12600 was used to stimulate Ca2+ fluxes in BMD and splenic macrophages19,58. A single colony was picked from an agar plate and inoculated into liquid broth overnight culture. The next day, 1 ml of the overnight culture was inoculated into 15 ml liquid broth and incubated with shaking at 37 °C until culture reach an OD600 of 1–1.3. Cells were then pelleted by centrifugation at 1,800 × g for 12 min at 4 °C, and supernatant was collected.
Calcium Imaging
BMD and splenic macrophages were isolated and differentiated in culture for 7 days as described above, then seeded on 8-chambered coverglasses (Nunc 155411, Thermo Scientific) and incubated overnight in macrophage medium at 37 °C in 5% CO2. For BMD macrophages, 10 ng/ml LPS from E. coli O55:B5 (Sigma) was included in the overnight incubation to activate cells. The next day, cells were loaded with 3 μM Fura-2AM (Invitrogen) in Ringers solution containing Ca2+ to be used as an extracellular source during the Ca2+ imaging assay (150 mM NaCl, 10 mM glucose, 5 mM HEPES, 5 mM KCl, 1 mM MgCl2, 2 mM CaCl2, pH 7.4) for 30 min at 37 °C in 5% CO2, washed with Ringers solution, then incubated for another 30 minutes at 37 °C in Ringers solution. Calcium imaging was performed at room temperature using an Olympus IX51 inverted microscope equipped with a xenon arc lamp. Fura-2AM loaded macrophages were excited using 340 nm and 380 nm excitation filters, and images of 340 nm, 380 nm, and transmitted light were capture using a florescence microscope camera (Q Imaging Exi Blue) with a 20x objective (N.A. 0.75) at 3-sec intervals. At the 2-min time point in each imaging protocol, 20 μl of bacterial supernatant was added to stimulate Ca2+ flux. Ionomycin (1 μM final concentration) was added at the 10-min time point as a positive control. 10–20 representative cells were selected as regions of interest in each frame, and F340:F380 ratios were calculated and analyzed using CellSens software from Olympus. Each individual cell’s fluorescence was normalized to its first recorded value according to the equation (F-Fo)/Fo, where F is the fluorescence at the specific time point, and Fo is the fluorescence value at time 019,59.
Engulfment Assay
BMD and splenic macrophages were isolated and differentiated in culture for 7 days as described above, then seeded in 12-well culture plates for flow cytometry-based engulfment assays22–28. 100% FBS was used to resuspend 2.0 μm phycoerythrin-conjugated polychromatic red latex microspheres (Polysciences, Inc.) to prevent beads from sticking to the cell membranes during engulfment23. The ~109 particles/ml concentration was chosen to ensure that beads were not a limiting factor in phagocytosis rates23. Macrophages were then activated by adding LPS from E. coli O55:B5 (Sigma) to a final concentration of 10 ng/ml and incubated for 1 hour at 37 °C and 5% CO2. Media was removed and cells were rinsed with cold PBS, then collected and analyzed by flow cytometry using an Attune flow cytometer (Applied Biosystems by Life technologies). Cells were pre-treated with anti-CD16/32 antibodies (14-0161-85 eBioscience) to prevent non-specific antibody binding, then surface stained with APC-conjugated anti-CD11b antibodies (17-0112-82 eBioscience) and FITC-conjugated anti-F4/80 antibodies (11-4801-82 eBioscience). Doublets were removed based on forward scatter width (FSC-W)/forward scatter area (FSC-A), and the F4/80 and CD11b double positive population was selected. From within this gate, engulfing macrophages were distinguished from non-engulfing macrophages based on phycoerythrin fluorescence, and macrophages could be further distinguished based on the engulfment of one, two, or three or more beads. Results were analyzed using FlowJo software (Tree Star).
Data Analysis
All assays were performed as at least three independent repeats, each in triplicate. Area under the curve (AUC) was determined using GraphPad Prism. Statistical significance was assessed using unpaired two-tailed Students T test in GraphPad Prism.
Acknowledgements
We thank Eric Wilson, Michael Olson, and Joseph Thiriot for their help and input with the bacterial infection protocol. This work was supported by a National Institute of Allergy and Infectious Diseases grant (R0102063) to KSW, by a National Cancer Institute grant (R15CA202619) to JLA, and by a Fritz B. Burns Foundation grant to JLA.
Author Contributions
L.C.B. and K.S.W. designed the project and obtained funding; L.C.B., K.S.W. and C.T.F. developed experiments and methodology; H.R.B. bred and maintained experimental animals; J.L.A. and J.C.V. directed and performed immunocytochemistry experiments; C.T.F., G.J.H., C.M.R., T.D.C., H.R.B. and D.K.J. performed remaining experiments; L.C.B., K.S.W. and C.T.F. performed data analysis and wrote the manuscript. All authors helped with manuscript revisions.
Data Availability
All data generated or analyzed during this study are included in this published article. Biological reagents will be made available on request.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Felin JE, et al. Nuclear variants of bone morphogenetic proteins. BMC Cell Biol. 2010;11:20. doi: 10.1186/1471-2121-11-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bridgewater LC, et al. A Novel Bone Morphogenetic Protein 2 Mutant Mouse, nBmp2NLS(tm), Displays Impaired Intracellular Ca(2+) Handling in Skeletal Muscle. Biomed Res Int. 2013;2013:125492. doi: 10.1155/2013/125492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cordner RD, et al. The BMP2 nuclear variant, nBMP2, is expressed in mouse hippocampus and impacts memory. Scientific reports. 2017;7:46464. doi: 10.1038/srep46464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bliss TV, Collingridge GL. A synaptic model of memory: long-term potentiation in the hippocampus. Nature. 1993;361:31–39. doi: 10.1038/361031a0. [DOI] [PubMed] [Google Scholar]
- 5.Nanou E, Scheuer T, Catterall WA. Calcium sensor regulation of the CaV2.1 Ca2+ channel contributes to long-term potentiation and spatial learning. Proc Natl Acad Sci USA. 2016;113:13209–13214. doi: 10.1073/pnas.1616206113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Park P, et al. Calcium-Permeable AMPA Receptors Mediate the Induction of the Protein Kinase A-Dependent Component of Long-Term Potentiation in the Hippocampus. J Neurosci. 2016;36:622–631. doi: 10.1523/jneurosci.3625-15.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Feske S. Calcium signalling in lymphocyte activation and disease. Nature reviews. Immunology. 2007;7:690–702. doi: 10.1038/nri2152. [DOI] [PubMed] [Google Scholar]
- 8.Vig M, Kinet JP. Calcium signaling in immune cells. Nature immunology. 2009;10:21–27. doi: 10.1038/ni.f.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lewis RS. Calcium signaling mechanisms in T lymphocytes. Annu Rev Immunol. 2001;19:497–521. doi: 10.1146/annurev.immunol.19.1.497. [DOI] [PubMed] [Google Scholar]
- 10.Verma S, et al. Selenoprotein K knockout mice exhibit deficient calcium flux in immune cells and impaired immune responses. Journal of immunology. 2011;186:2127–2137. doi: 10.4049/jimmunol.1002878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Olsen DS, et al. Targeted Mutation of Nuclear Bone Morphogenetic Protein 2 Impairs Secondary Immune Response in a Mouse Model. BioMed Research International. 2015;2015:13. doi: 10.1155/2015/975789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang Y, et al. Specific Hemosiderin Deposition in Spleen Induced by a Low Dose of Cisplatin: Altered Iron Metabolism and Its Implication as an Acute Hemosiderin Formation Model. Curr Drug Metab. 2010;11:507–515. doi: 10.2174/138920010791636149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seilie, E. S. & Bubeck Wardenburg, J. Staphylococcus aureus pore-forming toxins: The interface of pathogen and host complexity. Semin Cell Dev Biol, 10.1016/j.semcdb.2017.04.003 (2017). [DOI] [PMC free article] [PubMed]
- 14.Vandenesch F, Lina G, Henry T. Staphylococcus aureus hemolysins, bi-component leukocidins, and cytolytic peptides: a redundant arsenal of membrane-damaging virulence factors? Frontiers in cellular and infection microbiology. 2012;2:12. doi: 10.3389/fcimb.2012.00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weischenfeldt J, Porse B. Bone Marrow-Derived Macrophages (BMM): Isolation and Applications. Cold Spring Harbor Protocols. 2008;2008:pdb.prot5080. doi: 10.1101/pdb.prot5080. [DOI] [PubMed] [Google Scholar]
- 16.Barreto-Chang OL, Dolmetsch RE. Calcium imaging of cortical neurons using Fura-2 AM. Journal of visualized experiments: JoVE. 2009 doi: 10.3791/1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Watkins SC, Salter RD. Functional connectivity between immune cells mediated by tunneling nanotubules. Immunity. 2005;23:309–318. doi: 10.1016/j.immuni.2005.08.009. [DOI] [PubMed] [Google Scholar]
- 18.Christensen MG, et al. [Ca2+]i Oscillations and IL-6 Release Induced by alpha-Hemolysin from Escherichia coli Require P2 Receptor Activation in Renal Epithelia. J Biol Chem. 2015;290:14776–14784. doi: 10.1074/jbc.M115.639526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barbet G, et al. The calcium-activated nonselective cation channel TRPM4 is essential for the migration but not the maturation of dendritic cells. Nature immunology. 2008;9:1148–1156. doi: 10.1038/ni.1648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Seo HS, Michalek SM, Nahm MH. Lipoteichoic Acid Is Important in Innate Immune Responses to Gram-Positive Bacteria. Infection and Immunity. 2008;76:206–213. doi: 10.1128/IAI.01140-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fournier B, Philpott DJ. Recognition of Staphylococcus aureus by the Innate Immune System. Clinical Microbiology Reviews. 2005;18:521–540. doi: 10.1128/cmr.18.3.521-540.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sharma L, et al. Assessment of phagocytic activity of cultured macrophages using fluorescence microscopy and flow cytometry. Methods in molecular biology (Clifton, N.J.) 2014;1172:137–145. doi: 10.1007/978-1-4939-0928-5_12. [DOI] [PubMed] [Google Scholar]
- 23.Steck RP, et al. Pharmacologic immunosuppression of mononuclear phagocyte phagocytosis by caffeine. Pharmacol Res Perspect. 2015;3:e00180. doi: 10.1002/prp2.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dunn PA, Tyrer HW. Quantitation of neutrophil phagocytosis, using fluorescent latex beads. Correlation of microscopy and flow cytometry. The Journal of laboratory and clinical medicine. 1981;98:374–381. [PubMed] [Google Scholar]
- 25.Lehmann AK, Sornes S, Halstensen A. Phagocytosis: measurement by flow cytometry. Journal of immunological methods. 2000;243:229–242. doi: 10.1016/S0022-1759(00)00237-4. [DOI] [PubMed] [Google Scholar]
- 26.Kamei A, et al. Exogenous remodeling of lung resident macrophages protects against infectious consequences of bone marrow-suppressive chemotherapy. Proceedings of the National Academy of Sciences of the United States of America. 2016;113:E6153–E6161. doi: 10.1073/pnas.1607787113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Steinkamp JA, Wilson JS, Saunders GC, Stewart CC. Phagocytosis: flow cytometric quantitation with fluorescent microspheres. Science (New York, N.Y.) 1982;215:64–66. doi: 10.1126/science.7053559. [DOI] [PubMed] [Google Scholar]
- 28.Diler E, et al. Influence of external calcium and thapsigargin on the uptake of polystyrene beads by the macrophage-like cell lines U937 and MH-S. BMC pharmacology & toxicology. 2014;15:16. doi: 10.1186/2050-6511-15-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dube PR, Birnbaumer L, Vazquez G. Evidence for constitutive bone morphogenetic protein-2 secretion by M1 macrophages: Constitutive auto/paracrine osteogenic signaling by BMP-2 in M1 macrophages. Biochem Biophys Res Commun. 2017;491:154–158. doi: 10.1016/j.bbrc.2017.07.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.You M, Li K, Xie Y, Huang L, Zheng X. The Effects of Cerium Valence States at Cerium Oxide Coatings on the Responses of Bone Mesenchymal Stem Cells and Macrophages. Biological trace element research. 2017;179:259–270. doi: 10.1007/s12011-017-0968-4. [DOI] [PubMed] [Google Scholar]
- 31.Li B, et al. In vitro and in vivo responses of macrophages to magnesium-doped titanium. Scientific reports. 2017;7:42707. doi: 10.1038/srep42707. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 32.Muller PA, et al. Crosstalk between muscularis macrophages and enteric neurons regulates gastrointestinal motility. Cell. 2014;158:300–313. doi: 10.1016/j.cell.2014.04.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chung JH, et al. Palmitate promotes the paracrine effects of macrophages on vascular smooth muscle cells: the role of bone morphogenetic proteins. PLoS One. 2012;7:e29100. doi: 10.1371/journal.pone.0029100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bauer M, Weis S, Netea MG, Wetzker R. Remembering Pathogen Dose: Long-Term Adaptation in Innate Immunity. Trends Immunol. 2018;39:438–445. doi: 10.1016/j.it.2018.04.001. [DOI] [PubMed] [Google Scholar]
- 35.Netea MG, Quintin J, van der M, Jos WM. Trained Immunity: A Memory for Innate Host Defense. Cell Host & Microbe. 2011;9:355–361. doi: 10.1016/j.chom.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 36.Calcium Hypothesis of Alzheimer’s disease and brain aging: A framework for integrating new evidence into a comprehensive theory of pathogenesis. Alzheimer’s & dementia: the journal of the Alzheimer’s Association13, 178–182.e117, 10.1016/j.jalz.2016.12.006 (2017). [DOI] [PubMed]
- 37.Chandran, R. et al. Cellular calcium signaling in the aging brain. Journal of chemical neuroanatomy, 10.1016/j.jchemneu.2017.11.008 (2017). [DOI] [PubMed]
- 38.Santulli G, Marks AR. Essential Roles of Intracellular Calcium Release Channels in Muscle, Brain, Metabolism, and Aging. Current molecular pharmacology. 2015;8:206–222. doi: 10.2174/1874467208666150507105105. [DOI] [PubMed] [Google Scholar]
- 39.Serafini N, et al. The TRPM4 channel controls monocyte and macrophage, but not neutrophil, function for survival in sepsis. J Immunol. 2012;189:3689–3699. doi: 10.4049/jimmunol.1102969. [DOI] [PubMed] [Google Scholar]
- 40.Drysdale BE, Yapundich RA, Shin ML, Shin HS. Lipopolysaccharide-mediated macrophage activation: the role of calcium in the generation of tumoricidal activity. J Immunol. 1987;138:951–956. [PubMed] [Google Scholar]
- 41.Desai BN, Leitinger N. Purinergic and Calcium Signaling in Macrophage Function and Plasticity. Frontiers in Immunology. 2014;5:580. doi: 10.3389/fimmu.2014.00580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Myers JT, Swanson JA. Calcium spikes in activated macrophages during Fcgamma receptor-mediated phagocytosis. J Leukoc Biol. 2002;72:677–684. [PubMed] [Google Scholar]
- 43.Racioppi L, Noeldner PK, Lin F, Arvai S, Means AR. Calcium/calmodulin-dependent protein kinase kinase 2 regulates macrophage-mediated inflammatory responses. J Biol Chem. 2012;287:11579–11591. doi: 10.1074/jbc.M111.336032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wang F, et al. Contribution of programmed cell death receptor (PD)-1 to Kupffer cell dysfunction in murine polymicrobial sepsis. American journal of physiology. Gastrointestinal and liver physiology. 2016;311:G237–245. doi: 10.1152/ajpgi.00371.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kinoshita M, et al. In vivo Lipopolysaccharide Tolerance Recruits CD11b+ Macrophages to the Liver with Enhanced Bactericidal Activity and Low Tumor Necrosis Factor-Releasing Capability, Resulting in Drastic Resistance to Lethal Septicemia. Journal of innate immunity. 2017;9:493–510. doi: 10.1159/000475931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kirmizitas A, Meiklejohn S, Ciau-Uitz A, Stephenson R, Patient R. Dissecting BMP signaling input into the gene regulatory networks driving specification of the blood stem cell lineage. Proc Natl Acad Sci USA. 2017;114:5814–5821. doi: 10.1073/pnas.1610615114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kang YJ, et al. Inhibition of erythropoiesis by Smad6 in human cord blood hematopoietic stem cells. Biochem Biophys Res Commun. 2012;423:750–756. doi: 10.1016/j.bbrc.2012.06.031. [DOI] [PubMed] [Google Scholar]
- 48.Shiozawa Y, et al. Erythropoietin couples hematopoiesis with bone formation. PLoS One. 2010;5:e10853. doi: 10.1371/journal.pone.0010853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Li Y, et al. Adaptive immune response in osteoclastic bone resorption induced by orally administered Aggregatibacter actinomycetemcomitans in a rat model of periodontal disease. Molecular oral microbiology. 2010;25:275–292. doi: 10.1111/j.2041-1014.2010.00576.x. [DOI] [PubMed] [Google Scholar]
- 50.Provost KA, Smith M, Arold SP, Hava DL, Sethi S. Calcium restores the macrophage response to nontypeable haemophilus influenzae in chronic obstructive pulmonary disease. American journal of respiratory cell and molecular biology. 2015;52:728–737. doi: 10.1165/rcmb.2014-0172OC. [DOI] [PubMed] [Google Scholar]
- 51.Gronski MA, Kinchen JM, Juncadella IJ, Franc NC, Ravichandran KS. An essential role for calcium flux in phagocytes for apoptotic cell engulfment and the anti-inflammatory response. Cell death and differentiation. 2009;16:1323–1331. doi: 10.1038/cdd.2009.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Berridge MJ, Lipp P, Bootman MD. The versatility and universality of calcium signalling. Nat Rev Mol Cell Biol. 2000;1:11–21. doi: 10.1038/35036035. [DOI] [PubMed] [Google Scholar]
- 53.Gordon D. Ion channels in nerve and muscle cells. Current Opinion in Cell Biology. 1990;2:695–707. doi: 10.1016/0955-0674(90)90113-S. [DOI] [PubMed] [Google Scholar]
- 54.Wang L, Yule DI. Differential regulation of ion channels function by proteolysis. Biochimica et Biophysica Acta (BBA) - Molecular Cell Research. 2018;1865:1698–1706. doi: 10.1016/j.bbamcr.2018.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.National Research Council (U.S.). Committee for the Update of the Guide for the Care and Use of Laboratory Animals., Institute for Laboratory Animal Research (U.S.) & National Academies Press (U.S.). xxv, 220 p (National Academies Press, Washington, D.C., 2011).
- 56.Alatery A, Basta S. An efficient culture method for generating large quantities of mature mouse splenic macrophages. Journal of immunological methods. 2008;338:47–57. doi: 10.1016/j.jim.2008.07.009. [DOI] [PubMed] [Google Scholar]
- 57.Wang C, et al. Characterization of murine macrophages from bone marrow, spleen and peritoneum. BMC Immunology. 2013;14:6. doi: 10.1186/1471-2172-14-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Watkins SC, Salter RD. Functional Connectivity between Immune Cells Mediated by Tunneling Nanotubules. Immunity. 2005;23:309–318. doi: 10.1016/j.immuni.2005.08.009. [DOI] [PubMed] [Google Scholar]
- 59.Freitas CMT, Hamblin GJ, Raymond CM, Weber KS. Naive helper T cells with high CD5 expression have increased calcium signaling. PloS one. 2017;12:e0178799. doi: 10.1371/journal.pone.0178799. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article. Biological reagents will be made available on request.