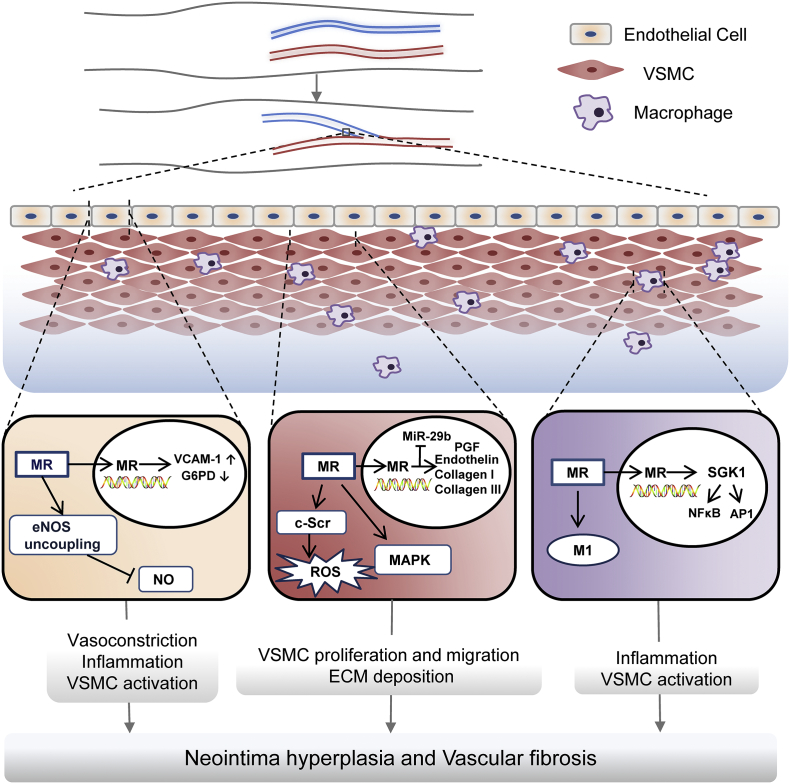
Fig. 2.
Contribution of MR signaling VSMC, endothelial cells and macrophages to vascular access dysfunction. In endothelial cells, MR signaling reduces production and bioavailability of nitric oxide by enhancing eNOS uncoupling, and amplifies inflammation and oxidative stress by promoting endothelial expression of VCAM-1 and inhibiting G6PD, which causes vasoconstriction, inflammation, and VSMC activation. In VSMC, MR exerts non-genomic mineralocorticoid actions, including phosphorylation and activation of MAPK and c-Src, and genomic mineralocorticoid actions, such as upregulation of PGF, endothelin and collagen I/III. In addition, MR signaling may diminish MiR-29b abundance. These effects in VSMC are responsible for VSMC proliferation migration and ECM deposition. In macrophages, MR promotes uncommitted M0 macrophages differentiation to M1 proinflammatory phenotype and activates NFκB and AP1 pathways via SGK1, which can trigger inflammatory response and activate VSMC. All these effects integrate synergistically ultimately resulting in vascular access failure, characterized by neointima hyperplasia and vascular fibrosis. Abbreviations: AP1, activator protein-1; ECM, extracellular matrix; eNOS, endothelial NO synthase; G6PD, glucose-6-phosphate dehydrogenase; MAPK, mitogen-activated protein kinase; MR: mineralocorticoid receptor; NFκB, nuclear factor-Κappa B; PGF, placental growth factor; ROS, reactive oxygen species; SGK-1, serum-and-glucocorticoid-regulated kinase1; VCAM-1, vascular cell adhesion molecule-1; VSMC, vascular smooth muscle cell.