Overview
Introduction
We present the surgical technique for arthroscopic revision posterior cruciate ligament (PCL) reconstruction with use of the modified tibial-inlay double-bundle method without a change of the patient’s position from supine to prone.
Step 1: Graft Preparation
Create the Achilles tendon allograft as a tibial bone block with two femoral bundles.
Step 2: Patient Position
With the patient in the supine position, flexion, abduction, and external rotation of the hip and flexion of the knee 60° to 90° can provide easier access to the popliteal area.
Step 3: Femoral Tunnel Preparation
Make anterolateral and posteromedial femoral tunnels in a shallow-shallow position using an outside-in technique for the anterolateral bundle and the inside-out technique for the posteromedial bundle.
Step 4: Tibial Tunnel Preparation
Make the tibial tunnel with the patient supine with the hip flexed, abducted, and externally rotated and the knee flexed 60° to 90° to provide easier access to the popliteal area.
Step 5: Graft Passage
Using a wire loop, pass the graft through the knee joint posterior to the intercondylar notch into the femoral tunnel.
Step 6: Graft Fixation
Use a cannulated screw with a spiked washer to secure fixation of the bone block to the tibia.
Step 7: Postoperative Rehabilitation
Rehabilitation after a PCL repair is generally more conservative than the accelerated rehabilitation used after an ACL repair.
Results
In our study, twenty-two patients (twenty men and two women; mean age, 37.4 years) were treated with revision PCL reconstruction performed with the described technique and followed for a mean of 39.6 months (range, twenty-four to seventy-two months)14.
Introduction
We present the surgical technique for arthroscopic revision posterior cruciate ligament (PCL) reconstruction with use of the modified tibial-inlay double-bundle method without a change of the patient’s position from supine to prone.
There are many reported arthroscopic techniques for reconstructing the PCL. Most of them are modifications of a transtibial tunnel method through an anterior approach1-5. However, the acute angular turn of the graft at the posterior opening of the tibial tunnel, which has been called the “killer turn,” may result in failure and stretching of the graft6. Therefore, the tibial inlay technique was devised for PCL reconstruction, to avoid the problem of graft abrasion on the tunnel edge and allow the graft to pass easily through the femoral tunnel7. Recently, however, specific advantages of the tibial inlay technique have been proposed8. First, the technique of using remnant fibers of the PCL has become widespread6,9,10. The remnant PCL fibers are interposed between the tunnel edge bone and the graft, thus protecting the graft by cushioning it against abrasion on the posterior tibial edge of the tunnel entrance. Furthermore, this inlay technique reduces the acute angle that the graft takes along its pathway from the joint into the tibial tunnel. The advances in arthroscopic instrument design and surgical techniques have enabled improved clinical outcomes compared with those achieved with the transtibial tunnel method despite the transtibial tunnel method being easier to perform4,5,10.
The tibial inlay technique is preferentially indicated for surgical revision of primary failed PCL reconstruction, and for the primary PCL augmentation and remnant fibers with tensioning. Additionally, this technique has been advocated for patients with chronic PCL rupture with scanty remnant fibers who need double-bundle PCL reconstruction. (If PCL remnant fibers are absent, we prefer to do double-bundle reconstruction rather than single-bundle reconstruction).
The standard tibial inlay technique has several disadvantages. First, the popliteal exposure requires additional surgical dissection. Second, the posterior incision and approach may cause neurovascular complications, such as injury of the popliteal artery and vein. Extra care is especially needed for revision surgery because of the adhesions. Also, the patient is in the prone position for the initial tibial inlay procedure, meaning that his or her position needs to be changed for the remainder of the operation; this both prolongs the operative time and creates additional work for the operative team7. We have modified the tibial inlay technique to eliminate the need to change the patient’s position during surgery11-13.
Our procedure is performed with the following steps.
Step 1: Graft Preparation
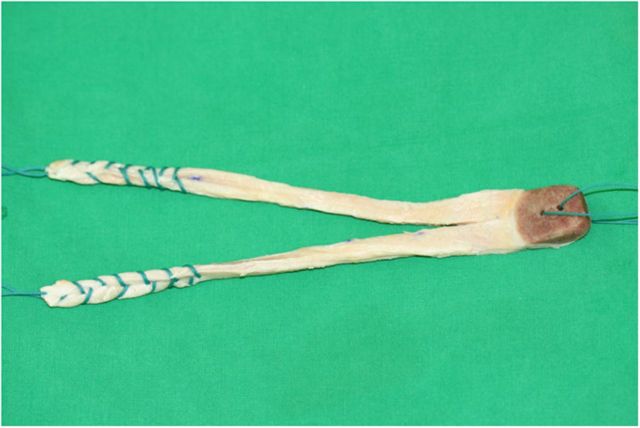
Create the Achilles tendon allograft as a tibial bone block with two femoral bundles (Fig. 1).
Transect the Achilles tendon graft sagittally into two strands, and suture each strand to a diameter of 6 to 9 mm with a locking whipstitch using number-5 nonabsorbable sutures. The strand consisting of the anterolateral bundle is usually prepared to a diameter of 8 to 9 mm, and the strand consisting of the posteromedial bundle is prepared to a diameter of 6 to 7 mm.
Prepare the tibial bone block such that it is 20 mm long, 15 mm wide, and 8 mm thick.
Fig. 1.
The Achilles tendon allograft consists of a tibial bone block and two tendon tails secured with a locking whipstitch with number-5 nonabsorbable suture.
Step 2: Patient Position
With the patient in the supine position, flexion, abduction, and external rotation of the hip and flexion of the knee 60° to 90° can provide easier access to the popliteal area.
Place the patient in a supine position. It should be possible to carry out an anterior arthroscopic or posterior approach to the knee by externally rotating the hip joint. We usually use a posteromedial approach to the knee to prevent injury to the common peroneal nerve.
For the modified tibial inlay technique, perform the arthroscopic operation with the patient in the supine position first. Then tilt the operating table 30°, so that the operatively treated knee is lower than the contralateral knee, and place the lower limb on a side-table with the hip flexed, abducted, and externally rotated and the knee flexed 60° to 90°. This facilitates access to the popliteal area.
Step 3: Femoral Tunnel Preparation
Make anterolateral and posteromedial femoral tunnels in a shallow-shallow position using an outside-in technique for the anterolateral bundle and the inside-out technique for the posteromedial bundle (Video 1).
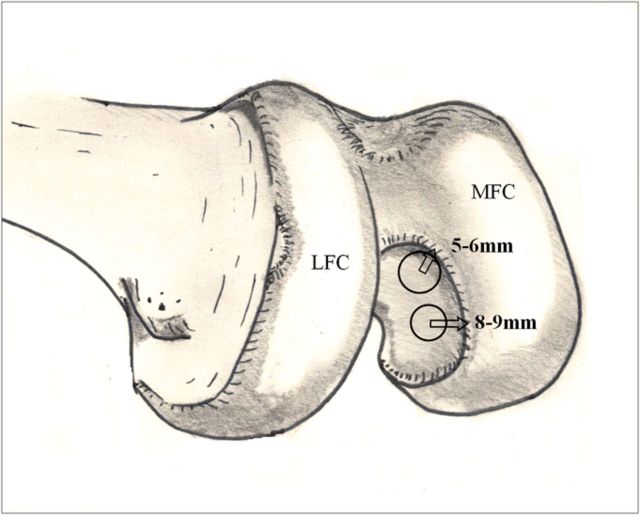
Place the center of the anterolateral femoral tunnel 5 to 6 mm proximal to the margin of the articular cartilage of the femoral condyle at approximately the 1 to 1:30 o’clock position in a right knee (Fig. 2).
Place the center of the posteromedial femoral tunnel 8 to 9 mm proximal to the margin of the distal articular cartilage of the femoral condyle at the 3 o’clock position in a right knee (Fig. 2).
Make the femoral tunnel for the anterolateral bundle using the outside-in technique by inserting a guide pin via the medial-side incision underneath the vastus medialis.
Create the femoral tunnel for the posteromedial bundle from an accessory anterolateral portal using an inside-out technique.
Remove the hardware, but preserve the previous PCL graft or the original PCL remnant bundle if possible. Reuse the primary tunnel if the position of the tunnel for the anterolateral bundle is correct. When tunnel placement is entirely incorrect, create a new tunnel at the correct position. The most difficult cases are those in which the tunnel position is somewhat but not entirely incorrect. In such cases, first make a tunnel with a dilator to avoid generating a large bone defect and to preserve the original graft. On occasion, an autogenous corticocancellous bone graft is impacted between the graft and the tunnel when the tunnel is widened.
Chamfer the internal orifice of the femoral tunnel edge with rasps to prevent acute-angle impingement, which may lead to premature wear of the graft.
Pass a 21-gauge wire loop through the femoral tunnel and direct it toward the just medial side of the remnant of the PCL on the tibia. It is used later to pass the graft from the area of the tibial insertion of the PCL into the femoral tunnel.
Fig. 2.
The center of the anterolateral femoral tunnel is placed 5 to 6 mm proximal to the articular cartilage at the one o’clock position. The posteromedial tunnel is placed 8 to 9 mm proximal to the margin of the distal articular cartilage, at the 3 o’clock position in a right knee. MFC = medial femoral condyle, and LFC = lateral femoral condyle.
Video 1.
The femoral tunnel for the anterolateral bundle is prepared with an outside-in technique, and the femoral tunnel for the posteromedial bundle is made with an inside-out technique.
Step 4: Tibial Tunnel Preparation
Make the tibial tunnel with the patient supine with the hip flexed, abducted, and externally rotated and the knee flexed 60° to 90° to provide easier access to the popliteal area.
Following the arthroscopic operation of the anterior aspect of the knee, tilt the operating table 30° so that the operatively treated knee is lower than the contralateral knee and then place the lower limb on a side-table, with the hip flexed, abducted, and externally rotated and the knee flexed 60° to 90° (Fig. 3, Video 2).
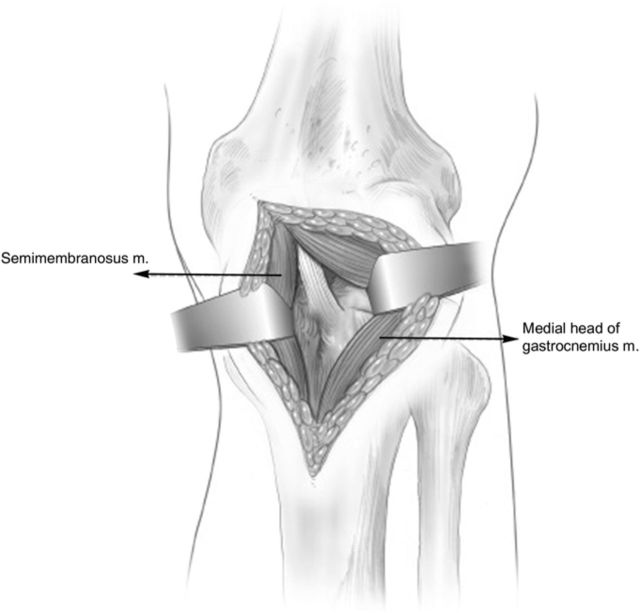
Identify the interval between the medial head of the gastrocnemius muscle and the semimembranosus tendon and develop it bluntly.
Retract the semimembranosus and semitendinosus tendons toward the medial side. Retract the gastrocnemius muscle laterally, protecting the popliteal neurovascular structures (Fig. 4).
If the branches of the inferior medial geniculate artery and vein are encountered near the midposterior portion of the capsule, ligate them securely.
Detach the popliteus muscle subperiosteally from the posteromedial surface of the proximal part of the tibia, and palpate the PCL tibial attachment site.
By moving the wire loop that you inserted previously, confirm the PCL insertion site.
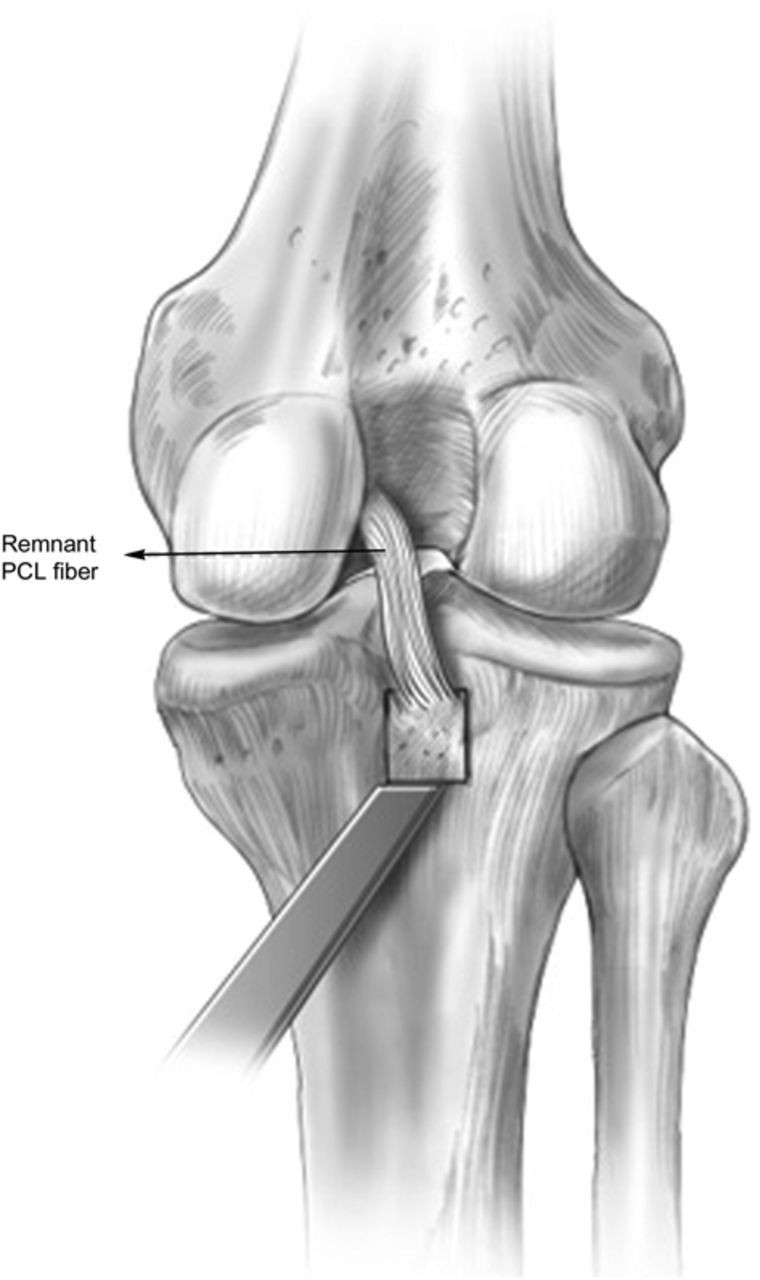
Then incise the posterior aspect of the knee capsule adjacent to the medial femoral condyle, and preserve the remnant PCL fibers.
Demarcate the tibial attachment of the PCL as a 1.5 × 2-cm area with an osteotome, and detach a 7-mm-thick bone block from distal to the proximal area using a 1.2 to 1.5-cm-wide curved osteotome (Fig. 5).
At the junction of bone and the remnant PCL, place a number-5 nonabsorbable Ethibond suture (Ethicon, Somerville, New Jersey) for easy distal traction of the remnant PCL.
Fig. 3.
The operating table is tilted down on the affected side for the posterior approach.
Fig. 4.
The medial border of the medial head of the gastrocnemius muscle is identified, and the interval between it and the semimembranosus tendon is developed, exposing the posterior aspect of the joint capsule.
Fig. 5.
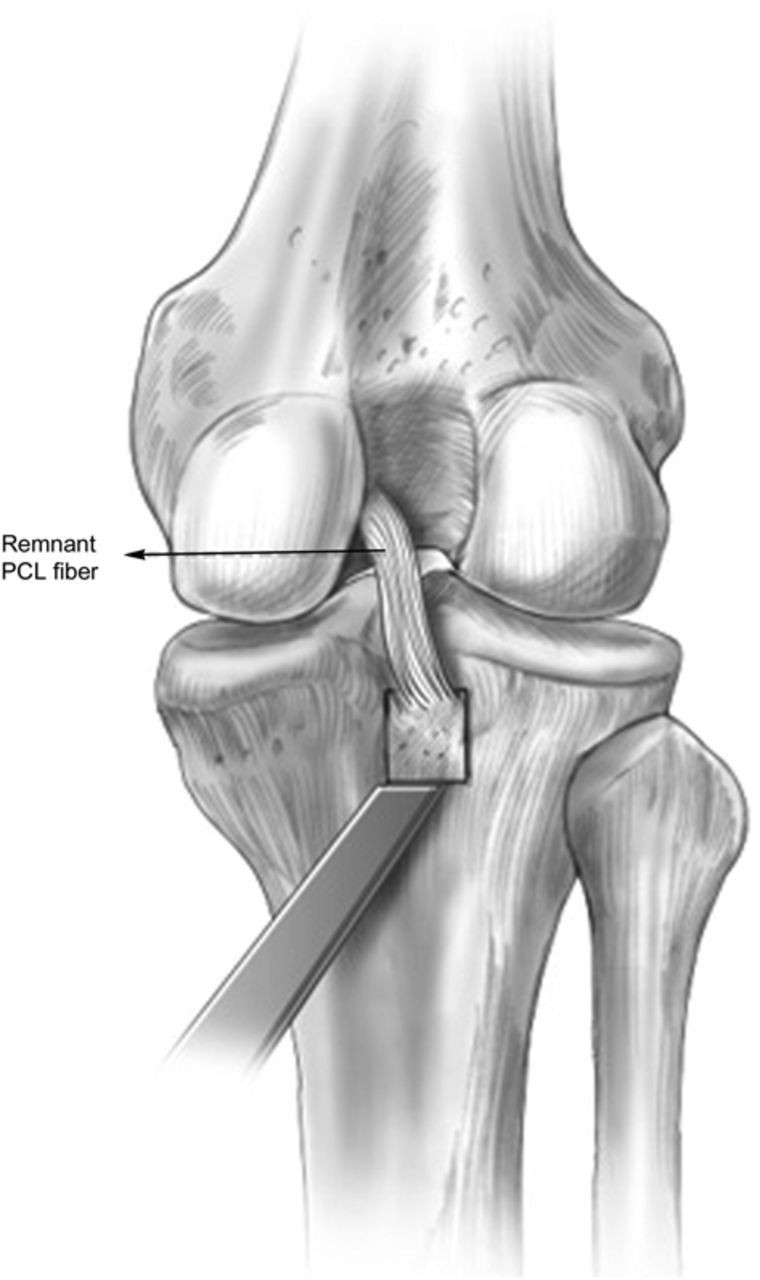
The bone block of the tibial attachment site of the PCL is detached with use of a curved osteotome, and a trough is created.
Video 2.
The operating table is tilted 30° to access the popliteal area.
Step 5: Graft Passage
Using a wire loop, pass the graft through the knee joint posterior to the intercondylar notch into the femoral tunnel.
Make an osseous trough at the bone-block detachment site.
Pass the tendon graft traction suture for the anterolateral bundle with a wire loop first and then pass the suture for the posteromedial bundle from the PCL tibial insertion area into the femoral tunnel. Pull the graft up through the knee joint into the femoral tunnel.
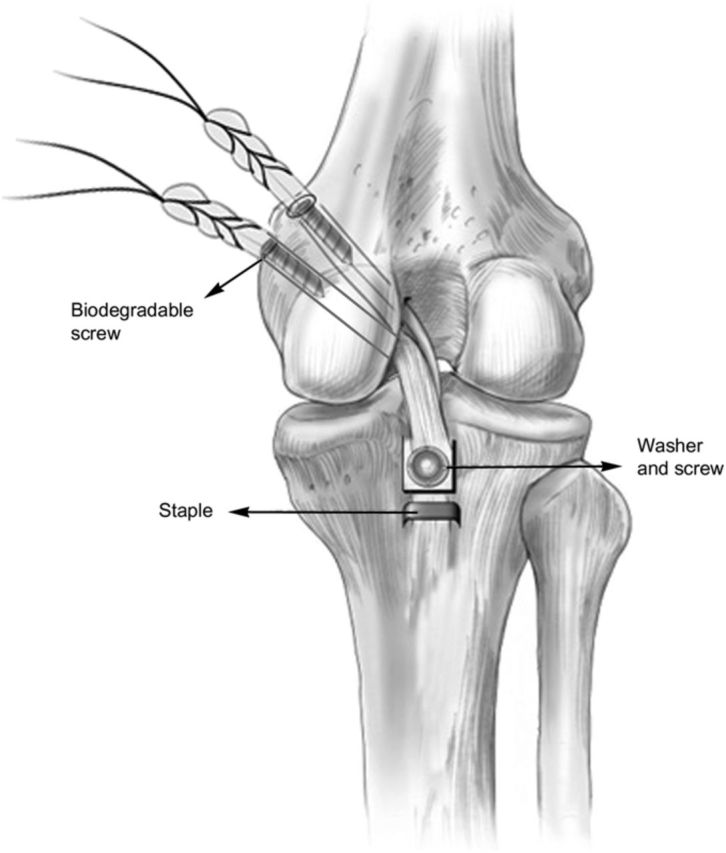
Step 6: Graft Fixation
Use a cannulated screw with a spiked washer to secure fixation of the bone block to the tibia.
Usually, the tibial side bone block is fixed first.
Fit the Achilles graft bone block into the osseous trough, and pull the detached native host tibial bone block with the remnant fiber of the PCL with tension over the Achilles graft bone block.
Use a 5 or 6.5-mm cannulated screw with a spiked washer to secure fixation of the bone block to the tibia (Fig. 6).
Cyclically load the graft with 67 N of tension by moving the knee through a passive range of motion twenty times.
Fix biodegradable interference screws to the femoral tunnels with anteriorly directed force applied to the proximal part of the tibia and the knee joint flexed 70° to 90°.
Apply a long leg splint to hold the knee in extension.
Fig. 6.
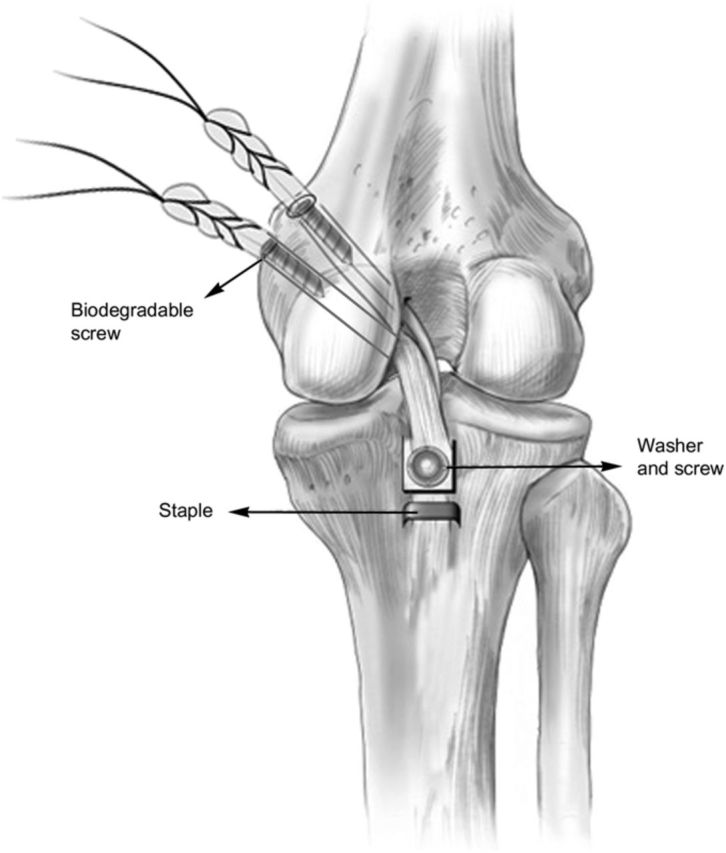
A 6.5-mm cannulated screw and a spiked washer are used to fix the graft to the tibia.
Step 7: Postoperative Rehabilitation
Rehabilitation after a PCL repair is generally more conservative than the accelerated rehabilitation used after an ACL repair.
For the first two or three weeks after the surgery, a long leg splint or PCL brace is used to hold the knee in extension.
The patient is encouraged to perform gradual passive flexion exercises from the third, fourth, or fifth postoperative day until the sixth postoperative week. The patient performs these exercises using both hands to support the proximal part of the tibia or the exercises can be performed by another person with the patient in the prone position to prevent posterior translation of the tibia by gravity (Video 3).
Soon after the procedure, straight-leg raising and quadriceps-setting exercises are begun due to the agonistic function of the quadriceps to the PCL.
Strengthening of the hamstring muscles is not allowed until the fourth month after surgery.
The patient remains partial weight-bearing, with use of crutches, until the sixth postoperative week, and full weight-bearing is allowed with the limb in as extended a position as pain permits.
By six months postoperatively, jogging can be initiated if the knee is asymptomatic with this activity.
Video 3.
The patient is encouraged to perform gradual passive flexion exercises to prevent posterior translation of tibia by gravity. The exercises can also be performed by another person, with the patient in the prone position.
Results
In our study, twenty-two patients (twenty men and two women; mean age, 37.4 years) were treated with revision PCL reconstruction performed with the described technique and followed for a mean of 39.6 months (range, twenty-four to seventy-two months)14. The side-to-side differences during posterior stress radiography improved from 9.9 ± 2.8 mm preoperatively to 2.8 ± 1.8 mm at the time of the latest follow-up (p < 0.001). The subjective and objective clinical scores at the latest follow-up evaluation were significantly better than the preoperative scores (p < 0.001).
What to Watch For
Indications
Recurrent pathological laxity (a side-to-side difference of >5 mm in posterior translation as demonstrated by posterior stress radiography with a TELOS stress device) that is painful during activities of daily living or athletic activities.
Failure of conservative treatment consisting of physiotherapy and quadriceps-strengthening exercises for at least three months.
Persistent pain, functional disability, and instability preventing the patient from returning to activities such as sprinting and descending stairs.
Contraindications
Advanced osteoarthritis of the knee.
Severe arthrofibrosis.
Active infection.
Severe malalignment of the affected limb.
Pitfalls & Challenges
The most serious complication of the tibial inlay technique is injury of the popliteal artery and vein during the operation. The surgeon needs to take a more cautious approach for posterior knee dissection, especially in the case of revision surgery, as postoperative scar formation and adhesion of the primary PCL repair might have caused an anatomically abnormal position of the popliteal artery and vein.
Posterior knee incision and dissection of deep layers can result in deep scar and adhesion formation and consequently delay the restoration of range of motion due to flexion contracture or limitation of flexion to 140°. However, this problem can usually be solved by constant passive range-of-motion exercise.
Associated posterolateral rotatory instabilities should be surgically corrected during PCL reconstruction to prevent graft failure due to abnormal lateral tibiofemoral joint opening.
The previous PCL graft or the original PCL remnant bundle should be preserved as much as possible because revision usually demonstrates preserved contour and continuity of the PCL.
A bifid Achilles tendon allograft is currently our first choice for revision PCL surgery. However, the Achilles tendon is not thick enough in some cases, and in those cases an additional semitendinosus autograft is a good option for augmentation for revision PCL surgery.
Clinical Comments
What is the most common cause of failure of PCL reconstruction?
What are the advantages of a tibial-inlay method for revision PCL reconstruction?
What prophylactic rehabilitation regimens are effective for preventing PCL graft loosening or failure of PCL reconstruction?
Based on an original article: J Bone Joint Surg Am. 2012 Mar 21;94(6):516-22.
Disclosure: None of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of any aspect of this work. None of the authors, or their institution(s), have had any financial relationship, in the thirty-six months prior to submission of this work, with any entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. Also, no author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1. Mariani PP Adriani E Santori N Maresca G. Arthroscopic posterior cruciate ligament reconstruction with bone-tendon-bone patellar graft. Knee Surg Sports Traumatol Arthrosc. 1997;5(4):239-44. [DOI] [PubMed] [Google Scholar]
- 2. Pinczewski LA Thuresson P Otto D Nyquist F. Arthroscopic posterior cruciate ligament reconstruction using four-strand hamstring tendon graft and interference screws. Arthroscopy. 1997 Oct;13(5):661-5. [DOI] [PubMed] [Google Scholar]
- 3. Schulte KR Chu ET Fu FH. Arthroscopic posterior cruciate ligament reconstruction. Clin Sports Med. 1997 Jan;16(1):145-56. [DOI] [PubMed] [Google Scholar]
- 4. Ahn JH Chung YS Oh I. Arthroscopic posterior cruciate ligament reconstruction using the posterior trans-septal portal. Arthroscopy. 2003 Jan;19(1):101-7. [DOI] [PubMed] [Google Scholar]
- 5. Ahn JH Yoo JC Wang JH. Posterior cruciate ligament reconstruction: double-loop hamstring tendon autograft versus Achilles tendon allograft—clinical results of a minimum 2-year follow-up. Arthroscopy. 2005 Aug;21(8):965-9. [DOI] [PubMed] [Google Scholar]
- 6. Kim SJ Kim TE Jo SB Kung YP. Comparison of the clinical results of three posterior cruciate ligament reconstruction techniques. J Bone Joint Surg Am. 2009 Nov;91(11):2543-9. [DOI] [PubMed] [Google Scholar]
- 7. Berg EE. Posterior cruciate ligament tibial inlay reconstruction. Arthroscopy. 1995 Feb;11(1):69-76. [DOI] [PubMed] [Google Scholar]
- 8. Kim SH Lee HJ Jung HJ Lee JS Kim KS. Less femoral lift-off and better femoral alignment in TKA using computer-assisted surgery. Knee Surg Sports Traumatol Arthrosc. 2013 Oct;21(10):2255-62. Epub 2012 Oct 6. [DOI] [PubMed] [Google Scholar]
- 9. Ahn JH Yang HS Jeong WK Koh KH. Arthroscopic transtibial posterior cruciate ligament reconstruction with preservation of posterior cruciate ligament fibers: clinical results of minimum 2-year follow-up. Am J Sports Med. 2006 Feb;34(2):194-204. Epub 2005 Nov 22. [DOI] [PubMed] [Google Scholar]
- 10. Jung YB Jung HJ Song KS Kim JY Lee HJ Lee JS. Remnant posterior cruciate ligament-augmenting stent procedure for injuries in the acute or subacute stage. Arthroscopy. 2010 Feb;26(2):223-9. Epub 2009 Dec 21. [DOI] [PubMed] [Google Scholar]
- 11. Jung YB Tae SK Jung HJ Lee KH. Replacement of the torn posterior cruciate ligament with a mid-third patellar tendon graft with use of a modified tibial inlay method. J Bone Joint Surg Am. 2004 Sep;86-A(9):1878-83. [DOI] [PubMed] [Google Scholar]
- 12. Jung YB Jung HJ Tae SK Lee YS Lee KH. Reconstruction of the posterior cruciate ligament with a mid-third patellar tendon graft with use of a modified tibial inlay method. J Bone Joint Surg Am. 2005 Sep;87(Pt 2)(Suppl 1):247-63. [DOI] [PubMed] [Google Scholar]
- 13. Jung YB Jung HJ Tae SK Lee YS Yang DL. Tensioning of remnant posterior cruciate ligament and reconstruction of anterolateral bundle in chronic posterior cruciate ligament injury. Arthroscopy. 2006 Mar;22(3):329-38. [DOI] [PubMed] [Google Scholar]
- 14. Lee SH Jung YB Lee HJ Jung HJ Kim SH. Revision posterior cruciate ligament reconstruction using a modified tibial-inlay double-bundle technique. J Bone Joint Surg Am. 2012 Mar 21;94(6):516-22. [DOI] [PubMed] [Google Scholar]