Abstract
Objective
Endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) is a minimally invasive procedure for pulmonary and mediastinal diseases. This study compared the performance of a novel 19-G needle with a 21- or 22-G needle.
Patients and Methods
Eleven patients at Okayama Medical Center were enrolled retrospectively between April and December 2017. Enlarged lymph nodes and a pulmonary nodule were sampled with both 19-G and 21- or 22-G needles in nine patients. Two patients underwent biopsies for suspected lymphoma with only the 19-G needle. We examined their medical records on the diagnosis, size of the lymph nodes and pulmonary nodule, and complications.
Results
The median longest diameter of the 13 lymph nodes (8 #7, 4 #4R, and 1 #11) and 1 pulmonary nodule (right segment 6) in the 11 patients was 31.6 mm (range, 10.4-45.0 mm). Definitive diagnoses were made using the 19-G needle in nine patients. EBUS-TBNA with a 19-G needle resulted in successful diagnoses of one case of retinal hemangioblastoma, one case of tuberculous lymphadenitis, and one case of lung adenocarcinoma, as well as the evaluation of the programmed death-ligand 1 (PD-L1) expression following initial negative findings after a 21- or 22-G biopsy. A small pulmonary nodule (lung squamous cell carcinoma) with negative findings after a 19-G biopsy was diagnosed with a 22-G biopsy. Two suspected lymphoma patients were diagnosed with a 19-G needle: one had lymphoma and the other sarcoidosis. Three patients were diagnosed with sarcoidosis using both the 19-G and 21- or 22-G needles.
Conclusion
EBUS-TBNA with a 19-G needle was useful for diagnosing retinal hemangioblastoma and tuberculous lymphadenitis as well as for PD-L1 testing after 21- and 22-G biopsies were unsuccessful.
Keywords: endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA), 19-G flexible needle
Introduction
Endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) is a minimally invasive diagnostic tool that is equivalent if not superior to mediastinoscopy for the evaluation of the mediastinal and hilar lymph nodes (1, 2). In addition to mediastinal lymph node staging of patients with lung cancer, it is useful for diagnosing other pulmonary and mediastinal diseases (3, 4). EBUS-TBNA using a Flex 19-G needle has afforded very high diagnostic yields for evaluating malignancy and sarcoidosis (5, 6). However, few studies have evaluated whether or not a 19-G needle has a higher diagnostic yield than a 21- or 22-G needle.
We compared the performance of a novel 19-G flexible needle with that of 21- or 22-G needles. To our knowledge, this is the first report in which a flexible 19-G needle was used to confirm the pathological diagnosis via EBUS-TBNA in Japan after initial negative results were obtained with 21- or 22-G needles.
Materials and Methods
Patient population and study design
This retrospective study enrolled all 11 patients at Okayama Medical Center who underwent EBUS-TBNA with a 19-G needle to diagnose pulmonary or mediastinal disease between April and December 2017. Enlarged lymph nodes and a pulmonary nodule were examined with both an initial 21- or 22-G ViziShot 2 needle (Olympus, Tokyo, Japan) and a 19-G ViziShot FLEX needle (Olympus) in nine patients; the remaining two patients with suspected lymphoma underwent a biopsy only with the 19-G ViziShot FLEX needle. When cores were obtained with a 21- or 22-G ViziShot 2 needle and 19-G ViziShot needle, the samples were sent separately for histological analyses. Chest radiographs and computed tomography (CT) before bronchoscopic examinations revealed at least 1 enlarged lymph node or pulmonary nodule ≥10 mm along the long axis in all of the patients.
The study was approved by the Institutional Ethics Committee of the National Hospital Organization, Okayama Medical Center on January 9, 2018 (Approval No. H29-RINKEN-ZINSOKU-082).
Bronchoscopy procedure
All of the bronchoscopic procedures were performed on an inpatient basis under local anesthesia with mild conscious sedation. A total of 5 mL of 2% (w/v) lidocaine was sprayed into the pharynx, and another 5 mL of 2% (w/v) lidocaine was administered through the channel during the procedures. The patients were monitored by electrocardiography, pulse oximetry, and blood pressure readings before starting anesthesia. The bronchoscope was inserted orally during fentanyl- and midazolam-induced conscious sedation. A conventional flexible bronchoscope (BF-P260 bronchovideoscope; Olympus) was used, and intubation was achieved using a siliconized uncuffed tracheal tube with an inside diameter of 7.5 mm (Portex; Smiths Medical, St. Paul, USA). Following conventional bronchoscopy, EBUS-TBNA was performed using an endobronchial ultrasound bronchoscope with a convex probe (BF-UC260F-OL8; Olympus).
Specimen handling
The samples were handled in the following manner: The aspirated material was pushed out of the puncture needle, smeared on a watch glass, and immediately evaluated by an on-site cytopathologist using a BioevaluatorⓇ (Murazumi Industrial, Osaka, Japan) (7). The number of needle biopsies performed was decided according to the rapid on-site evaluation (ROSE) method. Once adequate quantities of cells were obtained for a pathological diagnosis on ROSE, the needle biopsy was considered complete. More than half of the smears were stained using Diff-quickⓇ rapid staining (Kookje Scientific Products, Tokyo, Japan). The remaining samples were fixed in 10% formalin, paraffin-embedded, stained with Papanicolaou stain, and evaluated histologically.
Results
Table 1 summarizes the patient characteristics. There were eight men and three women. Their median age was 68 (range, 51-87) years. Pathological diagnoses were made using EBUS-TBNA in 10 patients: 2 lung cancers (adenocarcinoma and squamous cell carcinoma); 4 cases of sarcoidosis; and 1 case each of large-cell neuroendocrine carcinoma, lymphoma, retinal hemangioblastoma, and tuberculous lymphadenitis. A pathological diagnosis could not be made in one patient whose sputum samples became positive for Mycobacterium tuberculosis after EBUS-TBNA. The lymph nodes and pulmonary nodule (n=14) consisted of eight subcarinal, four right lower paratracheal, and one right hilar lymph nodes as well as one pulmonary nodule in right segment 6 (Table 2). The mean size of the enlarged lymph nodes and pulmonary nodule, measured over the long axis using CT, was 31.6 (range, 10.4-45.0) mm (Table 2).
Table 1.
Patient Characteristics.
| Characteristic | Value |
|---|---|
| Number of patients | 11 |
| Male/female, n | 8/3 |
| Median age (range), years | 68 (51-87) |
| Pathological diagnosis, n | |
| Lung cancer | 2 |
| Large-cell neuroendocrine carcinoma | 1 |
| Lymphoma | 1 |
| Retinal hemangioblastoma | 1 |
| Sarcoidosis | 4 |
| Tuberculous lymphadenitis | 1 |
| Indefinite | 1 |
Table 2.
Characteristics of the Lymph Nodes and Pulmonary Nodule Biopsied Using EBUS-TBNA.
| Characteristic | Value (range) |
|---|---|
| Number | 14 |
| Enlarged lymph node stationsa (4R/7/11), n | 4/8/1 |
| Pulmonary nodule stationb (right S6) | 1 |
| Longest diameter (range), mm | 31.6 (10.4-45.0) |
The lymph nodea and pulmonary noduleb stations were defined as follows: 4R, right lower paratracheal node; 7, subcarinal nodes; 11, N1 nodes; S6, segment 6.
Table 3 compares the performance of the novel 19-G needle with that of a 21- or 22-G gauge needle. The use of the 19-G needle resulted in the diagnosis of one retinal hemangioblastoma (Fig. 1), one tuberculous lymphadenitis, and one lung adenocarcinoma for evaluating programmed death-ligand 1 (PD-L1) expression following initially negative findings with 21- or 22-G needle EBUS-TBNA (Supplementary material 1). The small pulmonary nodule (lung squamous cell carcinoma) showed negative 19-G findings but was ultimately diagnosed with 22-G needle EBUS-TBNA (Fig. 2). Of the two patients with suspected lymphoma, one had lymphoma and the other sarcoidosis, both of which were diagnosed with 19-G needle EBUS-TBNA. The lymphoid cells showed positive immunohistochemical staining for cluster of differentiation (CD) 20. They were negative for CD3, CD 5, and CD10 and demonstrated high Ki-67 staining. Therefore, we made a diagnosis of diffuse large B cell lymphoma. Three patients were diagnosed with sarcoidosis with both the 19-G and 21- or 22-G needles. The quality of specimens obtained with each needle is showed in Supplementary material 2. There were no major complications in this study. Two cases are described in detail below.
Table 3.
Diagnostic Yields of EBUS-TBNA.
| Clinical diagnosis | Target lesions | Puncturesa (n) | 19G | 21G or 22G | |
|---|---|---|---|---|---|
| Case 1 | Retinal hemangioblastoma | #7 #11 |
2 1 |
Positiveb | Negativec |
| Case 2 | Lung squamous cell cancer | S6 | 3 | Negativec | Positiveb |
| Case 3 | Lung adenocarcinoma | #4R #7 |
1 2 |
Positiveb | Negativec |
| Case 4 | LCNEC | #4R | 2 | Positiveb | Positiveb |
| Case 5 | Lymphoma | #4R | 3 | Positiveb | - |
| Case 6 | Sarcoidosis | #7 | 2 | Positiveb | Positiveb |
| Case 7 | Sarcoidosis | #7 | 2 | Positiveb | Positiveb |
| Case 8 | Sarcoidosis | #7 | 1 | Positiveb | Positiveb |
| Case 9 | Sarcoidosis | #7 | 3 | Positiveb | - |
| Case 10 | Tuberculous lymphadenitis | #4R #7 |
2 2 |
Positiveb | Negativec |
| Case 11 | Tuberculous lymphadenitis | #7 | 1 | Negativec | Negativec |
Lymph node stations and pulmonary nodule are defined as follows: 4R, right lower paratracheal node; 7, subcarinal nodes; 11, N1 nodes; S6, segment 6. aPuncture performed with a 19G and 21G or 22G needle. bPositive pathologically. cNegative, not diagnosed pathologically.
EBUS-TBNA: endobronchial ultrasound-guided transbronchial needle aspiration, LCNEC: large-cell neuroendocrine carcinoma, 19G: 19 gauge needle, 21G or 22G: 21 or 22 gauge needle
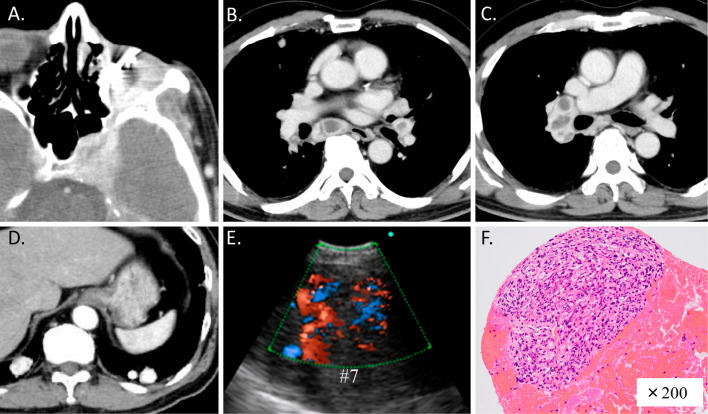
Figure 1.
A patient who had undergone ophthalmectomy for left retinal hemangioblastoma (A) developed mediastinal and bilateral hilar lymphadenopathy (B, C) and multiple hypervascular pulmonary nodules (D) on chest CT. Endobronchial ultrasound showed a hypervascular subcarinal node (#7) (E). The specimen obtained using 19-G EBUS-TBNA was observed to have a network of thin, vascular capillary-like channels lined by endothelial cells and pericytes (F). Hematoxylin and Eosin staining, 200×.
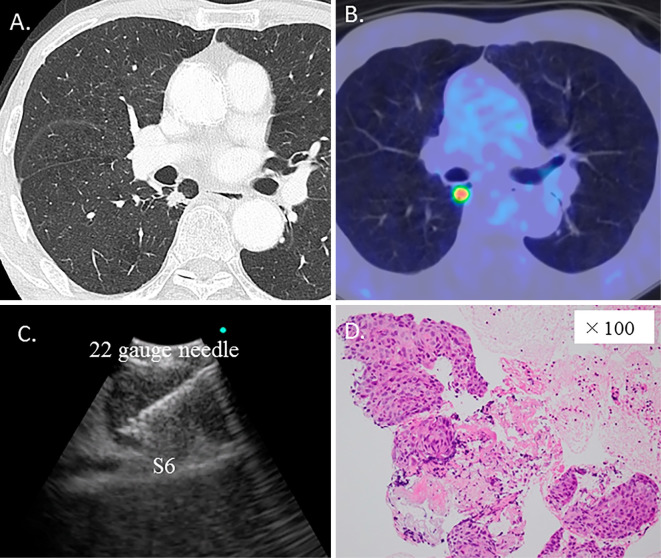
Figure 2.
A patient had a 10-mm pulmonary nodule (right segment 6) measured on the long axis after first-line carboplatin plus nab-paclitaxel chemotherapy on chest CT (A) and positron emission tomography (B). The specimen obtained using 22-G EBUS-TBNA (C) was found to be squamous cell carcinoma, (D) although the findings had been negative on a 19-G needle biopsy. Hematoxylin and Eosin staining, 100×.
Case 1
A 68-year-old man who had undergone ophthalmectomy for left retinal hemangioblastoma (Fig. 1A) showed mediastinal and bilateral hilar lymphadenopathy (Fig. 1B and C) and multiple pulmonary nodules (Fig. 1D) on chest CT performed 30 years after the surgery and 2 years after radiation therapy. Endobronchial ultrasound images showed hypervascular lymph nodes (Fig. 1E). The specimen obtained with a 19-G needle after an initially negative biopsy on EBUS-TBNA with a 22-G needle revealed a network of thin, vascular capillary-like channels lined by endothelial cells and pericytes (Fig. 1F). The cells were found to be retinal hemangioblastoma based on positive CD34 and Adipophilin staining. The cells showed negative staining for CD7, CD20, CD56, CD10, EMA, and Synaptophysin. The pulmonary nodules obtained at video-assisted thoracoscopic surgery had similar pathological characteristics compared to the EBUS-TBNA results.
Case 2
An 80-year-old man with a history of lung squamous cell carcinoma presented with progression of a pulmonary nodule (right segment 6) that measured 10 mm in the long axis after first-line carboplatin plus nab-paclitaxel chemotherapy on chest CT (Fig. 2A) and positron emission tomography (Fig. 2B). The specimen obtained by EBUS-TBNA (Fig. 2C) revealed squamous cell carcinoma (Fig. 1D) using a 22-G needle, although the findings had been negative with a 19-G needle.
Discussion
EBUS-TBNA using a 19-G needle can provide sufficient tissue for a histopathological diagnosis of malignancy and sarcoidosis (8). The tissue samples obtained from EBUS-TBNA are adequate for cytological, immunohistochemical, and molecular lung cancer typing (9, 10). A previous study found that quality of the cell block samples was very good and allowed for the performance of an anaplastic lymphoma kinase assay and ROS proto-oncogene 1 and PD-L1 typing, which tend to require relatively large samples (11). According to the 2016 CHEST Guideline, the use of either a 21-or 22-G needle is acceptable in patients undergoing EBUS-TBNA (12). In cases of a solid pancreatic mass, Sakamoto reported that fine-needle aspiration (FNA) using a 25-G needle was more efficient than that using 22- and 19-G needles (13). Furthermore, Nakai showed that the slow-pull technique was associated with less contamination with blood and a potentially increased diagnostic yield compared with the suction technique in pancreatic solid masses, especially with a 25-G FNA needle (14). Regarding EBUS-TBNA, however, data concerning 25-G needles or aspiration techniques are insufficient at present; a large-scale study may therefore be of interest.
In a preclinical evaluation comparing a novel 19-G flexible needle with a commercial 22-G EBUS-TBNA sampling needle, the samples collected with the 19-G needle were larger and had less blood contamination than those obtained with a 22-G needle (15). In our study, the use of the 19-G needle also provided sufficient tissue samples with less blood contamination that proved useful for diagnosing retinal hemangioblastoma, lung adenocarcinoma, and tuberculous lymphadenitis and for evaluating the PD-L1 expression in specimens whose findings had initially been negative with a 21- or 22-G needle. However, 19-G and 21- or 22-G needle EBUS-TBNA showed similar diagnostic yields in other patients (Table 3). Whether or not the use of a 19-G flexible needle is indeed more effective than a 21- or 22-G needle is therefore unclear based on these results. A larger study is needed to confirm our findings.
In our experience, 19-G needle EBUS-TBNA is useful clinically for diagnosing retinal hemangioblastoma, which can occur sporadically or as a manifestation of von Hippel-Lindau syndrome (Fig. 1). The tumors are hypervascular histopathologically (16). The sample obtained from a 22-G needle can be too small for an evaluation in some cases, but that using a 19-G needle is sufficient for a diagnosis because of the larger sample size and reduced risk of blood contamination. To our knowledge, this is the first report of a retinal hemangioblastoma with mediastinal and hilar lymph node metastasis being diagnosed using EBUS-TBNA with a 19-G needle.
In the present study, EBUS-TBNA with a 19-G needle resulted in successful diagnoses of tuberculous lymphadenitis, lymphoma, and lung adenocarcinoma as well as for evaluating the PD-L1 expression. However, a small pulmonary nodule (lung squamous cell carcinoma) with a negative 19-G needle biopsy was diagnosed with a 22-G needle EBUS-TBNA (Fig. 2). In that case, the pulmonary nodule in right segment 6 measured 10 mm along the long axis using CT. The 22-G ViziShot 2 needle has a sharper tip, reducing the puncture force required to sample calcified lymph nodes. We were therefore able to puncture the small pulmonary nodule with the 22-G ViziShot 2 needle despite difficulties achieving a smooth puncture using the 19-G ViziShot FLEX needle. The 21- or 22-G ViziShot 2 needle might be useful for such small target lesions.
One limitation associated with this study is the potential retrospective bias; another is the small number of subjects. Based on the present findings, possible indications of EBUS-TBNA with a 19-G ViziShot FLEX needle may include retinal hemangioblastoma and lymphoma, which are diagnosed by a large sample and reduced blood contamination. However, we must consider the high cost and difficulty associated with puncture performed using such a large-caliber needle. A prospective large-scale randomized study comparing the 21- or 22-G ViziShot 2 with a 19-G ViziShot FLEX needle might be of interest.
Conclusion
EBUS-TBNA with a 19-G needle was useful for diagnosing retinal hemangioblastoma and tuberculous lymphadenitis as well as for PD-L1 testing after 21-G and 22-G biopsies were unsuccessful.
The authors state that they have no Conflict of Interest (COI).
Supplementary Materials
EBUS-TBNA, endobronchial ultrasound-guided transbronchial needle aspiration; LCNEC, large-cell neuroendocrine carcinoma; 19G, 19 gauge needle; 21G or 22G, 21 or 22 gauge needle; a Negative, not diagnosed pathologically.
The specimen obtained via endobronchial ultrasound-guided transbronchial needle aspiration using a 19-gauge needle contained adenocarcinoma cells more than 21-gauge needle (hematoxylin-eosin staining) (A), (B). Confirmation of PD-L1 expression (1–24% cells) in the 19-gauge needle material (PD-L1 tumor membrane staining, ×200) (C).
Acknowledgement
We thank Dr. Keina Nagakita, Dr. Yoko Shinno, Dr. Toshiro Yonei and Dr. Toshio Sato for performing the bronchoscopic examinations and providing helpful discussion. We thank Mr. Satoshi Fukuda and Ms. Naomi Hiramoto for their cytoScreen expertise.
References
- 1. Yasufuku K, Pierre A, Darling G, et al. A prospective controlled trial of endobronchial ultrasound-guided transbronchial needle aspiration compared with mediastinoscopy for mediastinal lymph node staging of lung cancer. J Thorac Cardiovasc Surg 142: 1393-1400, 2011. [DOI] [PubMed] [Google Scholar]
- 2. Ernst A, Anantham D, Eberhardt R, et al. Diagnosis of mediastinal adenopathy-real-time endobronchial ultrasound guided needle aspiration versus mediastinoscopy. J Thorac Oncol 3: 577-582, 2008. [DOI] [PubMed] [Google Scholar]
- 3. Nakajima T, Yasufuku K. How I do it--optimal methodology for multidirectional analysis of endobronchial ultrasound-guided transbronchial needle aspiration samples. J Thorac Oncol 6: 203-206, 2011. [DOI] [PubMed] [Google Scholar]
- 4. Wohlschläger J, Darwiche K, Ting S, et al. Rapid on-site evaluation (ROSE) in cytological diagnostics of pulmonary and mediastinal diseases. Pathologe 33: 308-315, 2012. [DOI] [PubMed] [Google Scholar]
- 5. Gnass M, Sola J, Filarecka A, et al. Initial Polish experience of flexible 19 gauge endobronchial ultrasound-guided transbronchial needle aspiration. Adv Respir Med 85: 64-68, 2017. [DOI] [PubMed] [Google Scholar]
- 6. Tyan C, Patel P, Czarnecka K, et al. Flexible 19-G endobronchial ultrasound-guided transbronchial needle aspiration needle: first experience. Respiration 94: 52-57, 2017. [DOI] [PubMed] [Google Scholar]
- 7. Minami D, Takigawa N, Inoue H, et al. Rapid on-site evaluation with BIOEVALUATORⓇ during endobronchial ultrasound-guided transbronchial needle aspiration for diagnosing pulmonary and mediastinal diseases. Ann Thorac Med 9: 14-17, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Trisolini R, Natali F, Ferrari M, et al. Endobronchial ultrasound-guided transbronchial needle aspiration with the flexible 19-G needle. Clin Respir J 12: 1725-1731, 2018. [DOI] [PubMed] [Google Scholar]
- 9. Jeyabalan A, Bhatt N, Plummeridge MJ, et al. Adequacy of endobronchial ultrasound-guided transbronchial needle aspiration samples processed as histopathological samples for genetic mutation analysis in lung adenocarcinoma. Mol Clin Oncol 4: 119-125, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. van der Heijden EH, Casal RF, Trisolini R, et al. Guideline for the acquisition and preparation of conventional and endobronchial ultrasound-guided transbronchial needle aspiration specimens for the diagnosis and molecular testing of patients with known or suspected lung cancer. Respiration 88: 500-517, 2014. [DOI] [PubMed] [Google Scholar]
- 11. Stoy S, Lauren R, Septimiu M. The use of endobronchial ultrasound-guided transbronchial needle aspiration cytology specimens for programmed death ligand 1 immunohistochemistry testing in non-small cell lung cancer. J Bronchology Interv Pulmonol 24: 181-183, 2017. [DOI] [PubMed] [Google Scholar]
- 12. T Wahidi MM, Herth F, Yasufuku K, et al. Aspects of endobronchial ultrasound-guided transbronchial needle aspiration: CHEST guideline and expert panel report. Chest 149: 816-835, 2016. [DOI] [PubMed] [Google Scholar]
- 13. Sakamoto H, Kitano M, Komaki T, et al. Prospective comparative study of the EUS guided 25-G FNA needle with the 19-G Trucut needle and 22-G FNA needle in patients with solid pancreatic masses. J Gastroenterol Hepatol 24: 384-390, 2009. [DOI] [PubMed] [Google Scholar]
- 14. Nakai Y, Isayama H, Chang KJ, et al. Slow pull versus suction in endoscopic ultrasound-guided fine-needle aspiration of pancreatic solid masses. Dig Dis Sci 59: 1578-1585, 2014. [DOI] [PubMed] [Google Scholar]
- 15. Czarnecka-Kujawa K, Tremblay A, Yasufuku K, et al. A preclinical evaluation comparing the performance of a novel 19-g flexible needle to a commercially available 22-G EBUS-TBNA sampling needle. Respiration 95: 55-62, 2018(Epub ahead of print). [DOI] [PubMed] [Google Scholar]
- 16. Turell ME, Singh AD. Vascular tumors of the retina and choroid: diagnosis and treatment. Middle East Afr J Ophthalmol 17: 191-200, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
EBUS-TBNA, endobronchial ultrasound-guided transbronchial needle aspiration; LCNEC, large-cell neuroendocrine carcinoma; 19G, 19 gauge needle; 21G or 22G, 21 or 22 gauge needle; a Negative, not diagnosed pathologically.
The specimen obtained via endobronchial ultrasound-guided transbronchial needle aspiration using a 19-gauge needle contained adenocarcinoma cells more than 21-gauge needle (hematoxylin-eosin staining) (A), (B). Confirmation of PD-L1 expression (1–24% cells) in the 19-gauge needle material (PD-L1 tumor membrane staining, ×200) (C).