Abstract
Background and aim of the work: Fracture-dislocations of the proximal interphalangeal joint are complex injuries, often difficult to treat. Several treatment options have been described. Among them dynamic external fixation proved to be a safe technique leading to good results in many authors experience. The principles of this treatment are to avoid edema, prevent stiffness and tendon adhesions, promote joint remodelling and facilitate rehabilitation. The Ligamentotaxor® device is a simple and reproducible dynamic external fixation system that has been used in recent years to treat proximal interphalangeal joint fracture-dislocations, with favourable results. The aim of the present study is to evaluate our preliminary results with the Ligamentotaxor® device for treatment of these complex lesions. Methods: Four patients between December 2015 and January 2017 were treated at our institution with the Ligamentotaxor® device. Clinical and radiographic results were evaluated at mean 6 months follow-up. Results: Clinical results were meanly good and appeared to be comparable to most recent literature. Mean range of motion was 60,5°, mean extension lag 18,5°. Mean QuickDASH and Michigan Hand Questionnaire scored 21.6 and 72 respectively. Radiographic evaluation showed fracture healing in all cases. No relevant complications were noted. Conclusion: The Ligamentotaxor® device is simple to implant, provides good stability and allows an immediate gentle active movement. According to present work the preliminary results are encouraging. (www.actabiomedica.it)
Keywords: PIPfracture-dislocation, Ligamentotaxor®
Introduction
The PIP joint is a hinge joint normally stabilized by a “box” of soft tissues. The radial and ulnar collateral ligaments represent the box’s sides, the volar plate the box’s bottom and the central extensor slip the lid of the box (1, 2). When the disruption of one of these structures occur the stability of the joint is not compromised, while the disruption of at least two of these structures leads to dislocation (1). Dislocation may occur in volar, dorsal or lateral direction, with dorsal dislocation being the most common (1).
Fracture-dislocation of the proximal interphalangeal (PIP) joint is considered as a complicated dorsal dislocation and is recognized to be a complex injury often leading to poor outcome (3). Stiffness, pain and post traumatic arthritis are all common complications (4).
PIP joint dorsal fracture-dislocation have an estimated incidence of 9/100000 cases per year (5). PIP fracture-dislocations are commonly caused by hyperextension and axial loading of the joint resulting in impaction of the volar articular surface of the middle phalanx against the condyles of the proximal phalanx (6). Seno and colleagues classified these fractures in five types according to fracture site: in type 1 the fracture is on the palmar side; in type 2 the fracture is on the dorsal side; in type 3 fractures both volar and dorsal buttresses are compromised and the central part is depressed; type 4 is an extraarticular fracture; type 5 fractures occur on the sagittal plane (7). Type 3 fractures, also named PIP joint pilon fractures, occur when the finger is not hyperextended, the phalanges are collinear and an axial compressive force is applied. This fractures are associated to the worst outcome (8).
Conservative treatment with PIP joint immobilization may lead to a satisfying radiographic result, anyway firm tendon and periarticular adherences are unavoidable, with consequent relevant stiffness (9). Moreover, a reduction of range of motion of the injured joint is likely to occur even after a brief period of immobilization following internal fixation (4, 9-11). The aim of treatment is to avoid edema, prevent tendon adhesions and joint stiffness, promote joint remodeling and facilitate rehabilitation (10).
In order to choose the correct treatment the amount of intact joint surface and the stability of the fracture have both to be considered. If the fracture is considered stable a conservative treatment could be a good option. Some authors suggest more than 40% of articular surface involved to be an indication to surgical treatment (12). Other authors suggest that when 30% or less articular surface is involved the fracture should be considered stable, when more than 50% is involved it should be considered unstable and cases in-between these extremes are considered borderline and should be assessed carefully (13).
Diagnosis of these injuries is not always straightforward. Clinical presentation could be subtle. Plain radiographs are valuable to detect a complete dislocation, to quantify the extent of an eventual subluxation and to recognize avulsion fractures (2). On the other hand, subtle subluxation can be difficult to detect on standard radiographs. To identify these injuries, the clinician should look for the V-sign in lateral view, which represents the dorsal joint widening (Figure 1) (1).
Figure 1.

Radiographic exam in lateral view of ring finger, right hand. The V sign (white line) can be recognized, representing the joint dorsal widening associated to P2 fracture
When conservative treatment is indicated an extension block splinting may be the best choice, allowing for early mobilization of the joint without reaching complete extension (8).
Conversely, the best choice for surgical treatment is matter of debate. Surgical treatment options are several and include: open reduction and internal fixation, closed reduction and percutaneous fixation, volar plate arthroplasty and dynamic external fixation (14).
Dynamic external fixation has been described in literature, with reported satisfying results in terms of reduction, stabilization and early mobilization of PIP joint fractures (15). Distraction acts using ligamentotaxis to provide reduction, which is associated to good long term results especially thanks to the remodelling capacity of articular surface (15). The first dynamic external fixation device described in the literature was the banjo frame proposed by Schenk et al. in 1986 (16). Since then several devices were introduced until 1994 when Suzuki et al. (17) reported excellent results with a simple frame that allowed distraction and early mobilization. The Suzuki frame structure was made of Kirschner wires and rubber bands. To allow proper active motion of the PIP joint great importance resides in placing traction wire in the exact center of rotation of PIP joint at the proximal phalanx head. Moreover, as all controlled distraction procedures, the technique may be complex (18) and linked with the surgeon’s ability (19).
The Ligamentotaxor® device (Arex™, Palaiseau, France) (Figure 2) is based on the latter principles. The advantages of the device reside in the guided instrumentation that allows for easing the procedure and shortening the learning curve (10, 18). The device is made of Kirschner wires and plastic spherical joints that connect the wires with two metallic springs. The distraction can be precisely controlled trough the springs that can be screwed or unscrewed in order to increase or decrease the traction force.
Figure 2.

Clinical photograph of fifth finger, left hand, after Ligamentotaxor® application for PIP joint fracture-dislocation. The placement of the transverse Kirschner wires is made under fluoroscopy with the aid of a guiding device. After placing and modelling the K wires, spherical joints are placed and the metallic springs are screwed. The distraction obtained is controlled under fluoroscopy
The aim of the present work is to evaluate the clinical and radiographic preliminary results of PIP joint fracture-dislocations treatment with the Ligamentotaxor® device.
Methods
Form December 2015 to January 2017 4 cases of fracture-dislocation of the PIP joint were treated with the Ligamentotaxor® device at the Orthopaedics and Traumatology Unit of Cattinara Hospital-ASUITS of Trieste (Italy) in 4 patients. There were 3 male and 1 female, with mean age at the time of surgery of 49.5 years (range 42–62). Mean clinical and radiographic follow-up was 6 months (range 2–11). All fractures were classified according to Seno: two patients had a Seno type 1 fracture and two patients had a Seno type 3 fracture (pilon fracture). Patients underwent surgery meanly 6.5 days (range: 3–9) after trauma. Surgical treatment was performed under loco-regional anaesthesia and included closed reduction of dislocation and percutaneous application of the Ligamentotaxor® device under fluoroscopic control. In no case additional Kirschner wires were used to fix single bone fragments or to adjust the PIP joint alignment. All patients were allowed to start gentle active movement immediately after surgery. The Ligamentotaxor® frame was removed after 6 weeks in all cases.
Clinical evaluation at follow-up included the assessment of PIP joint range of motion (ROM), extension lag and total active movement (TAM). Pain during daily activities was measured with the VAS scale. Functional result was assessed by administering the QuickDASH score and the Michigan Hand Questionnaire. Time to return to normal activities including work was noted. Fracture healing and PIP joint alignment was evaluated on follow-up radiographic examination. Any complication including infection, non-union, persistent dislocation or reintervention was recorded. Present study results were compared to the literature.
Results and discussion
The mean range of motion of the PIP joint in the present study was 60,5° (range 40°-110°), with Seno type 3 patients having meanly poorer results (mean ROM 45°) (Table 1). The present study results concerning ROM are comparable to what reported in literature, both for the Ligamentotaxor® device and for other dynamic traction systems. In detail, Damert et al (9) reported a mean ROM of 73° (range 60°-100°) in 10 patients treated with the Ligamentotaxor® device. In the authors’ work only 2/10 patients (20%) suffered a Seno type 3 fracture. With the same device Pelissier et al. (18) reported a mean ROM of 81° (range: 0°-115°) in 88 patients. The same authors detected a meanly worse ROM value for pilon fractures, in which the mean ROM was 57°. Finally, Kortnig et al. and Colegate-Stone et al. reported a mean ROM of 76,3° (range 50°-120°) and 63° respectively (3, 10). In Colegate-Stone study only 1/12 patients suffered a pilon fracture. These results are also in line with what previously reported for other rubber and pins traction systems (8, 20-22).
Table 1.
Clinical results of the Seno 1 group compared with the Seno 3 group
| Seno 1 | Seno 3 | |
|---|---|---|
| ROM | 75 | 45 |
| Mean QuickDASH score | 19 | 24 |
| Mean extension lag | 16 | 21 |
| Mean pain (VAS score) | 2 | 2 |
In the present study the mean extension lag was 18,5°, with 2/4 patients (50%) reaching a complete extension of the PIP joint. Other authors reported similar results, with mean extension deficit between 11° (0°-45°) and 19,8° (0°-50°) (9, 10, 18).
The TAM mean value was 191,5° (range: 152–245) that according with the ASSH categories means an almost good result.
The mean VAS value for pain during daily activities was 2,2 (range 1–3). All patients experienced a persistent mild pain. The latter result is commonly reported in literature, being chronic persistent pain a sequela of complex fracture-dislocations of PIP joint in many authors experience (6, 18). Nonetheless, Kortnig et al. reported a mean VAS value for pain of 1,9 (range: 0–6), while Pelissier et al reported a persistent pain in 47% of patients (10, 18).
Functional results of the present study patients were meanly good and appeared to be comparable with the literature. All patients were able to return to their previous activities including work at mean 2,8 months (range: 2,5–3,5). The mean QuickDASH score was 21,6 (range 2,3–36.4) and the mean Michigan Hand Questionnaire outcome score was 72 (range 55–86). Other studies about the Ligamentotaxor® device reported QuickDASH mean values between 16,9 (0–43.18) and 9,1 (0–20,4) (3, 10).
At radiographic evaluation at follow-up all fractures healed, with only 1 case of articular surface depression and widening not negatively influencing clinical result (Case n°2). No cases of infection, nonunion or reintervention were registered. These data compare favourably to the literature where pin inflammation, infection and loosening are reported to be frequent complications, especially for the pin and rubber traction systems (6, 21-24). In fact, De Soras reported pin inflammation in 5/11 cases and pin loosening with osteolysis in 1/11 cases treated with the latter device (23). This has been suggested to be probably due to the mechanical stress in rotation to which the proximal pin is subjected. The theoretical advantage of the Ligamentotaxor® in this setting is that the plastic spherical joints absorbe the stress instead of the pins (10, 23), which may explain the low infection rate.
The only complication of the present study population was a minimal rotational defect in 1 case, which did not affect subjective and objective outcome.
Case n°1
A 50 years old female sustained a PIP joint fracture-dislocation of the ring finger of the right hand (Seno type 1). Seven days after the injury a Ligamentotaxor® device was applied. She started immediately active motion of the finger. After 6 weeks the device was removed. Four months after surgery follow-up radiographs showed healing of the fracture and restoration of the articular surface. Clinical results were excellent: PIP joint ROM was 110° with complete extension of the finger. The VAS for pain was 1, the QuickDASH score was 2,3 and the Michigan Hand Questionnaire outcome was 86. There were no rotational defects (Figure 3).
Figure 3.
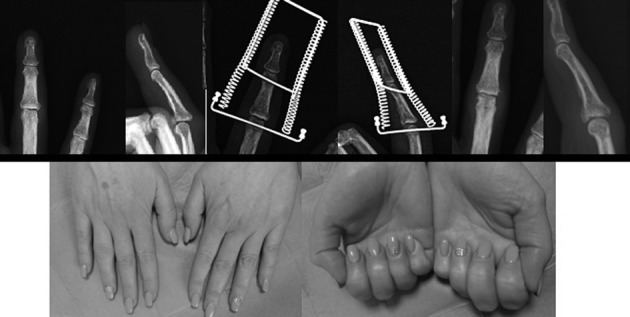
Clinical case n°1: The figure shows on top, from left to right, the trauma x-rays showing a Seno type 1 fracture of the ring finger (left), post-operative x-rays showing the Ligamentotaxor® in place with the amount of distraction and reduction applied (center) and follow-up x-rays at 4 months, showing fracture healing and initial joint remodelling (right). On the bottom the clinical outcome with ROM in extension (left) and flexion (right)
Case n°2
A 44 years-old heavy worker male patient reported a pilon fracture (Seno type 3) of the fifth finger of the right hand during a road traffic accident. Three days after a Ligamentotaxor® was applied and was removed after 6 weeks. Despite articular surface depression and widening at follow up x-rays the functional outcome was good: the range of motion was 60° with complete extension of the proximal interphalangeal joint, the QuickDASH score was 11,4, the Michigan Hand Questionnaire outcome was 82 and the VAS value for pain was 3. The patient returned to heavy hand working 3 months after surgery (Figure 4).
Figure 4.
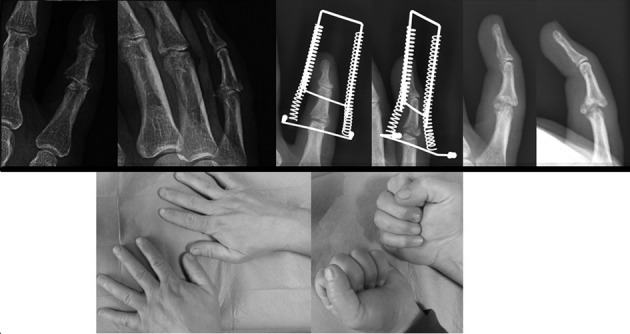
Clinical case n°2: The figure shows on top, from left to right, the trauma x-rays showing a Seno type 3 fracture of the fifth finger (left), post-operative x-rays showing the Ligamentotaxor® in place with the amount of distraction and reduction applied (center) and follow-up x-rays at 6 months, showing fracture healing resulted in articular surface depression and widening (right). On the bottom the good clinical outcome despite radiographic result with ROM in extension (left) and flexion (right).
Conclusions
The results of the present work are encouraging and seem to confirm the good results reported in literature for the Ligamentotaxor® device. In our experience the device proved to be simple to apply and reliable in outpatient management. It allows for an early and safe active mobilization of the PIP joint leading to good results even in case of radiographic unfair outcome, at least at short term follow-up. We recommend the use of dynamic external fixation to treat the dorsal fracture dislocation of the PIP joint.
References
- 1.Haase SC, Chung KC. Invited Hand Article: Current Concepts in Treatment of Fracture-Dislocations of the Proximal Interphalangeal Joint. Plast Reconstr Surg. 2014;134(6):1246–57. doi: 10.1097/PRS.0000000000000854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Freiberg A. Management of proximal interphalangeal joint injuries. Can J Plast Surg. 2007;15(4):199–203. doi: 10.1177/229255030701500407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Colegate-Stone T, Marenah K, Compson J, Tahmassebi R, Tavakkolizadeh A. Functional outcomes following pilon fractures of the middle phalanx managed with the Ligamentotaxor® external fixator. Hand Surg. 2015;20(02):285–9. doi: 10.1142/S0218810415500252. [DOI] [PubMed] [Google Scholar]
- 4.Badia A, Riano F, Ravikoff J, Khouri R, Gonzalez-Hernandez E, Orbay JL. Dynamic intradigital external fixation for proximal interphalangeal joint fracture dislocations. J Hand Surg Am. 2005;30(1):154–60. doi: 10.1016/j.jhsa.2004.07.019. [DOI] [PubMed] [Google Scholar]
- 5.Weiss APC. Cerclage fixation for fracture dislocation of the proximal interphalangeal joint. Clin Orthop Relat Res. 1996;327:21–8. doi: 10.1097/00003086-199606000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Bain GI, Mehta JA, Heptinstall RJ, Bria M. Dynamic external fixation for injuries of the proximal interphalangeal joint. J Bone Joint Surg Br. 1998;80(6):1014–9. doi: 10.1302/0301-620x.80b6.8030. [DOI] [PubMed] [Google Scholar]
- 7.Seno, Hashizume, Inoue, Imatani, Morito Fractures of the base of the middle phalanx of the finger. J Bone Joint Surg Br. 1997;79(5):758–63. doi: 10.1302/0301-620x.79b5.7664. [DOI] [PubMed] [Google Scholar]
- 8.Syed AA, Agarwal M, Boome R. Dynamic external fixator for pilon fractures of the proximal interphalangeal joints: a simple fixator for a complex fracture. J Hand Surg Br. 2003;28(2):137–41. doi: 10.1016/s0266-7681(02)00300-5. [DOI] [PubMed] [Google Scholar]
- 9.Damert HG, Altmann S, Kraus A, Infanger M, Sattler D. Treatment of intraarticular middle phalanx fractures using the Ligamentotaxor®. Hand. 2013;4:460–3. doi: 10.1007/s11552-013-9553-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Körting O, Facca S, Diaconu M, Liverneaux P. Treatment of complex proximal interphalangeal joint fractures using a new dynamic external fixator: 15 cases. Chir Main. 2009;28(3):153–7. doi: 10.1016/j.main.2009.03.001. [DOI] [PubMed] [Google Scholar]
- 11.Maalla R, Youssef M, Jdidia GB, Khimiri C, Essadam H. Extension-block pinning for fracture-dislocation of the proximal interphalangeal joint. Orthop Traumatol Surg Res. 2012;98(5):559–63. doi: 10.1016/j.otsr.2012.02.009. [DOI] [PubMed] [Google Scholar]
- 12.Green DP, Hotchkiss RN, Pederson WC, editors. Green’s Operative Hand Surgery. 5th ed. New York: Churchill Livingstone; 2011. [Google Scholar]
- 13.Mcelfresh EC, Dobyns JH, O’brien ET. Management of fracture-dislocation of the proximal interphalangeal joints by extension-block splinting. J Bone Joint Surg Am. 1972;54(8):1705–11. [PubMed] [Google Scholar]
- 14.Ruland RT, Hogan CJ, Cannon DL, Slade JF. Use of dynamic distraction external fixation for unstable fracture-dislocations of the proximal interphalangeal joint. J Hand Surg Am. 2008;33(1):19–25. doi: 10.1016/j.jhsa.2007.07.018. [DOI] [PubMed] [Google Scholar]
- 15.Kiral A, Erken HY, Akmaz I, Yildirim C, Erler K. Pins and rubber band traction for treatment of comminuted intra-articular fractures in the hand. J Hand Surg. 2014;39(4):696–705. doi: 10.1016/j.jhsa.2013.12.038. [DOI] [PubMed] [Google Scholar]
- 16.Schenck RR. Dynamic traction and early passive movement for fractures of the proximal interphalangeal joint. J Hand Surg. 1986;11(6):850–8. doi: 10.1016/s0363-5023(86)80236-2. [DOI] [PubMed] [Google Scholar]
- 17.Suzuki Y, Matsunaga T, Sato S, Yokoi T. The pins and rubbers traction system for treatment of comminuted intraarticular fractures and fracture-dislocations in the hand. J Hand Surg Br. 1994;19(1):98–107. doi: 10.1016/0266-7681(94)90059-0. [DOI] [PubMed] [Google Scholar]
- 18.Pélissier P, Gobel F, Choughri H, Alet JM. Proximal interphalangeal joint fractures treated with a dynamic external fixator: A multicenter and retrospective study of 88 cases. Chir Main. 2015;34(5):245–50. doi: 10.1016/j.main.2015.08.002. [DOI] [PubMed] [Google Scholar]
- 19.Debus G, Courvoisier A, Wimsey S, Pradel P, Moutet F. Pins and rubber traction system for intra-articular proximal interphalangeal joint fractures revisited. J Hand Surg Eur. 2010;35(5):396–401. doi: 10.1177/1753193409359493. [DOI] [PubMed] [Google Scholar]
- 20.El Khatib K, Kadlub N, Trost O, Danino AM, Malka G. Dynamic external traction system for management of distal displaced fractures of the head of the proximal phalanx. Chir Main. 2007;26(1):21–5. doi: 10.1016/j.main.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 21.Krakauer JD, Stern PJ. Hinged device for fractures involving the proximal interphalangeal joint. Clin Orthop Relat Res. 1996;327:29–37. doi: 10.1097/00003086-199606000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Schenck RR. The dynamic traction method. Combining movement and traction for intra-articular fractures of the phalanges. Hand Clin. 1994;10:187–98. [PubMed] [Google Scholar]
- 23.Soras X, Mourgues P, Guinard D, Moutet F. Pins and rubbers traction system. The Journal of Hand Surgery: British & European Volume. 1997;22(6):730–5. doi: 10.1016/s0266-7681(97)80435-4. [DOI] [PubMed] [Google Scholar]
- 24.Theivendran K, Pollock J, Rajaratnam V. Proximal interphalangeal joint fractures of the hand: treatment with an external dynamic traction device. Annals of plastic surgery. 2007;58(6):625–9. doi: 10.1097/01.sap.0000245132.14908.9d. [DOI] [PubMed] [Google Scholar]


