Supplemental Digital Content is available in the text
Keywords: anaphylaxis, community, epidemiology, incidence, republic of Korea, trigger
Abstract
Anaphylaxis can cause death and requires immediate management. For prevention and education programs for anaphylaxis, it is important to be aware of the common triggering factors. We investigated the triggers of anaphylaxis in the emergency departments (EDs) of community hospitals in Korea.
Patients who visited the EDs of 7 community hospitals for anaphylaxis from January 1, 2012 to December 31, 2016 were enrolled. Anaphylaxis was defined according to the World Allergy Organization criteria and identified via a thorough review of the medical records of patients who were diagnosed with anaphylaxis (ICD-10 codes: T780, T782, T805, and T886) at the ED or administered epinephrine in the ED. Triggers of anaphylaxis were also evaluated by a review of the medical records.
We identified 1021 ED visits for anaphylaxis. The incidence of anaphylaxis ED visits was 0.08%. The triggers of ED visits for anaphylaxis were bee venom (55.0%), foods (21.3%), and drugs (13.2%); 9.6% of cases were idiopathic. However, food was the most common trigger among the patients aged <20 years old. The frequency of ED visits for anaphylaxis was highest in summer (47.9%), followed by autumn (28.2%), spring (12.3%), and winter (11.6%). The incidence of anaphylaxis ED visits was highest in August, during which bee venom was the trigger for 80% of anaphylaxis cases. For the 55 patients with repeat ED visits for anaphylaxis, Bee venom was also the most common trigger.
The number of ED visits for anaphylaxis showed marked seasonal variation, peaking in summer. Bee venom was the most common trigger for adults and the main reason for seasonal variations of anaphylaxis ED visits in Korean community hospitals.
1. Introduction
Anaphylaxis is a life-threatening generalized hypersensitivity reaction,[1] with an incidence of 0.01% to 0.03%,[2] and this rate is increasing.[3,4] Anaphylaxis must be recognized early and treated immediately. Awareness of the common triggers is also important to prevent anaphylaxis.
Anaphylaxis can be triggered by diverse factors.[5–8] There have been several studies about the triggers for anaphylaxis in Korea and all of those studies were conducted in tertiary university hospitals.[6,9] Since the patients of tertiary university hospitals are usually highly selected and referred patients from community hospitals, it is doubtful whether those studies could reflect the truth for general population in the Korean community. Furthermore, no study has assessed the triggers of anaphylaxis and their seasonal changes in Korea,[10] although Korea has 4 distinct seasons with marked seasonal changes in weather, food for the season, and lifestyle. And thus studies about epidemiology and common triggers for anaphylaxis based on community hospitals are needed in Korea.
We investigated the common triggers of anaphylaxis in 7 Korean community hospitals by retrospective review of the medical records for the patients who visited the emergency departments (EDs) for anaphylaxis from 2012 to 2016.
2. Materials and methods
2.1. Study design and data collection
Patients who visited the EDs of 7 hospitals from January 2012 to December 2016 were enrolled. The medical records of ED patients diagnosed with anaphylaxis by the ICD-10 codes (T780, T782, T805, and T886) or of patients who were administered epinephrine at EDs were reviewed by a well-trained ED doctor of each hospital. And a pediatrician reviewed again to validate the collected data. Cases in which the anaphylaxis could not be clearly identified were excluded (Fig. 1). Anaphylaxis was defined according to the European Academy of Allergy and Clinical Immunology.[11]
Figure 1.
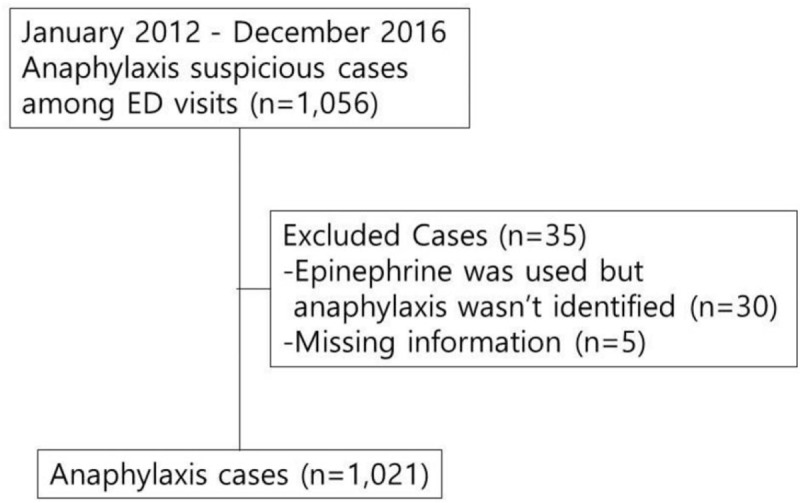
Eligible case enrolled in study.
Among government-operated hospitals which were asked to participate in this study, the 7 government-operated hospitals voluntarily participated in this study. Five hospitals were located in rural area and 2 hospitals were located in the urban area (Supplement Figure). EDs of government-operated hospitals cover the large part of the Korean community with a similar system in electronic medical record, order communication system, and patient management program. Six of these hospitals are the only institution with an ED in their administrative district. The annual incidence of anaphylaxis ED visits was estimated for these 6 areas by dividing the number of anaphylaxis ED visits by the number of residents reported by the National Statistical Office in that year. The incidence by age group was also calculated using the total number of persons in that age group registered by the National Statistical Office and the number of individuals in these areas who visited an ED for anaphylaxis.
Patients were grouped into 10 years old. The trigger of anaphylaxis was specified only when clearly described in the medical records. To exclude errors caused by a delayed response, the trigger was defined within 8 hours of symptom onset.[9] Triggers of anaphylaxis were classified as bee venom, foods (seafood, meat, vegetable, fruit, wheat, buckwheat, alcohol, nut products, other, unknown), drugs (non-steroidal anti-inflammatory drugs [NSAIDs], antibiotics, antibiotics and NSAIDs, acetaminophen, radiocontrast media, other), other insects, and idiopathic triggers. Anaphylaxis in patients simultaneously exposed to various triggers, or that for which the trigger could not be identified, was considered idiopathic. Regarding drugs, “cold medicine” in the medical records was classified as other drugs. We investigated anaphylaxis ED visits according to sex, age, trigger, and season. The triggers of anaphylaxis were analyzed monthly and by season: spring (March to May), summer (June to August), autumn (September to November), and winter (December to February).[10] The number of epinephrine auto-injector (EAI) prescriptions in the ED was also evaluated.
2.2. Statistical analysis
The mean age of the patients was evaluated by one-way analysis of variance. The frequencies of anaphylaxis triggers by season were analyzed by chi-squared test. Multiple logistic regression analysis of 4 common triggers was performed with adjustments for age, sex, and season. A P-value of <.05 was considered indicative of statistical significance. Statistical analyses were performed using SPSS for Windows ver. 20.0 (SPSS, Chicago, IL).
2.3. Ethical consideration
The study was approved by the Kangwon University Hospital Institutional Review Board and the ethics board of each participating institution. No patient informed consent was obtained, as it was a secondary analysis from medical records.
3. Results
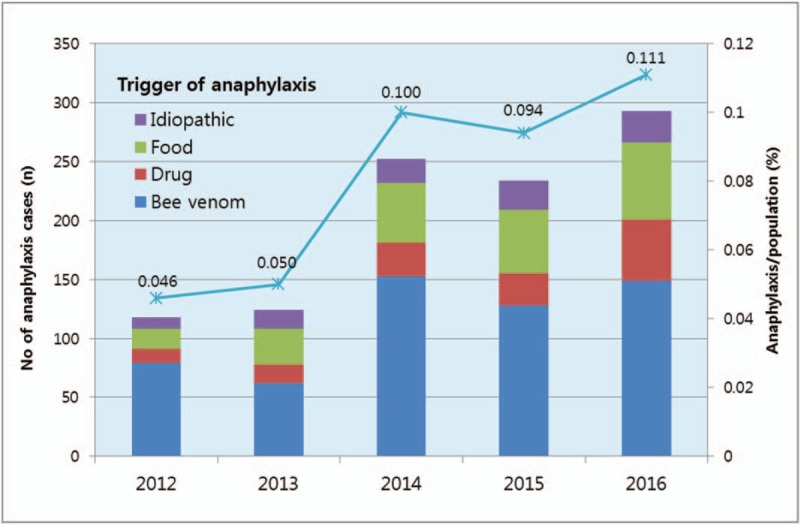
A total of 325,857 ED visits occurred during the study period, of which 1021 were for anaphylaxis (65% males, mean age 51.5 ± 16 years) (Table 1). Bee venom (55.0%) was the most common trigger, followed by foods (21.3%) and drugs (13.2%). Among the trigger foods, seafood was the most common (79/217, 36.4%; Fig. 2). A few cases in which grasshopper, pupae, frogs, and mushrooms were suspected of trigger food were classified as “other” in Figure 2. For the trigger medications, NSAIDs and antibiotics were the most common triggers of drug-induced anaphylaxis, whereas the causative drug was unknown in 46.7% (63/135) of cases according to ED medical records.
Table 1.
Characteristics of the cases.
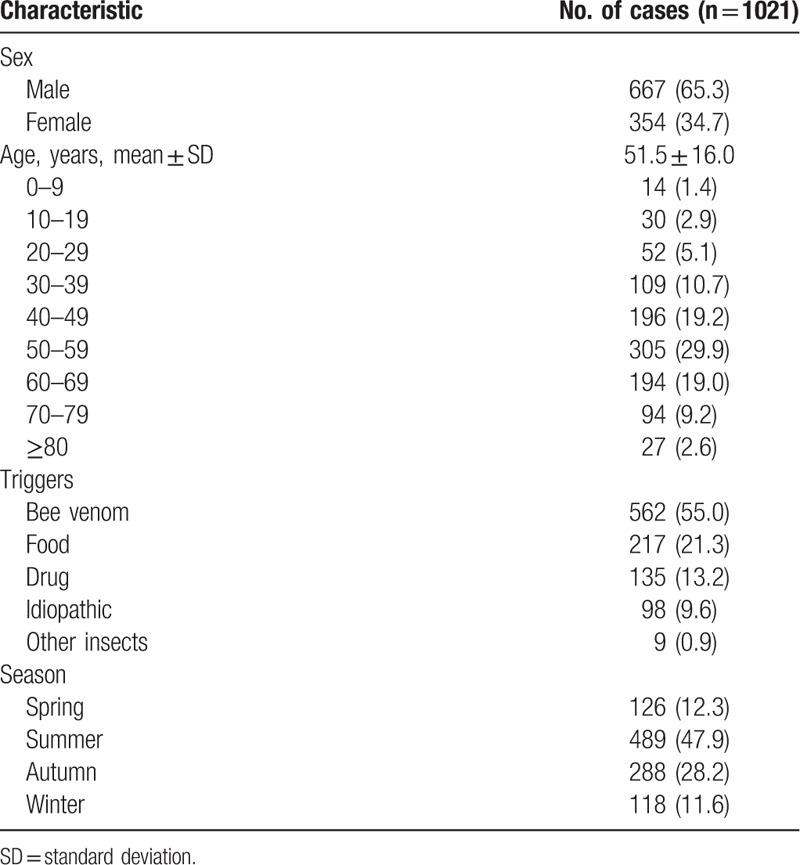
Figure 2.
Triggers of anaphylaxis resulting in an ED visit.
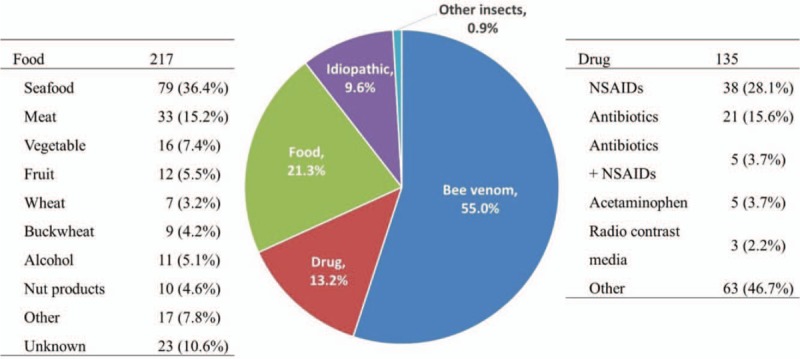
The number of ED visits for anaphylaxis increased during the study period, with an increase in the annual incidence from 0.045% in 2012 to 0.11% in 2016 (P < .001; Fig. 3). The frequency of ED visits for anaphylaxis showed marked seasonal variation (Fig. 4) and was highest in summer (n = 489, 47.9%; Table 1). The major cause of this seasonal variation was bee venom-induced anaphylaxis, which occurred from April to November with a peak in August, accounting for 80% of ED visits for anaphylaxis during that month. The frequency of ED visits for food-induced anaphylaxis seemed to be higher in January, June, and September, and that of drug-induced anaphylaxis seemed to be higher in February, July, and September. However, the distribution of causative foods and drugs did not differ by month.
Figure 3.
Annual change in the number of anaphylaxis ED visits and annual incidence of anaphylaxis ED visits.
Figure 4.
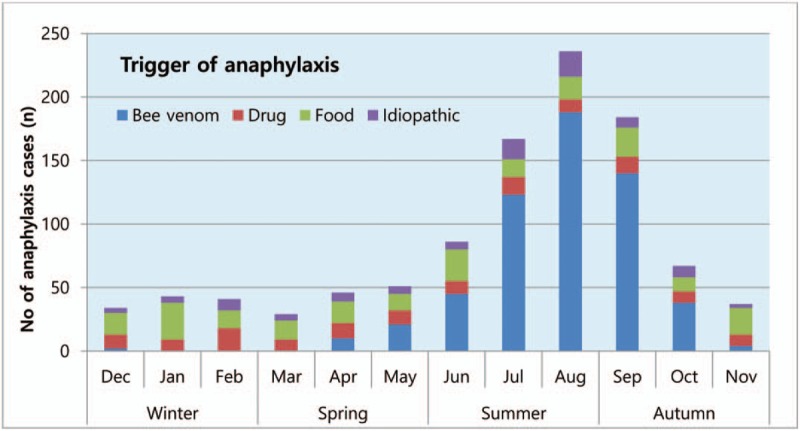
Number of anaphylaxis ED visits by month during 2012–2016 (n = 1,021). The number of ED visits for anaphylaxis caused by bee venom varied by month (P < 0.001).
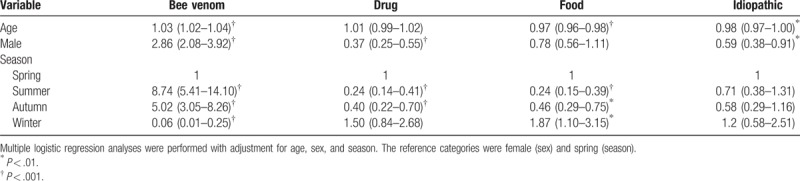
Food was the most common trigger among patients aged <20 years old (Fig. 5). The profiles of the trigger food seemed different between the patients aged <20 years old and those aged ≥20 years old (Fig. 6). The frequency of ED visits for bee venom- and food-induced anaphylaxis was highest in the 50 to 59-year age group. The frequency of ED visits for drug-induced anaphylaxis was highest in the 60 to 69-year age group (Fig. 5). Multiple logistic regression analysis revealed that the probability of ED visits for bee venom-induced anaphylaxis was associated with older age, male sex, and summer (Table 2). The frequency of ED visits for food anaphylaxis decreased with age and was higher in winter. The frequency of ED visits for drug-induced anaphylaxis was higher in females and lower in summer and autumn.
Figure 5.
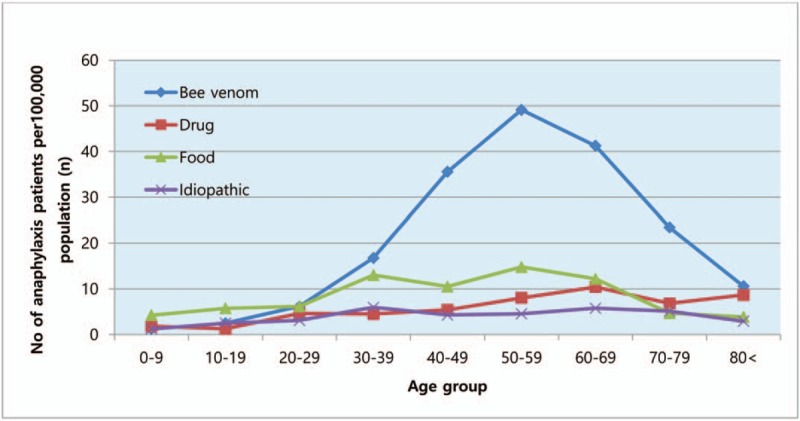
Age distribution according to the trigger of anaphylaxis (2012–2016). ‘Other insects’ is not shown because of the small number of cases.
Figure 6.
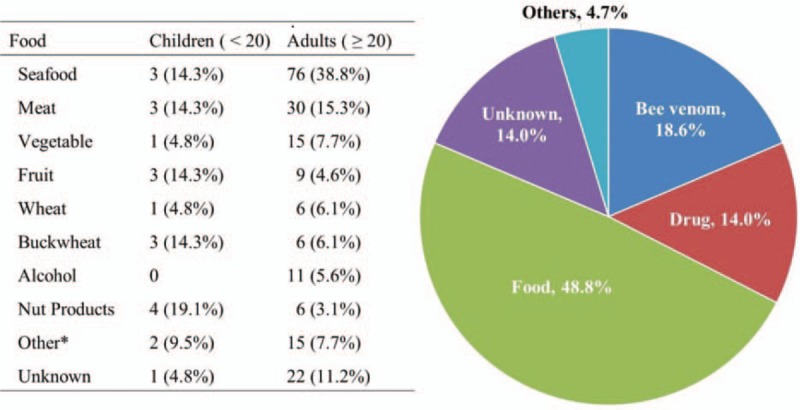
Triggers of anaphylaxis ED visits in patients <20 years old. (right). Comparison of triggers with <20 years old and ≥20 years old, in food anaphylaxis cases (left).
Table 2.
Multiple logistic regression analyses of the triggers of anaphylaxis.
Fifty-five patients had more than 1 episode of anaphylaxis, accounting for a total of 131 ED visits (12.8%). The average number of ED visits per person was 2.4. Repeat ED visits for anaphylaxis involved the same trigger in 30 patients (54.5%), a different trigger in 13 patients (23.6%), and was idiopathic in 12 patients (21.8%). Among the triggers of repeat ED visits for anaphylaxis, bee venom accounted for 58 cases (44.3%), food for 30 cases (22.9%), and drugs for 19 cases (14.5%; Fig. 7). The frequency of repeat ED visits for anaphylaxis was highest in the 60 to 69-year age group.
Figure 7.
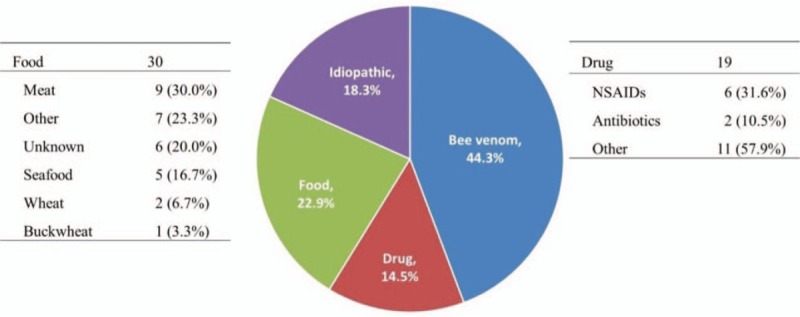
Triggers of anaphylaxis resulting in repeat ED visits (center). Detailed triggers of drug anaphylaxis (right), food anaphylaxis (left), in repeat ED visit cases.
There were no deaths associated with anaphylaxis among the all enrolled patients who visited ED for anaphylaxis during study periods. Otherwise, EAI was not prescribed in any case.
4. Discussion
The number of ED visits for anaphylaxis showed marked seasonal variation in this study. Bee sting was not only the most common trigger but also the main reason for the seasonal variation in the frequency of ED visits for anaphylaxis. The incidence of bee venom-induced anaphylaxis is highest in August and among middle-aged males. Foods and drugs were the next most frequent triggers of anaphylaxis. However, for young patients aged <20 years old, food was the most common trigger for anaphylaxis resulting in ED visits.
Bee sting was the most common trigger of ED visits for anaphylaxis and food was the most common trigger among young patients who visited ED for anaphylaxis in Korean community hospitals in this study. In contrast, previous epidemiological studies based on tertiary university hospitals in Korea reported that drugs (47%) were the most common triggers of anaphylaxis, with bee venom accounting for only about 16% of cases.[6,9,10,12] The differences in the results between our and previous studies in Korea may be due to differences in the enrolled hospitals, community hospitals versus tertiary referral hospitals, which could reflect different patient communities. Similar tendency in difference of the common triggers for anaphylaxis seemed to be observed in previous studies: Treudler et al reported that drugs (46%), bee venom (33%), and foods (11%) were the most common triggers at university hospitals in Germany.[5] In contrast, bee venom (32%) was the most common cause of anaphylaxis in the United Kingdom based on the medical records of general physicians, followed by drugs (30%) and foods (22%).[7] And a Swiss study based on the medical records of 17 regional hospitals reported that bee venom (59%), drugs (18%), and foods (10%) were the most common triggers.[8] Furthermore, this study showed marked seasonal variations in anaphylaxis mainly due to bee venom-induced anaphylaxis. Although several previous studies also reported seasonal variations in the incidence of anaphylaxis,[13,14] seasonal variations in this study is most pronounced and this may be because Korea has 4 distinct seasons. Therefore, this study suggests that epidemiological studies of anaphylaxis should be performed over at least 1 year to cover possible seasonal variations, and prevention and educational programs for anaphylaxis should be tailored to the particular community.
Common triggers for anaphylaxis ED visits were different between young patients (<20 years old) and adult patients (≥20 years old). Food was the most common trigger for young patients and the profiles of causative foods were also different between 2 groups, although the number of young patients was small: nut products seemed more common triggering food in the young population. These results are consistent with findings of the previous study about anaphylaxis-related hospitalizations in UK that common triggers were different according to the age group and food was most common trigger of anaphylaxis in children with nut product accounting for 48% of causes of fatal food-induced anaphylaxis cases.[15]
There have been several studies reported much higher rates of repeat ED visits for anaphylaxis (27.0%[16] and 42.8%[17]). Both of these studies involved a questionnaire survey of patients with a history of anaphylaxis, and foods were the most common triggers in these previous reports.[16,17] On the other hand, repeat ED visits accounted for 12.8% of the total ED visits for anaphylaxis in the present study and more than 50% of cases of them had the same trigger for each ED visit for anaphylaxis, most commonly bee-sting. However, no EAIs were prescribed in the EDs during the study period even though bee venom was the most common trigger of anaphylaxis resulting in single and repeat ED visits. In addition, the causative drug remained unidentified in the medical records of 46.7% of the patients with drug-induced anaphylaxis. Considering that EAI prescription in ED or primary care settings is recommended after acute anaphylaxis and identification of the causative medication and provision of an alternative are important for patients with anaphylaxis,[18] these findings suggest that EAI prescription in ED should be emphasized more for ED doctors and that an education program to reduce the recurrence of anaphylaxis and to evaluate its causes should be emphasized in the EDs of community hospitals in Korea.
There were some relationships among age, gender, and the triggers for anaphylaxis in this study. Bee venom-induced anaphylaxis was common in middle-aged males in this study, which is in agreement with a previous multicenter study of ED visits for insect venom allergies in North America.[19] Drug-induced anaphylaxis occurred predominantly in females for unknown reasons in this study. Liew et al[20] reported that more female than male subjects ≥15 years old were admitted for drug-induced anaphylaxis in Australia. Regarding drugs, NSAIDs and antibiotics were also common triggers of anaphylaxis in other studies.[10,20] Although the foods that trigger anaphylaxis vary regionally, seafood has been consistently reported as a frequent trigger of anaphylaxis.[15,20] And nut products were the most common triggering of food anaphylaxis in children.[15,21] Present study also showed the increase of ED visits for anaphylaxis in Korea, which is consistent with previous reports that prevalence rates of anaphylaxis have increased in recent years worldwide,[3,22–25] and in Korea.[26,27] Although it may need more studies to understand the reason why incidence of anaphylaxis increase, changes in environments and lifestyle, and increase of awareness about anaphylaxis might be one of the reasons for increase ED visits for anaphylaxis.
This study has limitations that should be discussed. First, because this was a retrospective study, it may have been influenced by selection bias. Large prospective epidemiologic studies are thus needed to assess the incidence and causes of anaphylaxis. Second, the proposed disease codes of anaphylaxis alone are likely to result in missing patients. Choi et al[28] reported, in the case of anaphylaxis, a lot of patients were registered inaccurate disease codes and epinephrine treatment was a factor associated with accurate registration with anaphylaxis disease codes in patients with anaphylaxis. So we reviewed all patients who were administered epinephrine in the EDs. Third, it is possible that all necessary data was not obtained from all patients due to differences in the fidelity of the medical records among the hospitals, which may affect the reliability of the results. However, all ED medical records provided the necessary information. One experienced pediatrician reviewed all medical records of patients diagnosed with anaphylaxis or who were administered epinephrine in the ED.
In conclusion, this is the first study of anaphylaxis in the EDs of Korean community hospitals. The triggers of anaphylaxis could be different according to the level of hospitals, targeted communities, and age. Bee venom was the most common trigger for adults and the main reason for seasonal variations of anaphylaxis ED visits in Korean community hospitals. Prevention and education programs for anaphylaxis should be tailored to the community in question and should take into account seasonal variations in the triggering factors.
Author contributions
Conceptualization: Hyunseok Cho.
Data curation: Hyunseok Cho, Dohyun Kim, Youngkwang Choo, Jungseok Park, Jangwon Choi, Dongwhan Jang, Taekwon Kim.
Formal analysis: Hyunseok Cho.
Investigation: Hyunseok Cho, Dohyun Kim, Youngkwang Choo, Jungseok Park, Jangwon Choi, Dongwhan Jang, Taekwon Kim.
Methodology: Hyunseok Cho.
Project administration: Hyunseok Cho.
Supervision: Hyunseok Cho, Jae Won Jeong, Jae-Woo Kwon.
Visualization: Hyunseok Cho.
Writing – original draft: Hyunseok Cho, Jae Won Jeong.
Writing – review and editing: Hyunseok Cho, Jae Won Jeong, Jae-Woo Kwon.
Hyunseok Cho orcid: 0000-0002-3105-4680.
Supplementary Material
Footnotes
Abbreviation: ED = emergency department.
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (NRF-2017R1D1A3B03034684).
The authors report no conflicts of interest.
Supplemental Digital Content is available for this article.
References
- [1].Simons FE, Ardusso LR, Bilo MB, et al. Update: World Allergy Organization Guidelines for the assessment and management of anaphylaxis. Curr Opin Allergy Clin Immunol 2012;12:389–99. [DOI] [PubMed] [Google Scholar]
- [2].Moneret-Vautrin D, Morisset M, Flabbee J, et al. Epidemiology of life-threatening and lethal anaphylaxis: a review. Allergy 2005;60:443–51. [DOI] [PubMed] [Google Scholar]
- [3].Decker WW, Campbell RL, Manivannan V, et al. The etiology and incidence of anaphylaxis in Rochester, Minnesota: a report from the Rochester epidemiology project. J Allergy Clin Immunol 2008;122:1161–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Sheikh A, Hippisley-Cox J, Newton J, et al. Trends in national incidence, lifetime prevalence and adrenaline prescribing for anaphylaxis in England. J R Soc Med 2008;101:139–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Treudler R, Kozovska Y, Simon J. Severe immediate type hypersensitivity reactions in 105 German adults: when to diagnose anaphylaxis. J Investig Allergol Clin Immunol 2008;18:52–8. [PubMed] [Google Scholar]
- [6].Ye Y-M, Kim MK, Kang H-R, et al. Predictors of the severity and serious outcomes of anaphylaxis in Korean adults: a multicenter retrospective case study. Allergy Asthma Immunol Res 2015;7:22–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Peng MM, Jick H. A population-based study of the incidence, cause, and severity of anaphylaxis in the United Kingdom. Arch Intern Med 2004;164:317–9. [DOI] [PubMed] [Google Scholar]
- [8].Helbling A, Hurni T, Mueller U, et al. Incidence of anaphylaxis with circulatory symptoms: a study over a 3-year period comprising 940 000 inhabitants of the Swiss Canton Bern. Clin Exp Allergy 2004;34:285–90. [DOI] [PubMed] [Google Scholar]
- [9].Yang M-S, Lee S-H, Kim T-W, et al. Epidemiologic and clinical features of anaphylaxis in Korea. Ann Allergy Asthma Immunol 2008;100:31–6. [DOI] [PubMed] [Google Scholar]
- [10].Lee Y-K, Kim MK, Kang H-R, et al. Seasonal and regional variations in the causes of anaphylaxis in Korean adults. Allergy Asthma Respir Dis 2015;3:187–93. [Google Scholar]
- [11].Muraro A, Roberts G, Worm M, et al. Anaphylaxis: guidelines from the European Academy of Allergy and Clinical Immunology. Allergy 2014;69:1026–45. [DOI] [PubMed] [Google Scholar]
- [12].Lee S-K, Ye Y-M, Park H-S, et al. Hymenoptera venom anaphylaxis in adult Korean: a multicenter retrospective case study. Allergy Asthma Respir Dis 2014;2:344–51. [Google Scholar]
- [13].Harduar-Morano L, Simon MR, Watkins S, et al. A population-based epidemiologic study of emergency department visits for anaphylaxis in Florida. J Allergy Clin Immunol 2011;128:594–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Simon MR, Mulla ZD. Hospitalizations for anaphylaxis in Florida: analysis of month of discharge. Int Arch Allergy Immunol 2008;146:89–90. [DOI] [PubMed] [Google Scholar]
- [15].Turner PJ, Gowland MH, Sharma V, et al. Increase in anaphylaxis-related hospitalizations but no increase in fatalities: an analysis of United Kingdom national anaphylaxis data, 1992–2012. J Allergy Clin Immunol 2015;135:956–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Mehl A, Wahn U, Niggemann B. Anaphylactic reactions in children–a questionnaire-based survey in Germany. Allergy 2005;60:1440–5. [DOI] [PubMed] [Google Scholar]
- [17].Mullins R. Anaphylaxis: risk factors for recurrence. Clin Exp Allergy 2003;33:1033–40. [DOI] [PubMed] [Google Scholar]
- [18].Ewan P, Brathwaite N, Leech S, et al. BSACI guideline: prescribing an adrenaline auto-injector. Clin Exp Allergy 2016;46:1258–80. [DOI] [PubMed] [Google Scholar]
- [19].Clark S, Long AA, Gaeta TJ, et al. Multicenter study of emergency department visits for insect sting allergies. J Allergy Clin Immunol 2005;116:643–9. [DOI] [PubMed] [Google Scholar]
- [20].Liew WK, Williamson E, Tang ML. Anaphylaxis fatalities and admissions in Australia. J Allergy Clin Immunol 2009;123:434–42. [DOI] [PubMed] [Google Scholar]
- [21].Motosue MS, Bellolio MF, Van Houten HK, et al. National trends in emergency department visits and hospitalizations for food-induced anaphylaxis in US children. Pediatr Allergy Immunol 2018. [DOI] [PubMed] [Google Scholar]
- [22].Parlaman JP, Oron AP, Uspal NG, et al. Emergency and hospital care for food-related anaphylaxis in children. Hosp Pediatr 2016;6:1–6. [DOI] [PubMed] [Google Scholar]
- [23].Michelson KA, Monuteaux MC, Neuman MI. Variation and trends in anaphylaxis care in United States children's hospitals. Acad Emerg Med 2016;23:623–7. [DOI] [PubMed] [Google Scholar]
- [24].Diwakar L, Cummins C, Ryan R, et al. Prescription rates of adrenaline auto-injectors for children in UK general practice: a retrospective cohort study. Br J Gen Pract 2017;67:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Sheikh F, Amin R, Rehan Khaliq AM, et al. First study of pattern of anaphylaxis in a large tertiary care hospital in Saudi Arabia. Asia Pac Allergy 2015;5:216–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Jeong K, Lee J-D, Kang DR, et al. A population-based epidemiological study of anaphylaxis using national big data in Korea: trends in age-specific prevalence and epinephrine use in 2010–2014. Allergy, Asthma & Clinical Immunology 2018;14:31–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Yang M-S, Kim J-Y, Yang M-S, Kim J-Y, Kim B-K, et al. True rise in anaphylaxis incidence: Epidemiologic study based on a national health insurance database. Medicine 2017;96:5–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Choi B, Kim SH, Lee H. Are registration of disease codes for adult anaphylaxis accurate in the emergency department? Allergy Asthma Immunol Res 2018;10:137–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


